MRI diagnosis of synovial folds of the knee joint
Filisteev Pavel Anatolyevich, head of the MRI department of the MED-7 diagnostic center, doctor of the X-ray diagnostics and tomography department of the Federal State Budgetary Institution "Central Clinical Hospital with Clinic" of the Administration of the President of the Russian Federation
Synovial folds of the knee joint are part of the normal anatomy of the knee joint and can sometimes cause clinical manifestations. Magnetic resonance imaging (MRI) and MR arthrography allow non-invasive assessment of the condition of synovial folds and differential diagnosis of the cause of pain in the knee joint. Synovial folds appear on MR images as linear, hypointense bands against surrounding fluid and fat. T2- and proton-weighted pulse sequences with suppression of the MR signal from adipose tissue have been recognized as optimal for visualizing synovial folds.
Synovial fold syndrome (SPS) is accompanied by pain in the knee joint and impaired function, and should be considered by clinicians and radiologists as one of the possible diagnoses. A diffusely thickened fold, usually accompanied by local synovitis and erosions of articular cartilage, is the most common manifestation of CVS. Treatment of synovial fold syndrome consists of conservative management of the patient at the first stage; if ineffective, arthroscopic resection of the pathological fold is performed.
Introduction
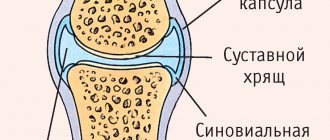
The fold of the knee joint is a duplication of the synovial membrane lining the joint cavity. The structure of synovial folds is thin, membranous, with zones of vascularization. From an embryogenetic point of view, the folds are partially vestigial synovial membranes and are found in the knee joints of healthy people. The exact function of synovial folds is unknown. A number of authors believe that synovial folds, like the eyelids, help improve the lubrication of the joint with synovial fluid.
In cases of direct trauma to the knee joint, with repeated stress or inflammation, clinical symptoms may occur due to the mechanical effect of the folds on other intra-articular structures. In particular, upon movement, the thickened and fibrotic synovial plica causes irritation of the synovial membrane at the edges of the bone condyles, which ultimately leads to reactive synovitis and thinning of the articular cartilage (synovial plica syndrome - SPL).
Changes in the mediopatellar fold occur most frequently, but an accurate assessment of the prevalence of CVS is difficult due to the lack of clear diagnostic criteria.
On MRI, intact synovial folds appear as thin, hypointense linear structures arising from the synovial lining. Their visualization is significantly improved in the presence of fluid in the joint (articular effusion, blood, or contrast agent during MR arthrography).
Diagnosis of diseases
Instrumental and clinical research methods are used to identify pathologies and disorders. During the consultation, the doctor collects anamnesis and conducts an initial examination and palpation of the affected joint. Attention is focused on the appearance of the shoulder: the presence of redness, a local increase in temperature, the size and distance to which the joint capsule has shifted. Patients who are concerned about shoulder pain are prescribed one of the types of X-ray examination: arthropnemography, contrast and plain radiography. These methods provide information about soft and hard tissues and allow you to prescribe the correct treatment and monitor recovery. If the x-ray turns out to be uninformative, then CT and MRI are used for diagnosis. To study the composition of the fluid that fills the synovial bursa, it is sent for cytological, biochemical and bacteriological examination.
Read also: Pain in the shoulder muscle of the left arm
Embryogenesis
Currently, it is widely believed that the knee joint initially consists of three compartments - medial, lateral and suprapatellar, separated by synovial septa. Incomplete resorption of these septa leads to the formation of well-developed synovial folds occupying the space between the distal parts of the epiphysis of the femur and the proximal parts of the tibia. Intrauterine movement in the fetal knee joint can simultaneously contribute to the resorption of folds and the formation of a joint cavity. This theory explains the presence of suprapatellar and infrapatellar folds, but is unfounded for the lateral and medial folds, since the patellofemoral joint is not divided into cavities in the plane of these folds at any stage of embryogenesis (that is, in the frontal one). Embryological work by S. Ogata and HK Uhthoff showed that the mediopatellar fold is not a remnant of the synovial septum. It is probably of mesenchymal origin and is associated with intrauterine lateralization of the patella, as evidenced by the predominance of mesenchyme in the mediopatellar zone.
There are no precise data in the literature on the prevalence of these persistent embryological structures in the population. In an anatomical study of the knee joints, T. Jouanin et al. in 11% of cases three main folds were present, in 10% no folds were identified. The suprapatellar and infrapatellar folds are the most common but are usually clinically intact. The lateral fold of the knee joint is extremely rare. Due to its clinical manifestations, the mediopatellar fold is the most studied to date.
Causes and symptoms of the disease
Bursitis of the shoulder joint often occurs in people involved in active physical activity: loaders, athletes. There are several causes of the disease:
- Constant intense physical activity.
- Gout.
- Received injury, bruises.
- Disturbance of metabolic processes in the body.
- Allergy.
- Weakened immunity.
- Intoxication of the body with alcohol or tobacco smoking.
Read also: Causes of pain in the shoulder joint of the left arm
The reasons can act both individually and in combination.
Symptoms to watch out for:
- swelling of the tissue around the sore joint;
- pain that intensifies when moving the arm, moving it back, when feeling the sore shoulder;
- limitation of joint mobility;
- significant decrease in sensitivity in the shoulder;
- sometimes the hand and forearm may become numb;
- There is an increase in muscle tone.
Possibilities of MRI in the diagnosis of synovial folds
On MR images, synovial folds appear as hypointense cords with peripheral fluid and fat. The most informative pulse sequences in the diagnosis of synovial folds due to the high signal from the fluid are recognized as gradient T2-weighted pulse sequences, as well as T2- or proton-weighted sequences using fat suppression. MR arthrography is applicable in case of insufficient amount of intra-articular fluid and the presence of pronounced clinical symptoms of the manifesting fold. The contrast agent provides high intertissue contrast of the articular surfaces, stretches the joint capsule, which together helps to visualize all folds of the knee joint, verify or exclude their pathological changes.
The size and morphological restructuring of synovial folds are not a reliable sign of their clinical significance. In the presence of persistent clinical symptoms and the absence of other possible causes of a similar symptom complex (for example, damage to the medial meniscus or internal collateral ligament, patellofemoral arthrosis, arthrosis of the medial parts of the joint), characteristic signs of pathological fold syndrome are local synovitis, erosion of the articular cartilage of the patella and the patellar surface of the femur bones.
Characteristics of the ankle cartilage
The anatomy of the ankle is not particularly complex. The joint consists of two main bones, the tibia and fibula. Additionally, feet are attached to them. The lower distal bones, by their location, form a socket, which is based on the process of the foot. This connection is the main ankle cartilage. It contains several main elements:
- outer ankle;
- inner ankle;
- bone elements.
There are two edges and surfaces on the outer ankle. In the back there is a depression to which the tendons of the peroneal muscles are attached. The lateral ligaments are attached to the outer surface of the ankle joint. An important element is the fascia; they are connective tissue membranes. The elements are formed by sheaths covering muscles, nerves and tendons.
On the inner surface there is hyaline cartilage. Together with the superior talus, it forms the outer space of the ankle joint. Taken together, all the elements represent a durable structure, which ensures optimal protection of the cartilage from negative environmental influences.
The anatomy of the connection is thought out by nature to the smallest detail. Thanks to this, the joints are mobile, elastic and flexible.
Suprapatellar fold
In the literature, there are several synonyms for the suprapatellar fold: suprapatellar septum, superior fold, patellar fold.
The suprapatellar fold is localized between the suprapatellar bursa and the cavity of the knee joint, has an obliquely descending course, starting from the synovium on the anterior surface of the femoral metaphysis and ending in the posterior part of the quadriceps tendon in the area of attachment to the patella. Until the end of the 4th month of intrauterine development of the fetus, the suprapatellar fold completely separates the cavity of the knee joint from the suprapatellar bursa, and by the end of the 5th month its shape does not differ from that of an adult.
It is believed that the key factor ensuring the degree of fold reduction is mechanical. Depending on the range of motion in the knee joint, either a small perforation in the fold or its partial or complete absence may form. T. Zidorn classified the degree of “development”, or more precisely, reduction, of the suprapatellar fold into 4 groups depending on the morphological features:
MR tomogram of the knee joint in T2 V.I., sagittal plane
- type I (septum completum) - closed suprapatellar bursa - the suprapatellar fold completely separates the patellar recess from the cavity of the knee joint;
- type II (septum perforatum) - the suprapatellar fold has one or more holes connecting the suprapatellar zone with the joint cavity;
- type III (septum residuale) – a residual connective tissue cord is visualized, often on the inside;
- type IV (septum extinctum) – characterized by complete involution of the suprapatellar fold.
In type II folds, the zones of its perforation, which provide circulation of articular fluid to the area of the inversion, are called the hilum.
The suprapatellar fold persists very often - up to 89% of cases according to autopsy data. On MRI of the knee, the fold is best identified in the sagittal plane as a linear hypointense band posterior and superior to the patella.
During arthroscopy, a completely unreduced suprapatellar fold can be suspected only by a decrease in the volume of the suprapatellar recess. Sometimes the diagnosis is made by chance during joint puncture, when the injection needle ends up in the suprapatellar bursa and not in the joint cavity.
Localization and structure
Closest to the shoulder joint are the subcoracoid and subscapularis bursae, which can fuse. It is believed that the subscapular bursa is a protrusion of the membrane of the joint. The shoulder is covered by 3 bundles of deltoid muscles: anterior, middle and posterior. Below them are the subacrominal and subdeltoid cavities, often connecting to form the subdeltoid bursa. At the base of the latissimus dorsi muscle are the axillary and subtendinous bursa. The hand makes a lot of movements thanks to the acromiocoracoid ligament under the corresponding tubercle, where there are 2 cavities: one under the ligament, and the other at the top of the acromion process. In the area of attachment of the pectoral muscle there is a corresponding joint capsule.
The average person has about 10 bursae in the shoulder joint.
Infrapatellar fold
The infrapatellar fold, or ligamentum mucosum, is the most common fold of the knee joint. Its formation occurs from 8 to 12 weeks of gestation and depends on the degree of involution of the primitive embryonic membrane separating the medial and lateral sections of the joint. The shape of the fold formed the basis for its arthroscopic classification by S. Kim and W. Choe:
- 0—no fold;
- 1 - complete persistence of the fold, the fold is separated from the anterior cruciate ligament;
- 2 - complete persistence of the fold, the fold is separated from the anterior cruciate ligament and has several bundles;
- 3 - vertical fold - complete persistence of the fold, which is associated with the anterior cruciate ligament and divides the joint cavity into medial and lateral sections;
- 4 - fenestrated vertical fold - a vertical fold with a hole/defect.
The infrapatellar fold begins in the anterior parts of the intercondylar recess of the femur, expands forward and downward, and attaches to the lower pole of the patella. The thickness of the fold varies widely from submillimeter to the size of the anterior cruciate ligament.
The infrapatellar fold is easily identified on sagittal MR images as a linear, hypointense structure running through the Hoffa fat pad in a plane parallel to the anterior cruciate ligament. In some cases, especially in patients with complete rupture of the anterior cruciate ligament, a well-developed infrapatellar fold can simulate its preserved bundles. It is also necessary to carry out a differential diagnosis of the infrapatellar fold with local nodular synovitis, postoperative changes and a loose body in the area of the Hoffa fat pad. The awareness of radiologists about the existence of this anatomical structure allows in most cases to make the correct diagnosis.
Functions of bags
Their appearance in the articulation area is associated with motor activity and the presence of load, tension or strong friction. Bursae are a way of adapting the body to human living conditions. Their main role in the life of the body is protection from injury, joint damage, ruptures and sprains. In addition, upon impact, they take part of the load upon themselves. The more movements a joint makes, the more bags appear. The shoulder joint, as the most mobile joint, has the largest number of bursae.
Mediopatellar fold
The mediopatellar fold is also called the medial fold, synovial patellar fold, pterygoid fold, patellar meniscus, and synovial protuberance. The mediopatellar fold begins in the area of the medial wall of the knee joint, goes obliquely downwards and is woven into the synovium around the Hoffa fat pad. It can be connected to the suprapatellar fold, but more often it has a separate attachment. If overdeveloped, the mediopatellar fold may extend to the medial surface of the femoral trochlea and the medial facet of the patella.
MR tomograms, axial plane, proton-weighted mode with signal suppression from adipose tissue
J. Sakakibara, based on the shape and size, identified 4 types of mediopatellar folds:
- type A – the fold is represented by a linear rope-like protrusion of the synovial wall;
- type B – the fold is represented by an elongated linear cord with uneven contours, but does not reach the medial condyle of the femur;
- type C – the fold is elongated, thickened, with uneven fringed contours, extending to the area of the medial condyle of the femur.
- type D – the fold extends to the area of the medial condyle of the femur, is thickened, uneven, and has a central defect (fenestrated fold).
This classification has received universal recognition and approval, as it is easy to use and clinically relevant. Types A and B of the mediopatellar fold are asymptomatic. Types C and D may impinge between the medial femoral condyle and the patella with subsequent thickening and induration, damaging the cartilage at the patellofemoral joint. The main mechanism of action of the fold is compression of the articular cartilage of the medial facet of the patella during flexion and the patellar surface of the medial femoral condyle during extension. A number of authors are of the opinion that the fenestrated mediopatellar fold (type D) more often causes damage (impingement) of the articular cartilage of the medial parts of the patellofemoral joint.
For visualization of the mediopatellar fold using MRI, T2- or proton-weighted images in the sagittal and axial planes with or without fat suppression are considered the most informative. The mediopatellar fold has a low MR signal and is easily recognized in a typical location against the background of a small amount of intra-articular fluid. On the other hand, one should always pay attention not only to the size of the fold and its location relative to the medial condyle, but also to the condition of the articular cartilage in the medial facet of the patella, femoral condyle, and the patient's complaints. With massive intra-articular effusion, lateral displacement of the fold may occur, complicating the differential diagnosis of types B and C. The large size of the mediopatellar fold may make it difficult to examine the medial parts of the joint during arthroscopy.
Hip cartilage and its specifics
The structural features of the hip joint are its nut-shaped shape and its belonging to the girdle of the lower extremities. The element connects the pelvic bone and cartilage through the articulation of the glenoid cavity. The surfaces of the bones are covered with a special smooth layer.
The fibrous capsule has an arrangement similar to that of the elbow joint. It is localized along the edge of the articular cavity, its cartilaginous lip is located in the cavity of the joint. The upper part of the capsule is attached to one quarter of the length of the femoral neck. At the back it doesn't even reach half of it.
Extra-articular and intra-articular ligaments of the hip joint strengthen its strength. The deep layers of the capsule are responsible for its contents. This area is called the round zone, it covers the femoral neck and underlies the bursa of the hip joint.
The main feature of the hip joint is its deeper fit. The joint is characterized by increased strength, but at the same time has less freedom of action. Healthy cartilage allows movement in three planes. Extension and flexion are carried out through the frontal axis.
Lateral patellar fold
Schematic representation of the anatomical structures of the lateral recess of the knee joint (normal)
The lateral patellar fold is the most rarely encountered fold of the knee joint. Most often, it has a longitudinal shape, is very thin and is located 1-2 cm lateral to the patella. The lateral patellar fold originates on the lateral wall and is attached to the infrapatellar fat body. S. Ogata and HK Uhthoff hypothesized that rare persistence of the lateral patellar fold is associated with lateral displacement of the patella, leaving no room for it in the lateral recess. The lateral fold may make it difficult to perform knee arthroscopy through the anterolateral approach.
The lateral patellar fold should not be confused with the more commonly encountered pterygoid, superolateral, and transverse arcuate folds.
The arrows indicate: in Figure A - lateral patellar fold (white thin arrow), lateral pterygoid fold (black thin arrow), transverse arcuate fold (black thick arrow); in Figure B - superolateral fold (white thick arrow).
The lateral pterygoid fold is located close to the patella along the outer wall, the superolateral fold is a type of suprapatellar fold dislocated outward. A transverse arcuate synovial fold is often found at the junction of the vertical and anteroposterior portions of the lateral recess.
Types of disease
There are several types of shoulder bursitis:
Subacromial or subdeltoid
Subacromial bursitis is characterized by severe pain in the arm when trying to move it to the side. At the same time, the limb moves forward and backward freely and almost painlessly. Damage to the bursa occurs below and above the joint.
The disease is accompanied by blood penetration into the bursa and loss of joint fluid.
Subcoracoidal (calcified)
This type of bursitis develops due to chronic injury to the periarticular bursa, or due to the deposition of calcium salts in it. Calcified shoulder bursitis is accompanied by severe pain when a person tries to move the shoulder back. If you do not pay attention to the first symptoms for a long time, then the movement of the shoulder joint is increasingly limited and sometimes reaches complete immobilization of the shoulder.
With calcified bursitis, acute inflammation of the joint capsule develops, throbbing pain appears, radiating to the neck and throughout the arm. The shoulder may also swell and body temperature may rise. Pain in the joint area can last up to several weeks, after which it subsides, but after a while it appears again.
Limestone (stone)
The most common type of shoulder bursitis. Stone bursitis develops as a result of metabolic disorders, so calcium salts accumulate in the area of the synovial bursa and cause inflammation.
As a result of bone growths, damage to cartilage tissue, and the accumulation of calcium particles in the joint fluid, the ability of the synovial fluid to lubricate the joints is significantly reduced.
There is pain in the joint area, the shoulder swells and turns red. Calcareous bursitis lasts a long time, its symptoms may go away on their own, but if the disease is not treated, it will become chronic.
Calculous
If there are multiple calcific deposits, then we can talk about calculous bursitis.
Calculous bursitis of the shoulder joint occurs as a result of damage and further destruction of the bursa due to the penetration of pyogenic bacteria and microbes into the area of the joint capsule.
Their waste products enter the blood and lymph and flow into the joint. Toxins accumulate, which leads to destruction of the bursa and changes in the composition of the fluid.
Very similar in its manifestations to subdeltoid bursitis. The pain is just as severe, the shoulder swells, the skin turns red around the inflamed joint. But in this case, the shoulder hurts much more than the arm.
Subdeltoid
A type of shoulder bursitis that can only be differentiated and treated by an experienced doctor. Certain points of the synovial membrane are affected, but the bursa is not completely damaged. Subdeltoid bursitis causes severe pain in the arm and shoulder. Moreover, the pain is so strong that even many painkillers cannot cope with it.
Subacromial
Subacromial bursitis occurs after injury, improper physical activity, or as a result of infection. It affects certain layers of the synovial membrane. It is difficult to raise your arm above your head.
Subcoracoid
It develops when the shoulder is dislocated when the bone of the shoulder joint comes out of place and moves back and forth, while stretching and compressing the subcoracoid bursa (an integral part of the shoulder joint).
Subcoracoid bursitis has the following symptoms: swelling of the shoulder, a sharp and severe increase in temperature, pain that intensifies when trying to raise the arm up, when pressing on the shoulder. With this type of disease, the bursa is damaged on the side of the joint.
Inflammation is accompanied by suppuration and penetration of pustular foci into the osteochondral structures.
Before treating shoulder bursitis, the following diagnostic methods are used to accurately diagnose:
- Initial examination and palpation of the diseased joint by a doctor, taking an anamnesis.
- X-ray or ultrasonic flaw detection.
- Puncture. In some types of shoulder bursitis, it is necessary to take joint fluid for analysis. This is necessary to determine its composition and the presence of various impurities in synovitis.
Treatment of bursitis of the shoulder joint is carried out comprehensively, which includes local, conservative, and surgical therapy.
Pathogenesis and clinical manifestations
Synovial fold syndrome (shelf-, plica-syndrome or their most common variety - mediopatellar fold syndrome) describes a complex of painful dysfunctions of the knee joint, in which the only finding is a thickened and fibrous-changed fold.
MRI scan of the knee joint
Patient A., 18 years old. MR imaging of the knee, proton-weighted fat suppression (axial plane) and arthroscopic slides. Complaints of pain in the internal parts of the knee joint. There is elongation, thickening, and fibrillation of the medial patellar fold, which reaches the medial femoral condyle (type C according to Sakakibara). The arrow indicates the area of “cracking” and chondromalacia of the articular cartilage of the medial facet of the patella.
The onset of pathology is usually an injury to the knee joint (direct blow, repeated load, twisting, leading to stretching of the fold), less often inflammatory and degenerative changes. Post-traumatic, inflammatory swelling of the fold leads to loss of elasticity, thickening and clinical manifestations if it reaches the patellofemoral joint during movements. The result of fibrosis and hypertrophy is reactive mechanical synovitis, as well as erosion of the articular cartilage of the femur and patella. In the early stages of the disease, the cause of pain is often the fold itself, while in a later period, chondromalacia of the articular cartilage and synovitis come to the fore. It should be remembered that the size, shape, and rigidity of the folds of the knee joint directly depend on the hereditary and constitutional characteristics of a particular person, however, most experts agree that a thick fold manifests itself clinically much more often than a thin one.
Mediopatellar fold syndrome is more often diagnosed in adolescents than in adults due to the rarer occurrence of concomitant lesions of the menisci and ligaments. The most typical occurrence of symptoms is after blunt trauma to the knee. The main complaint of patients is pain in the medial parts of the joint, which can occur both with load and at rest, and intensifies with repeated flexion/extension. The pain is localized medially from the patella, above the line of the joint space of the knee joint. Nonspecific signs include crepitus, popping, clicking, pseudojamming, and effusion. It is most often necessary to differentiate CVS from a medial meniscus tear and patellar instability. If a dense, painful cord is palpated medial to the patella, the diagnosis of mediopatellar fold syndrome becomes more likely.
There are two main mechanisms for the pathological effects of the suprapatellar fold. The first is compression of the knee joint cavity by the suprapatellar bursa with impingement of the articular cartilage of the superomedial parts of the femur during flexion. The second is inflammation of the suprapatellar bursa.
MRI scan of the knee joint (sagittal plane)
MR tomogram of the knee joint (sagittal plane) in T2-weighted mode with fat suppression before contrast (A) and T1-weighted after intravenous administration of a contrast agent (B). A completely unreduced suprapatellar fold is identified with the formation of a closed suprapatellar bursa. There is thickening of the synovial membrane of the bursa (signs of bursitis), prolapse of the lower pole of the bursa into the upper parts of the patellofemoral joint with compression phenomena.
As a rule, both pathological conditions occur with a completely unreduced fold (type I) with the formation of a closed suprapatellar (subquadricipital) cavity.
The lateral patellar fold is extremely rare and is usually asymptomatic. Clinical and MRI signs of lateral CVS are identical to those of mediopatellar fold syndrome. Manifestations of lateral CV joint may include pain in the lateral area of the joint and clicking. A palpable tourniquet-like painful cord of appropriate localization is a pathognomonic symptom.
Diseases, their causes and symptoms
Pathologies of the bags often involve the tissues of the joint in which they are localized. The shoulder joint is susceptible to injuries: falls, bruises, sprains, which occur due to heavy loads during training by athletes or careless sudden movements. As a result of injuries, a rupture of the bag occurs, characterized by severe pain in the shoulder joint and a crunching sound when moving the arm. The most common diseases are:
- Bursitis is an inflammation of the synovial bursa due to heavy stress, injury to the joint or tendons. It is characterized by swelling, redness of the skin at the site of the lesion, fever and pain. Tendobursitis is accompanied by inflammation and pathological changes in the tendon.
- All forms of arthritis and arthrosis are inflammations of the joint. Their symptoms are acute or aching pain in the affected area, joint deformation, redness, swelling of the joints and limited mobility. Occur due to injury, infection or metabolic disorders.
- Capsulitis is a rare pathology, manifested by stiffness of movement and pain. The reason is inflammation in the joint and sticking of its walls together and, as a result, the formation of scars due to which movements are very painful.
- The consequence of osteochondrosis of the cervical spine is a similar lesion of the shoulder joint. The affected area swells, pain is felt when touched with fingers, and hand mobility decreases.
Return to contents
Treatment
The first stage of treatment for CVS usually involves conservative techniques such as restriction of physical activity, massage, physical therapy, stretching of the hamstring muscles, and strengthening of the quadriceps femoris muscle. Drug therapy consists of cutaneous, oral or intra-articular administration of non-steroidal anti-inflammatory drugs and corticosteroids.
If conservative therapy is ineffective, arthroscopic resection of the synovial fold is performed. Radical surgery involves complete removal of the fold from the base. With a non-radical operation, for example, when dividing a fold with scissors, its independent repair may occur with the recurrence of symptoms.
An interesting study by DS Tearse et al., who, based on data from 3000 arthroscopy of the knee joint, found lateral folds in 21 patients. Of these, 14 were thickened, fibrous and correlated with the severity of complaints. In 13 patients, resection of the fold was accompanied by complete recovery.
Minimally invasive surgeries of the shoulder joint for inflammation of the periarticular bursa
Only in cases where drug treatment for shoulder bursitis, as well as physical therapy, have been unsuccessful and a person continues to feel tingling in the shoulder, does there become a need for surgical treatment of subacromial bursitis. We draw your attention to the fact that treatment of bursitis of the shoulder joint is carried out using arthroscopic minimally invasive techniques. This operation, during which the surgeon completely removes the inflamed joint capsule, is performed through the so-called “keyhole”.
Shoulder arthroscopy is a minimally invasive surgery for shoulder pain, for which the surgeon uses microscopic instruments with a diameter of 0.5 - 1 cm. An arthroscopic camera helps the doctor obtain a limited but accurate image of the surgical site. This intervention consists of aspiration (suction) of the contents from the joint capsule. In addition, in parallel, the surgeon can treat diseases that cause bursitis, such as impingement syndrome or calcification of the forearm. © bilderzwerg / fotolia
Additional operations when removing a bursa (bursectomy)
Additional interventions
- Removing calcium from the supraspinatus tendon
- Acromioplasty
- Suture placement of the supraspinatus tendon
In addition to the operation, the specialist examines and, if necessary, begins treatment of all structures of the shoulder joint. Thus, if bursitis is suspected, calcium deposits from the supraspinatus tendon, as well as bone spurs under the acromion, can be removed during arthroscopy.
Shoulder arthroscopy: Postoperative treatment and prognosis
After surgical removal of the periarticular bursa of the shoulder (bursectomy), a new bursa is formed in the same place within a short time, performing the functions of the removed tissue in full.
Motor functions of the shoulder are restored a few days after the operation. The pain syndrome disappears immediately.
Almost immediately, the patient can move the shoulder as before and return to previous activities. The stitches are removed after about 10 days.
Make an appointment
What does traditional medicine offer?
Home treatment is aimed at eliminating the symptoms of bursitis.
The main effects are heating, compresses, medicinal drinks.
Alcohol compresses
As a compress, you can use an alcohol tincture of propolis or simply moisten a cotton cloth in vodka, add Vishnevsky ointment and apply it to the shoulder. It is necessary to keep the compress throughout the day. The compress can be reapplied after 2 days.
Golden mustache decoction compress
1 tablespoon of chopped mustache is poured into a glass of water. The mixture is boiled in a closed container for 5 minutes. The broth is infused for an hour. Then soak the cloth in the broth and apply it to the sore shoulder. Insulate. The course is carried out at home at least 20 times, applying a compress every day.
Treatment with burdock rhizome
A tablespoon of crushed burdock root is poured into 1.5 liters of hot water. Leave for 30 minutes, then cool the broth, moisten a cotton cloth in it and apply it to the sore shoulder. Carefully secure with a bandage and leave for 2 hours. The procedure should be repeated at home until the swelling subsides and the pain subsides.
Grind the leaves of Kalanchoe so that they give juice, place them on a cloth and apply to the sore shoulder. Insulate with cling film and a woolen scarf. This remedy perfectly relieves inflammation.
Medicines
Painkillers are used: hormonal agents and non-steroidal analgesics, corticosteroids. To relieve pain and inflammation, hydrocortisone injections are given into the joint capsule. It is imperative to treat shoulder bursitis with ointments.
They eliminate pain and inflammation, restore the function of the arm and shoulder. They prescribe Ketonal, Collagen Ultra, Nise, Deep Relief gel, Voltaren, Fastum-gel. A variety of pepper ointments that have a warming effect (Finalgon, Mellivenon).