The joint capsule (bursa) is located in the extreme part of the cartilage and menisci. It is the main element that protects cartilage from serious mechanical damage and injury. Additional strengthening is provided by the muscles. The anatomy of the bursa depends on its location. The entire mechanism of the joint is enclosed in one capsule, which is based on cartilage, bones and ligaments. All this is hermetically hidden behind a special bag. It is attached to the bones and performs a lot of important functions.
Joint structure
Content
- 1 Structure 1.1 Articular surfaces
- 1.2 Joint capsule
- 1.3 Articular cavity
- 1.4 Periarticular tissues
- 1.5 Joint ligaments
- 2.1 Cylindrical joint
Joints
(lat. articulatio) - movable joints of skeletal bones, separated by a gap, covered with a synovial membrane and an articular capsule. An intermittent, cavity-like connection that allows the articulating bones to move relative to each other with the help of muscles. The joints are located in the skeleton where distinct movements occur: flexion (Latin flexio) and extension (Latin extensio), abduction (Latin abductio) and adduction (Latin adductio), pronation (Latin pronatio) and supination (Latin . supinatio), rotation (lat. circumductio). As an integral organ, the joint takes an important part in supporting and motor functions. All joints are divided into simple, formed by two articular surfaces, and complex, consisting of several simple ones.
Structure[ | ]
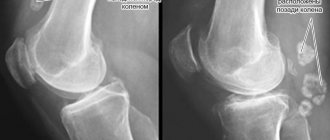
Each joint has articular surfaces, most often covered with hyaline cartilage, an articular capsule and an articular cavity containing a small amount of synovial fluid. In the cavity of the knee joint there are menisci - these cartilaginous formations increase the congruence (compliance) of the articular surfaces and are additional shock absorbers that soften the effect of shocks.
Main elements of the joint:
- articular surfaces covered with cartilage
- Articular cavity;
- joint capsule;
- synovial membrane;
- synovial fluid.
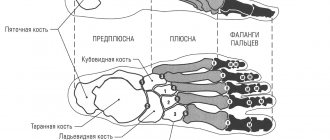
Articular surfaces[ | ]
Articular surfaces
(lat. fácies articuláres) articulating bones are covered with hyaline (less often fibrous) articular cartilage 0.2-0.5 thick. Constant friction maintains smoothness, facilitating the sliding of the articular surfaces, and the cartilage itself, thanks to its elastic properties, softens shocks, acting as a buffer [1].
Joint capsule[ | ]
Joint capsule
(lat. capsula articuláris) or
articular capsule
- attached to the connecting bones near the edges of the articular surfaces or retreating some distance from them, hermetically surrounds the articular cavity, protects the joint from various external damage (ruptures and mechanical damage). The joint capsule consists of dense fibers that give it strength. Fibers from the ligaments and tendons of nearby muscles are also woven into it. Covered with an outer fibrous and inner synovial membrane.
Outer layer
denser, thicker and stronger than the internal one, it is formed from dense fibrous connective tissue with a predominantly longitudinal direction of the fibers. Often the articular capsule is supported by ligaments (Latin ligamenta), which strengthen the articular capsule.
Inner layer
represented by a synovial membrane, the function of which is the secretion of synovial fluid from synovial villi on the synovial membrane, which in turn:
- nourishes the joint
- moisturizes it
- eliminates friction of articular surfaces.
This is the most innervated part of the joint, responsible for pain sensitivity [2].
Articular cavity[ | ]
Articular cavity
- a slit-like hermetically sealed space limited by the synovial membrane and articular surfaces. The articular cavity of the joint may contain discs and menisci.
Periarticular tissues[ | ]
Periarticular tissues
- these are the tissues immediately surrounding the joint: muscles, tendons, ligaments, blood vessels and nerves[3]. They are sensitive to any internal and external negative influences; disturbances in them immediately affect the condition of the joint. The muscles surrounding the joint provide direct movement of the joint and strengthen it from the outside. Numerous nerve pathways, blood and lymphatic vessels feeding the joints pass through the intermuscular connective tissue layers.
Joint ligaments[ | ]
Joint ligaments
- strong, dense formations that strengthen the connections between bones and limit the range of motion in the joints. Ligaments are located on the outside of the joint capsule; in some joints (knee, hip) they are located inside to provide greater strength.
The blood supply to the joint is carried out from a widely anastomosing (branched) articular arterial network formed by 3-8 arteries. The joint is innervated by its nervous network formed by sympathetic and spinal nerves.
All articular elements (except for hyaline cartilage) have innervation, in other words, they contain significant numbers of nerve endings that, in particular, carry out pain perception, and therefore can become a source of pain.
What is the basis of the knee joints?
The joint capsule is additionally strengthened by tendons, and the kneecap is located next to it. It covers and protects the cartilage from excessive pressure and negative influences from the external environment. On the sides there are internal and external ligaments; they act as additional reinforcing elements.
Cartilage tissue contains many folds that provide flexibility. The inner lining of the knee joint lines the articular surfaces of the bones, forming pockets. In medical practice they are called volvulus and bursae. This is where the common disease bursitis originates.
The cavity of the knee joint has a close relationship with the synovial bursae. A total of 13 main twists are recorded, which affect flexibility and the production of the required amount of joint fluid. These elements form a single cavity.
The bursa is a small pocket completely filled with fluid. The main function of the element is to reduce the load on the knee joint during movement. The bursa absorbs shock and mechanical stress. It is in close proximity to the cartilage. The outside of the protective element is lined with a fibrous membrane. It is characterized by increased density and strength. It is based on dense connective tissue.
The lining of the knee cartilage is responsible for the production of synovial fluid. It plays an important role in the performance of the joint. The shell is very sensitive to injuries and impacts of various types.
Classification of joints[ | ]
According to the current anatomical and physiological classification, joints are distinguished [4]:
- by the number of articular surfaces
- according to the shape of the articular surfaces and functions.
According to the number of articular surfaces
:
- simple joint (lat. articulatio simplex) - has two articular surfaces, for example the interphalangeal joint of the thumb;
- complex joint (lat. articulatio composita) - has more than two articular surfaces, for example the elbow joint;
- complex joint (lat. articulatio complexa) - contains intra-articular cartilage (meniscus or disc), dividing the joint into two chambers, for example the knee joint;
- combined joint (lat. articulatio combinata) is a combination of several isolated joints located separately from each other, for example the temporomandibular joint.
According to the function and shape of the articular surfaces
.
- Uniaxial joints:
- Cylindrical joint, (lat. art. cylindrica), for example atlanto-axial median;
- Trochlear joint, (lat. art. ginglymus), for example interphalangeal joints of the fingers;
- A helical joint is a type of trochlear joint, for example the humeroulnar joint.
- Biaxial joints:
- Elliptical (lat. art. ellipsoidea), for example the wrist joint;
- Condylar (lat. art. condylaris), for example the knee joint;
- Saddle (lat. art. sellaris), for example, the carpometacarpal joint of the first finger;
- Multi-axis joints:
- Spherical (lat. art. spheroidea), for example, the shoulder joint;
- Cup-shaped, as a type of spherical, such as the hip joint;
- Flat (lat. art. plana), for example intervertebral joints.
Cylindrical joint[ | ]
Cylindrical joint
(
rotational joint
) is a cylindrical articular surface, the axis of which is located in the vertical axis of the body or parallel to the long axis of the articulating bones and provides movement around one (vertical) axis - rotation (lat. rotatio) [4].
Trochlear joint[ | ]
Trochlear joint
— the articular surface is a cylinder lying in the frontal plane, located perpendicular to the long axis of the articulating bones [4].
Elliptical joint[ | ]
Elliptical joint
- articular surfaces have the form of elliptical segments (one convex and the other concave), which provide movement around two mutually perpendicular axes [4].
Condylar joint[ | ]
Condylar joint
- has a convex articular head, in the form of a protruding process (condyle), close in shape to an ellipse. The condyle corresponds to a depression on the articular surface of another bone, although their surfaces may differ significantly from each other. The condylar joint can be considered as a transitional form from the trochlear joint to the ellipsoid joint [4].
Saddle joint[ | ]
Saddle joint
- formed by two saddle-shaped articular surfaces, sitting “astride” each other, of which one moves along the other, due to which movement in two mutually perpendicular axes is possible [4].
Ball and socket joint[ | ]
Ball and socket joint
- one of the articular surfaces is represented by a convex spherical head, and the other is a correspondingly concave articular cavity. Theoretically, movement in this type of joint can be carried out around many axes, but in practice only three are used. The ball and socket joint is the loosest of all joints[4].
Flat joint[ | ]
Flat joint
- have practically flat articular surfaces (the surface of a ball with a very large radius), so movements are possible around all three axes, but the range of movements due to the slight difference in the areas of the articular surfaces is insignificant [4].
Tight joint or stiff[ | ]
Tight joint
(
amphiarthrosis
) - represent a group of joints with different shapes of articular surfaces with a tightly stretched capsule and a very strong auxiliary ligamentous apparatus; closely adjacent articular surfaces sharply limit the range of movements in this type of joint. Tight joints smooth out shocks and soften shocks between bones[4].
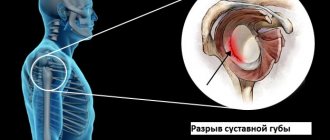
Shoulder and elbow joints
There are several bursae around the shoulder cartilage. Together they make up the sliding apparatus of muscle-tendon formations.
| Element | Characteristics |
| The most important and permanent element is the subscapular bursa. | It is characterized by a superficial location, which provides strong protection of the elbow joint. The subscapularis bursa is considered as an extra-articular protrusion located in the synovium of the shoulder joint. |
| There is another important element - the intertubercular bursa. | Its inversion covers the heads of the biceps brachii muscles and passes through the entire cavity of the cartilage. |
The tendon passes at the level of the greater and lesser tubercles. It is located in a special groove. A dense overlap is fixed on all sides of the humeral cartilage, without fusion with the main capsule.
The cellular junction contains the synovial bursae. Some of them are located on top of the tendon, the other - under the acromion process. In some cases, fusion of the shoulder joint bags is recorded. The result of this process is a common subdeltoid bursa.
The axillary neurovascular bundle with surrounded nerves is located inside the formation. Its location is closely related to the main access to the cartilage. The condition of the elbow joint directly depends on its protection.
Why is cervical lymphadenopathy dangerous? Back pain: how to get rid of it? What causes numbness in your hands? More details>>
Joint diseases[ | ]
Joint hypermobility
- increased joint mobility; stretching of the articular ligaments, allowing the joint to make more extensive movements beyond the limits of its anatomical capabilities. As a result, elements of contacting cartilaginous surfaces can produce characteristic clicks. This extensibility of the articular ligaments occurs as a result of a structural change in collagen, which becomes less strong and more elastic and becomes capable of partial deformation. This factor is of hereditary origin, but the mechanism of development of this connective tissue inferiority still remains unknown.
Hypermobility is detected mostly in women, and young ones at that. The genetic determination of hypermobility leads to changes in many tissues. First of all, joints, but also those organs that contain a lot of altered collagen. For example, such people have thin, stretchable and vulnerable skin; stretch marks easily appear on it, and they appear even in very young girls or women who have never given birth. With joint hypermobility, vascular incompetence is also observed, because their walls also consist of collagen. If it is extensible, then the blood vessels stretch very quickly under the pressure of blood. Hence, such people have early varicose veins (at 25 or even 20 years old).
People with hypermobility are not recommended to choose a job where they need to stay in the same position for a long time (this is especially true for teachers, salespeople, surgeons, and hairdressers who stand for several hours at a time). People in these professions have a very high risk of developing varicose veins and arthrosis, and if they have hypermobility, the risk is almost one hundred percent. In addition, you need to be careful when playing sports so as not to cause even more hyperextension of the ligaments.
Joint swelling occurs when fluid accumulates in the tissues. It may be accompanied by pain and stiffness.
Capsulitis —
diffuse damage to the capsule and synovium of the shoulder joint. It often leads to quite long-term disability of the patient. It most often occurs in older people (from 50 to 70 years old), with women getting sick more often than men. Often the pain is worse at night or just lying down if the person is lying on the sore shoulder.[5]
Bursitis (inflammation of the bursae)
Inflammation of the synovial bursa most often occurs in the joint area with excessive accumulation of fluid (exudate). Exudate during inflammation can be serous, in the presence of infection - purulent, as a result of injury - hemorrhagic (with blood or plasma).
Bursitis is a fairly common disease, most often occurring in the shoulder, elbow, knee and hip joints.
With age, the risk of inflammation increases. This disease often affects people whose professions require significant physical activity and constant fixed position of the limbs (athletes, loaders, musicians, artists, etc.), excess weight plays an important role.
Symptoms of bursitis
Bursitis can be either chronic or acute. In acute bursitis, the disease develops rapidly - within 2-3 days. A person may wake up with swelling and severe pain in the joint area and a local fever. After a few days, the symptoms increase and then subside. If left untreated, the process can become chronic.
Have you noticed the following symptoms? Make an appointment
The chronic process develops slowly, usually against the background of some chronic infection or acute form. There is limited swelling in the joint area, the wall of the bursa becomes denser, but the joint still remains mobile. The chronic form entails further formation of adhesions in the joint, frequent relapses and severe limitation of movement.
Causes of bursitis
The causes of bursitis can be:
- injury
- infection in the wound (through an abrasion or cut)
- chronic inflammatory, infectious and systemic diseases (arthritis, diabetes mellitus, gout, tuberculosis, brucellosis, furunculosis, etc.)
- sexually transmitted diseases
- simple cold
Diagnosis of bursitis
The first stage in diagnosing this disease is an examination by an orthopedic traumatologist or rheumatologist. The doctor collects an anamnesis of the person’s life and professional activities, information about previous diseases and injuries, on the basis of which he will recommend the necessary examination.
We recommend that you consult a doctor! 276-00-15
As a rule, when diagnosing bursitis, it is necessary to take a general blood test, and if a chronic form of bursitis is suspected, a biochemical blood test, including specific proteins. In some cases, tests are performed for sexually transmitted diseases.
To assess the full picture of the disease, an X-ray and ultrasound examination of the joint, computer (CT) or magnetic resonance (MRI) diagnostics, puncture of the synovial bursa with examination of the contents and sending it for bacteriological examination are required. In order not to miss systemic diseases, hormonal and immune status is examined.
Treatment of bursitis
To treat bursitis, it is necessary first of all to provide rest and cold to the inflamed joint to relieve swelling, since when moving, the synovial bursa moves, creating friction, which aggravates the process.
With conservative treatment, anti-inflammatory and painkillers are prescribed. If necessary, a puncture of the synovial bursa is performed with pumping out the contents, sanitizing the cavity with antiseptics and administering glucocorticosteroids (hormones) to relieve the inflammatory process.
doctor
If the cause of bursitis is an infection, broad-spectrum antibiotics, immunomodulators and drugs to maintain intestinal microflora are prescribed. Physiotherapy and ozone therapy are possible only after the acute process has resolved - during the period of remission and rehabilitation.
Surgical treatment of bursitis is carried out in case of purulent inflammation or in case of ineffectiveness of drug treatment, the essence of which is to remove the synovial bursa (bursectomy).
Prevention of bursitis
At the first signs of the disease, you should consult a specialist. If you previously had bursitis, you need to protect the joint from unnecessary stress and injury, lead a healthy lifestyle, do not smoke, go swimming, exercise therapy, undergo sanatorium treatment, and lose excess weight.
Notes[ | ]
- Human anatomy. — 9th ed., revised. and additional - M.: Medicine, 1985. - P. -63. — 672 p. — (Educational literature for students of medical institutes). — 110,000 copies.
- Types of bone joints
- Publication for practicing doctors “Russian Medical Journal”.
Paraarticular tissues: variants of lesions and their treatment (continued)
(unspecified)
.
www.rmj.ru.
_ Date accessed: November 18, 2021. - ↑ 123456789
Human anatomy / Prives M. G., Lysenkov N. K. - 9th ed., revised. and additional - M.: Medicine, 1985. - P. -66. — 672 p. — (Educational literature for students of medical institutes). — 110,000 copies. - Publication for practicing doctors “Russian Medical Journal”.
Capsulitis (“frozen shoulder”)
(undefined)
.
www.rmj.ru.
_ Date accessed: November 18, 2021.