Anatomical structure of the foot
The foot has three sections: the tarsus, metatarsus and phalanges.
The tarsus is formed by seven short spongy bones arranged in two rows. The posterior row includes the calcaneus and talus. The anterior row consists of an internal group of bones: the scaphoid, medial, medial and lateral sphenoid, and the externally located cuboid.
The metatarsus consists of five metatarsal bones. These are short tubular bones that have a base, body and head. The 1st, 2nd and 3rd metatarsals are connected at their base to the sphenoid bones, and the 4th and 5th to the cuboid bone. 1st metatarsal bone is the shortest and thickest, 2nd is the longest. It has been established that the mechanical strength of the 1st and 5th metatarsals is 3 times higher than the strength of 2,3,4.
The phalanges of the fingers are short tubular bones. The fingers act as additional supporting areas when walking (see below The process of walking). A clear idea of the role of the toes in the supporting function of the foot can be obtained by looking at the inner surface of the insole of worn shoes, where the areas of the foot on which we rest when walking are clearly contoured.
These bones, varied in shape and size, form the foot; they are connected to each other using numerous ligaments and muscles that provide mobility in three planes. The activity of the foot and lower leg muscles helps maintain the shape and function of the foot.
Hip joint
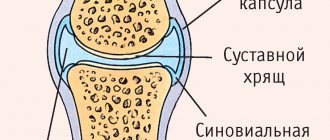
The hip joints connect the lower limbs (thigh bones) to the pelvis. The hip is the largest and most heavily loaded joint. It is a classic hinge: it consists of a spherical head of the femur (1) inserted into a concave round acetabulum (2) in the pelvic bones. Both the head of the femur and the acetabulum are covered with elastic and durable cartilage (3). The cavity of the hip joint contains slippery synovial fluid (4), which reduces friction, softens shock and transfers some nutrients. The head of the femur is supplied with blood from the vascular bundle (5) passing inside the hip joint.
The structure of the hip joint. (1) head of the femur, (2) acetabulum, (3) elastic cartilage, (4) synovial fluid, (5) vessels inside the joint.
The hip joint usually responds well to treatment, except in cases of significant destruction of the joint tissue. It is important not only to relieve inflammation and pain, but to pay attention to blood circulation in the joint, ensuring its nutrition, and proper muscle function. We often find that the cause of arthrosis is metabolic disorders, treatment of which is possible and necessary.
Common hip problems
Arthrosis of the hip joint (coxarthrosis). This disease begins with overload and deterioration in the nutrition of the joint, or with its inflammation. As a result, the volume of fluid in the hip joint decreases, the cartilage becomes thinned and torn, hence pain and limited mobility in the joint. Read more…
Hip dysplasia is a congenital underdevelopment of the acetabulum. We often see dysplasia as the cause of dislocations and arthrosis, even in advanced aged patients. The roof of the acetabulum in this case only partially covers the head of the femur. Thus, the area of support of one articular surface on another is reduced, which means that the pressure per unit area of the joint increases significantly. In addition, excessive movements during walking are possible in such a joint, which over time destroys the hip joint. Read more…
Inflammation of the hip joint (coxitis, arthritis) occurs with arthrosis, overload of the joint and with such serious rheumatic diseases as ankylosing spondylitis, gout, articular psoriasis, reactive arthritis, systemic lupus erythematosus. For proper treatment, it is necessary to accurately find the cause of inflammation, and we do this with the help of modern laboratory tests. Read more...
Aseptic necrosis of the femoral head occurs when there is blockage or compression of the vascular bundle supplying the femoral head with blood. As a result of bleeding, the head of the femur dies and is destroyed, which leads to pain and immobility. It is important to immediately establish and eliminate the cause of the blockage of the vessel, because there is a possible risk of blockage of other important arteries and veins (stroke, necrosis of another joint, etc.).. Read more…
A hip fracture is common in osteoporosis, a loss of calcium in the bones. The femoral neck is the thinnest and least durable section of the femur. The completed fracture is subject to surgical treatment (fixation with a metal structure) in the traumatology department. We will provide assistance if surgery is not possible, or if pain and immobility remain after surgery. Read more...
A herniated disc and painful sciatic nerve can mimic hip pain. Read more…
Functional structure of the foot
The foot, as a structure, has a rather complex arched shape, reminiscent of a spiral or propeller blade. The foot has an arched structure. It is customary to distinguish between two longitudinal arches and one transverse arch.
Longitudinal bone arches: internal (spring) is formed by the calcaneus, talus, navicular, three wedge-shaped, 1,2,3 metatarsal bones, is an arch that runs through the entire foot, starts from the calcaneal tubercle and ends at the fulcrum of the head of the 1st metatarsal bone;
the outer (cargo) is formed by the calcaneus, cuboid, 4th and 5th metatarsal bones, and also has the shape of an arc that runs through the entire foot, starting from the heel tubercle and ending at the fulcrum of the head of the 5th metatarsal bone.
The vast majority of doctors do not doubt the existence of the transverse fornix, but there are two opinions regarding its localization. First: the transverse bony arch is an arch formed by all the heads of the metatarsal bones. It is located in a plane perpendicular to the arcs of the longitudinal arches. Second: the transverse arch is most clearly expressed in the area of the sphenoid, cuboid and bases of the metatarsal bones.
It is possible to consider the arches of the foot as independent elements only conditionally, since in reality they are in constant interaction and function as a single organ. In maintaining the arched shape of the foot, the leading role belongs to the ligaments, plantar aponeurosis and tendons of the muscles that pass from the lower leg to the foot, and the actual muscles of the dorsal and plantar surfaces of the foot.
The foot is supported at three points: the area of the heel tubercle, the heads of the 1st and 5th metatarsal bones. The pressure between the front and rear support points is normally distributed as 1:4.
Between the bony skeleton of the foot and the supporting surface there are soft tissue structures (muscles, ligaments, subcutaneous tissue, the layer of skin itself), which form the relief of the plantar surface of the foot; numerous vessels and nerves of the foot pass through here. The skin of the plantar area in places of contact with the support has a cellular structure. Fibrous cords are located perpendicularly in it, between which there are areas of adipose tissue, which are good shock absorbers. In the area of support points (heel, area of metatarsophalangeal joints) the skin is denser and resistant to compression.
Jaw (temporomandibular, TMJ) joint
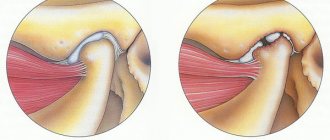
The temporomandibular joint (TMJ) is a movable and very strong connection of the lower jaw with the temporal bone of the skull. The TMJ consists of the articular head of the lower jaw (1), the mandibular fossa (2) and tubercle (3) and the intra-articular cartilaginous disc (4). The rubbing surfaces of the joint are covered with cartilage. Normally, the intra-articular disc serves as a softening pad and is constantly located between the articular head and the fossa, even when the mouth is opened. Normal operation of the TMJ is possible while maintaining proper closure of the teeth.
The structure of the temporomandibular joint. jaw, (2) mandibular fossa, (3) tubercle, (4) intra-articular cartilaginous disc.
The temporomandibular joint suffers from malocclusion, as a result of disease or loss of teeth, from injury (a blow to the jaw), or from inflammation (arthritis). If the disc is damaged (subluxated, thinned, or ruptured), it no longer protects the articular head from friction, and then pain, crunching, clicking, limited jaw movement, and even inflammation with swelling may occur. Symptoms of suffering from the temporomandibular joint are often mistaken for diseases of the teeth, trigeminal and facial nerves, and ear.
Typical temporomandibular joint problems
Temporomandibular joint dysfunction is a violation of joint mobility, in the form of limited or increased movement, lateral displacement, clicking in the joint, pain in the muscles and nerves of the face. If TMJ dysfunction continues for a long time, the articular cartilage wears out prematurely, and in these cases we often see arthrosis or arthritis. This disorder is often mistaken for trigeminal neuralgia, and is treated for a long time and ineffectively. Read more…
Arthrosis of the temporomandibular joint usually develops as a result of long-term dysfunction, trauma or inflammation. The articular disc and cartilage become thinned and torn, hence pain and limited mobility in the joint. The diagnosis of arthrosis of the TMJ is easy to establish during examination and using x-rays. Comprehensive treatment usually helps relieve pain and improve mobility. Read more…
Inflammation of the temporomandibular joint (arthritis) occurs with arthrosis, after injury and with such serious rheumatic diseases as rheumatoid arthritis, ankylosing spondylitis, gout, articular psoriasis, reactive arthritis, systemic lupus erythematosus. To properly treat TMJ arthritis, it is necessary to find the exact cause of the inflammation, and we do this with the help of modern laboratory tests. Read more...
Immobilization (contracture) of the temporomandibular joint after injury or inflammation. Read more...
Trismus is a spasm of the jaw muscles, with difficulty opening the mouth . This is a consequence of pain in the teeth or temporomandibular joint, against the background of a depleted state of the nervous system. Read more...
Features of a child's foot
In children under 3 years of age, the subcutaneous fat layer is significantly developed; it fills the entire niche of the internal longitudinal arch, performing an arch-forming role and the role of a shock absorber.
The ligaments of a child’s foot contain few elastic fibers and a lot of ground substance. The main role in the passive fixation of the arches belongs to the plantar aponeurosis.
Children have wider joint spaces than adults. This makes the joints mobile and reduces the role of the articular surfaces as a passive stabilizer of the arches. Up to 6 years of age, X-rays do not show lines of force in the bones of the foot, which indicates their functional failure and vulnerability. The tarsal bones are not differentiated until the age of 6 years.
Only a doctor can assess the true condition of a child’s feet based on clinical examination data, measurements of foot parameters, and plantography.
It should be noted that in children under 3 years of age, upon examination, this fat pad gives false impressions of a decrease in the size of the soft arch and flattening of the internal longitudinal arch.
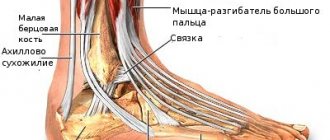
Wrist joint
The wrist (carpal) joint is a movable connection of the carpal bones of the hand (1) with the radius (2) and ulna (3) bones. The articular ends of the bones that form the joint are covered with strong and elastic cartilage (4), and the joint cavity is filled with slippery synovial fluid (5), which reduces friction and transfers some nutrients. The joint is very strong and mobile. It is reinforced on all sides with strong ligaments. The wrist joint contains nerves and tendons that control the fingers.
The structure of the wrist joint. (1) carpal bones of the hand, (2) radius, (3) ulna, (4) elastic cartilage, (5) synovial fluid.
The wrist joint usually responds well to treatment, except in cases of significant destruction of the joint tissue. It is important not only to relieve inflammation and pain, but to pay attention to blood circulation in the joint, ensuring its nutrition, and proper muscle function. We often find that the wrist joint suffers during certain professional and sports activities (musicians, tennis players, athletes).
Typical wrist joint problems
Arthrosis of the wrist joint usually develops after injury or inflammation. Often - after a fracture of the bones of the forearm. The volume of synovial fluid in the joint decreases, the cartilage becomes thinned and torn, hence pain and limited mobility in the joint. The diagnosis is easy to establish by examination and x-rays. Comprehensive treatment usually helps relieve pain and improve mobility. Read more…
Inflammation of the wrist joint (arthritis) occurs with arthrosis and such serious rheumatic diseases as rheumatoid arthritis, ankylosing spondylitis, gout, articular psoriasis, reactive arthritis, systemic lupus erythematosus. For proper treatment, it is necessary to accurately find the cause of inflammation, and we do this with the help of modern laboratory tests. Read more...
Immobilization (contracture) of the wrist joint after injury or inflammation. Read more...
Infringement and damage (neuropathy) of the radial, ulnar or median nerves occurs after injuries, inflammation in the joint and arthrosis. In most cases, the nerve can be freed without surgery.