As one friend of mine, a very good ENT doctor, said about the possibility of conservative treatment of a deviated nasal septum: “If a fence falls on the street, you need to call special equipment and put it in place.” Operate. No options. Also with hallux valgus deformity. You should not hope that various orthopedic products (insoles, inserts) will solve the problem. Yes, all this is good in the early stages, but if you are reading this article, then the methods of conservative therapy have probably already exhausted themselves.
What I have always liked about traumatology is that healing and craft are intertwined in it. Moreover, craft is on the verge of art. This is all clearly visible in the methods of surgical correction of Hallux valgus: each doctor’s case will be unique! Correction of each foot will have its own characteristics.
Currently, more than 200 methods of surgical treatment of hallux valgus are known (according to other sources - more than 300). Many of them led to a poor prognosis in treatment due to the fact that at the time of their appearance the mechanism of the formation of hallux valgus was not understood. Other techniques were hardly distinguishable from the “original”, supplemented by the author’s “touches”. The development of surgery is a method of trial and selection of the best options. It is worth noting only those few techniques that have been time-tested, improved and are currently used. And what is also very important: cosmetic surgery is completely inappropriate for Hallux valgus. In order for there to be indications for surgery, the patient must be bothered by pain that is not corrected by the usual change of shoes and orthopedic products.
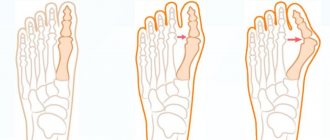
Operations for hallux valgus deformity can be divided into groups: operations on soft tissues, operations on bones and their combinations.
Soft tissue operations
Operation Silver
The essence of the technique is cutting off the tendon of the adductor muscle of the big toe. As a rule, it is one of the stages of combined techniques.
Operation McBride
The adductor tendon is not simply cut off, but transferred. Quite often combined with Shede's operation.
The illustration shows the creation of a “tunnel” through the metatarsal head and the passage of the adductor tendon through it. In various modifications of McBride, the tendon can be sutured to the capsule and head of the metatarsal bone, or fixed on the back of the head. The modifications have the same goal: to reduce the angle between the metatarsals.
Operation Mann (RA Mann)
Distal soft tissue procedure. It is currently an integral part of many combined operations. The goal of the procedure is to restore the position of the sesamoid bones in the thumb area.
Sesamoid bones are displaced laterally during valgus deformity. Returning them to their previous anatomical position is carried out by cutting off the tendon of the adductor pollicis muscle from the lateral sesamoid bone, excision of the lateral collateral ligament, making releasing incisions on the outer surface of the joint capsule and intersection of the metatarsesamoid ligament. It can be performed through an arthroscope. In this case, the traumatic nature of the operation is significantly reduced.
Bone operations
Akin wedge osteotomy
Small in volume and technically relatively simple operation. A wedge-shaped resection is performed in the area of the proximal phalanx of the thumb. It is now usually used in combination with other techniques. Used in isolation for interphalangeal valgus.
Technique of operation. A longitudinal incision is made over the metatarsal head, then the incision is extended distally. Resection begins with a distance of 5-7 mm from the joint. The base of the wedge itself is usually 3-4 mm. Bone fragments are fixed with knitting needles, sutures, or special staples.
Operation Schede-Brandes
This technique can be called “classical”. Despite the fact that it has a number of disadvantages, it is still used. The essence of the operation is to remove the inner part of the head of the first metatarsal bone. This is the removal of that very bone. As some patients say, “just take it and cut off the lump.” Shede's operation in its purest form. In 1929, Brandes recommended resecting the base proximally of the thumb phalanx.
The attitudes of specialists towards the Schede-Brandes technique are ambiguous, especially since it looks “mutilating”. And although there are observations of long-term treatment results (up to 23 years), which have a positive result (Kudinsky Yu.G., 1967), there are still cooler reviews. The positive aspects of the operation include its relative simplicity. In addition, it can be performed without applying a tourniquet (important for patients with chronic venous and arterial insufficiency) and without complex instruments and metal structures. Fast recovery time. It is not contraindicated in patients with osteoporosis, so it is often performed on elderly patients. The disadvantages of the operation lie in the technical features. Removal of the base of the phalanx leads to disruption of the foot roll function. In addition, the big toe is shortened (especially in patients with an antique foot shape, for whom indications are limited). It also does not increase the range of motion in the thumb if it is rigid, Hallux rigidus (“mussel picker’s disease”). In case of rigidity, the first stage is performed according to Keller. Category of patients: sedentary and elderly people with signs of arthrosis in the metatarsophalangeal joint
Arthrodesis of the metatarsophalangeal joint
The essence of the operation is to fix the head of the metatarsal bone on the main phalanx of the big toe, as a result of which the joint becomes a fixed joint.
The purpose of such an intervention is to make the joint, with severe valgus deformity, firmly aligned and immobile. Subsequently, in most cases, the pain syndrome is relieved, since movement in the affected joint is eliminated. Arthrodesis of the big toe is usually performed in patients who already have severe arthrosis or severe hallux rigidus. However, this intervention can be successfully used in severe hallux valgus. To turn two bones in a joint into a fixed joint, you need to completely remove the cartilage from the articular surface - this will lead to fusion. The bones must be aligned in such a way as to provide the most advantageous functional position. The connection is secured with two or three screws, although a metal plate is often used to stabilize the connection. Depending on the age and general condition of the patient, recovery takes 6-12 weeks. During this time, walking with emphasis on the heel is allowed. Or they wear special orthopedic shoes, such as Cam Walker Boots. What complications can there be? Complications are rare and are usually associated with problems with wound healing or with impaired fusion of the stabilized bones. As for specific problems, an important task for the surgeon is the correct choice of the angle of deviation of the thumb. Otherwise, there will be excessive stress on the immovable finger when walking.
Chevron osteotomy
It is also called Austin osteotomy, as it was first performed by doctor Dale W. Austin in 1962 in the USA. The name "chevron" is in honor of the US military patch, the chevron, V-shaped.
The main advantage of chevron osteotomy is the relative simplicity of the operation and long-lasting positive results. There are various options for this operation. The difference lies in the change in the area of the cuts. Or by changing the length of the arms of this “V”. The cross-sectional areas may be the same or different. Such differences in options are associated with the improvement of the technique for various clinical situations. Variants of chevron osteotomy are mainly associated with changes in the direction and length of the bone cut. Indications for Austin osteotomy The operation is recommended for persons with mild to moderate valgus deformity (with a misalignment angle of the 1st and 2nd metatarsal bones of no more than 17 degrees). A good result occurs in the absence of pronounced changes in the head of the metatarsal bone. Technique of operation. A Y-shaped incision is made in the joint capsule (the so-called “champagne access”). Then the outer surface of the metatarsal head is released from the tendon. Then follows the main stage of the operation - a V-shaped cut is made, which separates the head of the first metatarsal bone. Next, the head is shifted outward and fixed with a screw or suture material. The remaining protruding bone is excised. Subsequently, the joint capsule is restored, the medial collateral ligament is stabilized and sutures are placed on the skin. Rehabilitation. After Austin's operation, the patient is allowed to walk almost the next day, but only with emphasis on the heel and in shoes with hard soles. Of course, physical activity should be limited after surgery. You can walk in regular shoes after 1.5 months. Patients feel completely healthy after 3-4 months. In rare cases, recovery can take up to 9 months. Swelling in the surgical area persists for a very long time (increased blood circulation and formation of callus). What complications occur after chevron osteotomy If we talk about rare but very dangerous diseases that are not specific to surgery and traumatology: infectious complications, nerve trauma and deep vein thrombosis. When it comes to specific complications of Austin's operation, they talk about incorrect positioning of the metatarsal head after surgery. It is extremely rare that a repeat operation is required. In less than 3% of patients, circulatory disturbances in the metatarsal head are described. The consequences of this are very different. And further. When the joint capsule is weakened, another condition that is difficult to correct is possible - hallux varus (hallux valgus on the contrary)
Operation Ludloff and operation Mau (operation Mau)
The Ludloff procedure is a surgical technique that can be used for mild hallux valgus. The technique was first applied and described by its author in 1918. The technique is based on a wedge-shaped cut of the first metatarsal bone and displacement of the distal part of the bone inward. The bone is moved to correct the main problem of valgus deformity - too much angle between the 1st and 2nd metatarsals. At first glance, the Mau operation is distinguished by an insignificant detail: the position of the cut.
The surgical technique involves creating a lateral approach to the metatarsal bone and forming a wedge-shaped defect. The distal metatarsal is then shifted to reduce the metatarsal angle. The bone is stabilized most often with screws and sometimes with a plate. The joint capsule is additionally sutured to reduce valgus deviation. Recovery after Ludloff's surgery is long, at least 6 weeks. This is due to the fact that it is necessary to form a complete bone callus in the area of the operation. After 8-12 weeks, walking in shoes with wide toes is allowed. For many patients, there is permanent swelling in the surgical area, so it is recommended to avoid wearing tight shoes. What troubles can there be? Of course, there are universal ones: infection, wound problems. But it is worth noting the special complications of Ludloff’s operation: - Nerve injury. There is a risk of damage to the nerve on the inner surface of the foot - the internal branch of the superficial peroneal nerve. In addition, it is also possible that the nerve responsible for the first interdigital space (a branch of the deep peroneal nerve) is injured. When damaged, numbness and a strong burning sensation occur. Very rarely, a stable regional pain syndrome occurs. - Slow consolidation or lack of consolidation. The bones simply do not fuse. This happens extremely rare and requires reoperation. - Recurrence of valgus transformation. Sometimes this can happen over time and may require a revision of the surgical technique. - Hallux varus - excessive inward deviation of the big toe. This is a rather unusual complication after the Ludloff procedure. - Restricted mobility of the metatarsophalangeal joint. Cause This complication may include scar changes in the area of the base of the thumb. Treatment is usually conservative, but with severe arthrosis, surgical intervention may be required.
SCARF osteotomy
This operation was proposed in 1926 by Dr. Mayer, but the method has been actively used since the 70s. In Russia, this technique appeared even later: surgeons began to master it only in 2000. The term SCARF itself describes the shape of the bone cut that the surgeon uses during surgery. The term has architectural and carpentry roots and is defined as "a joint made by a groove, a groove, holding two parts together to form a strong, continuous member." To put it simply, this is a way to connect wooden beams without increasing the cross-section. When a similar Z-shaped cut is used in foot traumatology, it is called a SCARF osteotomy.
The big advantage of scarf osteotomy is that it is possible to move the bone fragment in three planes and the doctor’s capabilities in modeling the anatomy are very expanded. An osteotomy involves making a Z-shaped incision into the first metatarsal, which can then be repositioned and secured in its new position. Fixation is usually carried out with two screws. Subsequently, excess bone is removed from the inner surface. During the operation, the collateral ligaments running along the lateral surfaces of the finger are corrected. The operation is often combined with other techniques, for example, osteotomy of the proximal phalanx according to Akin. Recovery from surgery lasts about 6 weeks.
Modern operations using microtools and Tritrope steel wire stabilizers
This is already minimally invasive surgery for Hallux valgus. It is also called “keyhole surgery”. The correction is carried out through 3-4 very small incisions, 3-4 millimeters long. Working instruments are introduced through micro-incisions, including micro-mills for cutting bones. The operation is controlled by fluoroscopy (or through an endoscope camera).
Treatment of recurrent hallux valgus deformity of the first toe with us
Treatment of recurrent hallux valgus is a complex process that requires special knowledge and experience from the doctor. In addition to complex deformation, these patients also have psychological trauma: doubt in achieving good treatment results, mistrust.
Petrosyan Armen Sergeevich is an orthopedic traumatologist who has the necessary experience and tools for diagnosing and treating relapse of hallux valgus using conservative and surgical methods.
The advantages of treating recurrent hallux valgus with us:
- diagnostics are carried out using modern equipment by a highly qualified specialist;
- treatment of relapse of hallux valgus using a conservative or surgical method (use of modern high-tech equipment);
- complete preoperative and postoperative management;
- preventing complications;
- patient consultation at all stages of treatment and recovery.
Don’t waste precious time, make an appointment with a doctor by calling the numbers listed on the pages of the site, and a deformity that seems irreparable will remain a thing of the past for you.