Synovitis of the shoulder joint is an acute or chronic pathology accompanied by inflammation of the synovial membrane. An excessive amount of exudate is produced in the joint cavity, which reduces the functional activity of the shoulder apparatus. Clinically, synovitis is manifested by pain of varying intensity, swelling of soft tissues, and limited range of motion. The causes of the disease are injuries, degenerative-destructive pathologies of the joint, and metabolic disorders. To confirm the initial diagnosis, a number of instrumental techniques are used - radiography, CT, ultrasound. In the initial stages of synovitis of the shoulder joint, conservative treatment is carried out. If complications develop, the patient is prescribed surgery.
Etiology
The most common cause of synovitis is destructive changes in the tissues of the shoulder joint. Its structural elements thicken and become rough, damaging the layers of the synovial bursa. The volume of fluid produced to lubricate the joint surfaces exceeds normal values. Constant “swelling” of structural components leads to the development of an inflammatory process. Sometimes it is provoked by injuries - dislocations, subluxations, fractures, ruptures and sprains of ligaments or tendons. The following external or internal negative factors can become the impetus for the occurrence of pathology:
- excessive physical activity in untrained people;
- bleeding disorders accompanied by bleeding in the joints, for example, hemophilia;
- arthritis, arthrosis, osteoarthrosis;
- a severe allergic reaction with increased sensitivity of the synovial membrane to a certain endogenous chemical compound.
Pathogenic microorganisms penetrating into the joint cavity can provoke the inflammatory process. Pathogenic bacteria infect tissues during injuries with severe damage to the epidermis. These include lacerations, puncture wounds, and cuts. Microbes can enter the synovial bursa from primary inflammatory foci. Therefore, in people with weakened immune systems, the impetus for the development of synovitis of the shoulder joint is respiratory diseases - acute tonsillitis, bronchitis, sinusitis.
Synovitis of the shoulder joint is often diagnosed in athletes who, during training, make monotonous movements with their arms, applying a certain load. These are hockey players, volleyball players, tennis players.
Diagnostics
Several studies help the doctor diagnose synovitis of the shoulder joint. In general, a specialist is already able to identify the disease during a visual examination, palpation and listening to complaints.
To clarify, a puncture is performed. The study of biomaterial allows us to determine the nature and cause of the development of pathology.
Doctors have other informative diagnostic methods at their disposal:
- X-ray;
- biopsy of the synovium;
- Ultrasound;
- Magnetic resonance imaging;
- CT scan;
- arthropneumography.
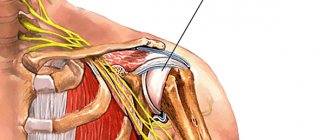
In some cases, arthroscopy is used during the examination. The technique allows you to examine the joint almost bloodlessly by piercing the surface tissue with a needle. A special optical system is inserted into the hole. Thanks to innovative technologies, a specialist has the opportunity to completely examine the joint from the inside and make an accurate diagnosis.
If there is a suspicion that the cause of the pathology is endocrine diseases, allergic reactions, or disruptions in metabolic processes, an examination is prescribed by appropriate specialized specialists.
Classification
Treatments for shoulder synovitis depend on its cause. To facilitate diagnosis, it is determined whether the disease is aseptic or infectious. The first option is more common and occurs as a result of injury, sensitization reactions, endocrine disorders, and diseases occurring against the background of a metabolic disorder. The following classification of synovitis is important for adequate therapy:
- spicy . This form is characterized by serous inflammation, in which exudate with proteins and blood cells is released. The vessels of the synovial membrane become overfilled with fluid. If blood particles appear in the effusion, villous hemorrhagic synovitis is diagnosed;
- chronic _ Rarely accompanied by serous inflammation alone. Usually, a serous-fibrinoid form of synovitis is detected, in which exudate with a high concentration of fibrin (high molecular weight, non-globular protein) is formed. Gradually, its fibers become compacted with the formation of free intra-articular bodies.
View through an arthroscope.
In the acute form of the pathology, no changes occur in the capsular membrane, but in chronic synovitis, its functional activity decreases as a result of the accumulation of fibrin. The acute course of the infectious disease is accompanied by the appearance of pus in the exudate. There is a specific synovitis, the cause of which is Treponema pallidum, Mycobacterium tuberculosis, and gonorrhea pathogens. The development of nonspecific pathology is provoked by streptococci, Escherichia coli and Pseudomonas aeruginosa or staphylococci.
The National Association of Traumatologists has released statistics on the most common location of synovitis. Ahead were acute and chronic pathologies of the knee joint. Synovitis of the shoulder joint ranks second in terms of distribution and severity.
Which doctor treats synovitis of the shoulder joint?
To treat shoulder synovitis, you need to consult a rheumatologist.
An arthrologist and an orthopedist also treat joints. To improve the effectiveness of therapy, other highly specialized specialists are often involved in the process. Allergists, surgeons, massage therapists, and physiotherapists come to the aid of a patient with synovitis of the shoulder joint. If a person only assumes a diagnosis, then he can seek help from a therapist. The doctor will examine the patient and, if necessary, refer to a specialist.
Clinical picture
The main symptom of acute synovitis of the shoulder joint is pain, the intensity of which increases with movement. Excessive accumulation of exudate leads to swelling of the joint. The severity of pain increases in the morning and gradually decreases in the evening due to the production of hormones. The acute form of pathology is also characterized by the following symptoms:
- limitation of range of motion in the shoulder apparatus;
- redness of the skin in the area of inflammation of the shoulder.
With purulent synovitis, symptoms of general intoxication of the body develop. During the day the temperature rises above 38.5 °C several times. The patient develops chills, fever, and increased sweating. Against the background of hyperthermia, digestion and peristalsis are upset, there is often a complete loss of appetite, headaches, weakness, and psycho-emotional instability occur. The person requires urgent medical attention, otherwise serious complications may develop.
In the absence of medical intervention, synovitis takes a chronic course. With this form of the disease, clinical manifestations are often completely absent. A person may be concerned about:
- slight morning swelling of the shoulder;
- stiffness of movements.
But at this time the processes of tissue destruction in the joint accelerate. Gradually, the severity of symptoms increases, and painful relapses occur more often.
Protracted forms of chronic synovitis rarely respond to conservative treatment. The synovial membrane has undergone irreversible changes. It formed hypertrophied villi and (or) focal deposits of calcium salts in areas of pronounced dystrophic changes. Patients are prescribed a surgical operation - partial, subtotal or total synovectomy.
Symptoms
Reactive synovitis of the shoulder manifests itself differently in the acute and chronic stages. The disease can be easily confused with other pathologies of joint joints. However, there are signs that should alert you and make you see a doctor.
Let's look at them:
- The shoulder joint swells and a feeling of heat appears.
- Discomfort or pain when pressing, palpating, or moving your hands.
- The appearance of rashes in the area around the affected joint.
- Synovitis of the left shoulder joint gives the feeling that the heart hurts.
Swelling during synovitis manifests itself to an insignificant extent. The swelling does not have clear boundaries. Palpation makes it possible to understand that the joint has increased in volume and acquired a rounded shape.
The nature of the pain depends on the clinical picture. Regardless of its form, the disease makes hand movements painful. The person is in pain even at rest. Unpleasant sensations intensify at night.
The advanced pathological process leads to the fact that fibrous tissue begins to form in the joint capsule. After this, the symptoms change somewhat. In addition to pain, heat, swelling, the joint loses its functionality. Movements become constrained.
The disease can be distinguished from bursitis by the presence of a rash in the joint area. This is one of the characteristic symptoms of all synovitis.
Diagnostic techniques
The diagnosis is based on the patient’s complaints and objective instrumental studies of the damaged shoulder joint. The most informative methods are:
- radiography. Allows you to identify the inflammatory process in the synovium, visually determined by the excessive volume of exudate. The diagnosis is confirmed by the size of the joint space and the changed surfaces of the shoulder joint. Doctors order the patient to have an X-ray of the diseased and healthy shoulder for comparison;
- ultrasonography. Ultrasound is performed to determine the thickness of the synovial membrane and the volume of exudate filling the joint, and to identify changes in the condition of the periarticular tissues.
The most preferred research method is joint puncture, which is performed to collect exudate for laboratory analysis. Further research will help establish the species of infectious agents and their sensitivity to antibiotics.
Classification features
Synovitis of the problematic joint often affects one side. In certain diseases, bilateral damage is recorded - in rheumatoid or bacterial forms of arthritis, acute rheumatism.
The pathological process occurs with a purulent or serous variant:
- Jet;
- Acute
- Chronic in nature.
The constantly present form can be provoked by a variety of factors:
- Lack of elimination of the primary source of irritation and further progression of the disease with periodic relapses;
- Incorrect puncture of the affected joint;
- Violation by the patient of the rest regime and immobilization of the joint, as a result of which complete absorption of the accumulated fluid does not occur.
The process undergoes a phased transition in three main stages:
- Initial – with the appearance of reactive irritation and redness in the synovial surfaces. The amount of swelling and spontaneous accumulation of synovial fluid in the affected joint is insignificant.
- Secondary - with constant exposure to irritants (traumatic, infectious or other types), a gradual transition to the serous form occurs, with the formation of an effusion of the same name. The inner surface of the joint swells significantly, its covering becomes velvety, with increased villi. Blood rushes to the site of injury. The exudate acquires a yellow tint and fibrin clots are found in it. A diagnostic study of the problem area records infiltration at the cellular level and division of synovial cells.
- Tertiary or purulent - the level of blood filling of the vessels increases, the progression of the anomaly is accompanied by hyperemia. Further thickening of the synovial surfaces occurs and their impregnation with purulent contents. In the joint fluid there is a mixture of fibrin flakes with pus.
Methods of conservative therapy
In rheumatology and traumatology, complex treatment of synovitis of any location is practiced. At the initial stage of therapy, the affected joint is immobilized. For fractures and dislocations, the patient is recommended to wear a bandage with rigid inserts that restricts movement. For minor injuries, fixing bandages of medium rigidity are used.
When examining a patient, swelling of the affected shoulder is most often detected. To eliminate the symptom, the excess amount of exudate accumulated in the joint is removed using a puncture. The treatment procedure is carried out at the diagnostic stage when a sample is taken for analysis.
| Group of pharmacological drugs for the treatment of synovitis | Name and cost (in rubles) of medicines |
| Nonsteroidal anti-inflammatory drugs | Tablets or capsules: Diclofenac (45), Meloxicam (68), Nimesulide (87), Ketorolac (37) Ointments and gels: Voltaren (220), Fastum (265), Ketorol (280) |
| Chondroprotectors | Tablets or capsules: Structum (1490), Dona (1300), Glucosamine-Maximum (450), Chondroitin-Akos (310) Creams and ointments: Arthro-Active (100) or Shark fat (75) with glucosamine and chondroitin, Honda ( 240) |
| Antibiotics | Tablets or capsules: Azithromycin (140), Josamycin (450), Erythromycin (70), Clarithromycin (450), Amoxiclav (220), Panclave (320), Augmentin (370) |
About the reasons
To understand how to treat bursitis of the shoulder joint (or any other joints), which should become the basis of prevention, you need to understand the cause of the inflammation. There are several of them (main ones) and most often their complex action leads to inflammation.
The main causes of shoulder bursitis:
- Shoulder injuries - fractures, dislocations, or simply bruises and wounds with or without a violation of the integrity of the joint. They lead to post-traumatic bursitis, the main principle of treatment of which is rest and immobility. Of particular danger are open joint injuries, in which harmful microflora (staphylococcus and other microorganisms) can easily penetrate inside.
- Constant overexertion and heavy physical stress on the shoulders.
- Diseases of the musculoskeletal system - arthritis, rheumatism and others.
- Autoimmune diseases – scleroderma, lupus and others.
- Allergy.
- Metabolic disorders in which joint nutrition deteriorates or salt deposits occur - gout and others.
There is a group of risk factors - reasons that lead to an increased chance of joint inflammation:
- Profession, work associated with constant or heavy load on the joint - loader, athlete.
- Intoxication of the body from smoking, alcohol abuse.
- Weak immunity.
- Patients taking certain medications for a long time and after corticosteroid therapy.
Nonsteroidal anti-inflammatory drugs
To reduce the severity of symptoms, patients are recommended to take systemic non-steroidal anti-inflammatory drugs. They are used 2-3 times a day in dosages prescribed by the attending physician. The duration of the therapeutic course is 7-10 days. The following drugs have proven themselves to be effective in the treatment of synovitis:
- Diclofenac;
- Meloxicam;
- Ibuprofen;
- Ketorolac;
- Nimesulide.
NSAIDs quickly relieve inflammation and pain by preventing the production of prostaglandins. The high effectiveness of the drugs is offset by their pronounced adverse reaction - ulceration of the gastric mucosa. Combining them with proton pump inhibitors, such as Omeprazole or Pantoprazole, helps to minimize such consequences of taking NSAIDs. As the pain intensity decreases, non-steroidal anti-inflammatory drugs in tablets are replaced with ointments, gels or creams. The greatest therapeutic effectiveness is typical for external agents Voltaren, Fastum, Dolobene, Diclovit. Ointments are applied to the area of inflammation and pain 2-4 times a day.
Chronic synovitis in rheumatology. Assessment of activity and treatment tactics
About the article
61422
0
Regular issues of "RMZh" No. 8 dated April 29, 2005 p. 548
Category: General articles
Author: Olyunin Yu.A. 1 1 FGBNU NIIR im. V.A. Nasonova, Moscow, Russia
For quotation:
Olyunin Yu.A. Chronic synovitis in rheumatology. Assessment of activity and treatment tactics. RMJ. 2005;8:548.
Among the various manifestations of chronic joint diseases, synovitis occupies a leading place. The inflammatory process developing in the synovium determines the main features of the clinical picture and is the driving force behind the progression of the disease. It is the body’s response to a pathogenic stimulus, which is realized through the transformation of the synovium into a kind of immune defense organ. In this case, functionally active cells of inflammatory infiltrates are formed not due to the local proliferation of the initially present cellular elements, but as a result of the migration of the corresponding cells from the circulation.
This process leads to the formation of highly specialized cellular aggregates, the components of which actively interact with each other and produce aggressive products that cause tissue damage. The formation of inflammatory cell infiltrates is accompanied by proliferation of stromal elements and blood vessels of the synovium. Over time, the thin shell of the joint turns into a fairly powerful tissue mass. The structure and functional activity of such tissue varies in different diseases, in different patients suffering from the same disease, in different joints of the same patient, and even within the same joint. The most common types of chronic synovitis are primary inflammation of the synovium in chronic arthritis and secondary synovitis in patients with osteoarthritis (OA). According to modern concepts, the key link in the development of chronic arthritis is the recognition of an unknown pathogenic factor by the antigen-presenting cell [4]. The cell that recognizes the antigen processes it and presents it to the T lymphocyte, triggering the synthesis of proinflammatory cytokines that induce the migration of inflammatory cells into the joint and the proliferation of synovial vessels. The development of secondary synovitis in OA is associated with the accumulation of cartilage degradation products (fragments of proteoglycan and collagen molecules, chondrocyte membranes, etc.) in the joint [6]. Normally, cells of the immune system do not come into contact with these antigens and therefore recognize them as foreign material. This leads to the development of an immune response, accompanied by chronic inflammation of the synovium. The morphological picture of secondary synovitis as a whole is not fundamentally different from those changes that are observed in chronic arthritis. Active synovitis in patients with chronic arthritis is accompanied by the production of proteolytic enzymes that mediate joint destruction. Chronic synovitis in OA is itself the result of a destructive process. However, it, in turn, can aggravate joint destruction [1]. Therefore, suppression of the chronic inflammatory process, apparently, can slow down the progression of the disease not only in chronic inflammatory joint diseases, but also in OA. The basis for the treatment of inflammatory changes in the joints is systemic drug therapy. However, often systemic treatment does not adequately suppress local inflammatory activity and synovitis occurs as a relatively autonomous process, which is supported mainly by local mechanisms. In such cases, a favorable result can be achieved with the help of therapeutic measures aimed directly at the source of inflammation. At the same time, the tactics of therapeutic measures are largely determined by the activity of the inflammatory process. The main clinical signs of the activity of chronic inflammation of the synovial membrane are arthralgia and swelling of the affected joint. These symptoms are equally characteristic of both primary and secondary synovitis. The formation of pain syndrome in inflammatory and degenerative joint diseases can be associated with various mechanisms. But the main role among them is probably played by irritation of the nerve endings located in the joint under the influence of inflammatory mediators produced here. Joint pain is the leading symptom of the disease, and the functional limitations that develop in the patient are primarily associated with it. Currently, there are two main ways to record the intensity of pain. The simpler of them is the assessment of arthralgia in points, which usually provides 5 degrees of severity of the symptom (0 - no pain, 1 - mild, 2 - moderate, 3 - severe and 4 - very severe pain). It is somewhat more difficult to assess pain using a visual analogue scale (VAS), but this method provides more accurate results. VAS is a straight line 100 mm long. The zero point of the scale located on its left edge means no pain. The far right point corresponds to unbearable pain. Between these extreme positions, the patient must indicate the level corresponding to his pain sensations. It should be borne in mind that pain is a dynamic indicator, the severity of which varies depending on the time of day and the physical activity of the patient. Therefore, it is not the intensity of pain at the time of examination that should be recorded, but its maximum level over the past week. The exudative component of inflammation is not as noticeable for the patient as pain, but is of exceptional importance as an objective indicator of the activity of synovitis. The presence of exudate in the cavity of the affected joint is necessarily taken into account when determining treatment tactics and assessing the effectiveness of the therapy. When examining a patient, as a rule, one can quite reliably judge the presence or absence of exudate in those joints that are sufficiently accessible for visual and palpation examination (knees, wrist elbow joints, small joints of the hands and feet). It is quite difficult to detect moderate accumulation of exudate in the ankle and shoulder joints. It is not possible to detect fluid in the hip joints without the help of instrumental research methods. In order to reliably estimate the amount of exudate, it must be evacuated from the joint cavity. You can roughly assess the severity of the exudative component of arthritis by measuring the circumference of the inflamed joint. For short periods of observation, the dynamics of this indicator can be taken into account when assessing the effectiveness of treatment. However, in cases where the result is assessed at a sufficiently long term, a decrease in the circumference of the joint can occur due to atrophy of the muscles located in this area. Therefore, when examining a patient, qualitative registration of the presence or absence of exudate provides more reliable data than an attempt to quantify it. Additional information about the nature of changes in the affected joint can be obtained using instrumental research methods. The most common of these is radiography. However, a standard x-ray examination allows us to evaluate not the features of the development of synovitis, but its consequences. It makes it possible to determine, first of all, the degree of destruction of the joints, to record the presence of subluxation, aseptic necrosis of the bone or ankylosis of the joint. Ultrasound can be used to visualize the inflamed synovium itself. It allows you to obtain an image of a section of the joint under study, made in a certain plane. Using such a section, you can accurately measure the thickness of the synovial membrane, as well as approximately estimate the amount of synovial fluid in a given part of the joint. Ultrasound provides the ability to semiquantitatively assess exudative changes. The degree of accumulation of exudate in a certain part of the joint can be expressed in points and then the dynamics of this indicator can be monitored against the background of the treatment. The thickness of the synovial membrane, which can be recorded by ultrasound, is also one of the signs of synovitis activity. Its value is largely determined by inflammatory edema and decreases significantly as inflammation subsides. The use of arthroscopy (AS) allows direct visual examination of the inflamed synovium of the affected joint. Unlike ultrasound, AS does not allow one to accurately measure the thickness of the inflamed synovium and assess the severity of exudative changes in a given part of the joint. These two methods do not replace, but complement each other. Arthroscopic examination of the joint makes it possible to study the relief of the synovium along its entire length. Depending on the duration of synovitis and the characteristics of its development in a given joint, changes in the synovial membrane can vary within a very wide range. Normal synovium in the form of a thin transparent film covers the joint capsule. The development of the inflammatory process is accompanied by its thickening, the appearance of hyperemia, proliferation of villi, and the formation of fibrin clots on its surface. AS allows for a differentiated assessment of the nature of joint damage in patients with a similar clinical picture of the disease. To record observed changes, several methods for their semi-quantitative assessment have been proposed. Zschabitz A. et al. assessed the morphological changes in the synovium identified in AS using an index, which was calculated according to 4 indicators: vascularization, hyperemia, swelling of the synovium and villi formation [10]. The severity of each indicator was determined in points from 0 to 3. This scheme allows you to record the severity of changes, but does not take into account their prevalence, so it is difficult to characterize the damage to the joint as a whole. Paus AC et al. tried to overcome this drawback [9]. They divided the joint into 5 regions (posterior, intercondylar, medial, lateral, suprapatellar). In each zone, the severity of the lesion was assessed in 4 degrees: 1 - no signs of synovitis, 2 - moderate hyperemia without villi formation, 3 - moderate hyperemia with moderate villi formation, 4 - moderate or severe hyperemia with massive villi formation. The overall index was the arithmetic average of the scores of the 5 specified areas. The American College of Rheumatology has proposed assessing the severity of hyperemia, thickening, and villous proliferation of the synovium using a visual analogue scale and simultaneously recording the extent of the lesion as a percentage of the total area of the synovium. It should be noted that one of the most significant parameters characterizing the development of chronic synovitis may be the degree of increase in the volume of the affected synovium, an indicator of which is the severity of its villous proliferation. As it progresses, the size of the inflammatory focus increases, which, on the one hand, leads to a change in the ratio between the amount of drug injected into the joint and the mass of the affected tissue, and on the other hand, it impairs the circulation of fluid in the joint and makes it difficult for the drug to enter the inflammatory zone. There are 4 degrees of proliferative changes in the synovial membrane of the knee joint. The first is thickening of the synovium without significant villous proliferation. The second can be defined as the appearance of focal accumulations of villi against the background of a thickened synovium. In the third degree, the villi cover most of the synovium of the lateral parts of the joint, leaving the upper part free. The fourth degree is characterized by diffuse villous proliferation, which covers all parts of the joint. Arthroscopic control could be of some interest for assessing the results of treatment of chronic arthritis. Judging by the data from publications that assessed the effectiveness of intra-articular injections of drugs (in particular, methotrexate and rifampicin), the most dynamic indicator is synovial hyperemia [8]. It clearly decreases with a decrease in clinical signs of inflammation. At the same time, the structure of the synovia is generally quite stable. When examining patients before and after radiosynovectomy, we also observed the disappearance of hyperemia with favorable clinical results. In addition, in some cases, areas of synovial sclerosis and fatty degeneration of synovial villi appeared. While clinical signs of active inflammation persisted, hyperemia of the synovial membrane persisted in all cases. The tactics of local treatment of chronic synovitis is determined by the activity of the local pathological process and the effectiveness of previous therapy. In the presence of pain syndrome that is not accompanied by significant exudative changes, both in chronic inflammatory diseases of the joints and in OA, in addition to systemic drug therapy, medications in the form of ointments or gels are usually prescribed. In many cases, a beneficial effect can be achieved by prescribing locally irritating drugs that reduce the severity of pain due to a distracting effect. For this purpose, preparations based on menthol, turpentine, and camphor are used. The use of ointment and gel products containing nonsteroidal anti-inflammatory drugs (NSAIDs) ensures that these medications are delivered through the skin directly to the site of inflammation. For this purpose, medications containing such powerful agents as indomethacin, diclofenac, ibuprofen, and piroxicam are widely used. They are usually used 3-4 times a day, squeezing 4-8 cm out of the tube, depending on the size of the affected joint. Often, the optimal effect can be achieved using combination drugs containing ingredients with different mechanisms of action. One such successful combination is Dicloran Plus. It contains three anti-inflammatory components (diclofenac, methyl salicylate, linseed oil) and menthol, which has a local irritant effect. Menthol has a so-called “cooling” effect - due to irritation of cold receptors. A number of drug studies have shown that “cooling” gels containing menthol have significant analgesic activity and help to shorten the period of swelling and dysfunction when compared with placebo. Diclofenac and methyl salicylate are among the classic NSAIDs that achieve their effect by inhibiting the activity of cyclooxygenases, leading to a decrease in the synthesis of prostaglandins, which reduces swelling and infiltration of inflamed tissues. At the moment, according to FDA (USA) experts, only drugs containing methyl salicylate, menthol and capsaicin can be considered undeniably effective as analgesics. A-linolenic acid, which is part of flaxseed oil, binds activated cyclooxygenases at the site of inflammation. In the presence of significant exudative manifestations of the inflammatory process, the method of choice is intra-articular injection of GC. It is also practiced for both inflammatory and degenerative joint changes. It should be noted, however, that secondary synovitis is generally more resistant to the action of hormones and clinical improvement is often not long-lasting. For injection into joints, microcrystalline suspensions of poorly soluble hormonal drugs are used, which can be deposited in the affected joint for up to 3 weeks. As a result of the gradual dissolution of hormonal compounds deposited in the joint, a constant supply of a sufficient amount of medicine directly to the site of inflammation is ensured. The effect of GCs introduced into the joint cavity is mediated by interaction with the corresponding receptors of cells infiltrating the synovium and participating in the development of synovitis. The effect of HA on joint tissue largely depends on the dose and frequency of administration. Frequent injections of high doses of hormones in the experiment contributed to the development of degenerative changes in articular cartilage. At the same time, sporadic intra-articular injections of these drugs may have a chondroprotective effect. Therefore, in clinical practice, the injection of HA into the same joint is allowed no more than 3–4 times a year. The number of injections into different joints is not particularly regulated. However, they should not be performed too often and regularly. Otherwise, local therapy will actually become an analogue of systemic hormonal treatment, since the drug is constantly absorbed from the joint cavity into the bloodstream and provides, in addition to local, a noticeable systemic effect. The anti-inflammatory effect of GCs introduced into the joint is usually quite pronounced. The duration of the improvement achieved can vary within very wide limits. It depends both on the properties of the drug and on the characteristics of the course of inflammation in each specific case. The effectiveness of the drug directly depends on the solubility of the microcrystalline suspension. Reduced solubility increases duration of action and increases effectiveness. Currently, triamcinolone compounds (hexacetonide and acetonide) have the most long-lasting effects [3]. The lack of effectiveness of intra-articular injections in many cases may be associated with relative resistance to the action of GCs due to the production of a large number of pro-inflammatory cytokines at the site of inflammation. To avoid the unwanted effects of inflammatory stimulants that accumulate in the joints during chronic synovitis, the exudate is removed before administering the drug. However, proliferative changes forming in the joint and fibrin clots often prevent the full evacuation of the synovial fluid. Therefore, in a number of cases, it is not possible to completely remove it with a joint puncture and the pro -inflammatory factors remaining in the joint cavity impede the effect of the drug. The almost complete removal of inflammatory exudate can be achieved when the joint washes with a large amount of fluid during the AC. This method provides sufficient fluid intake into all parts of the joint and free evacuation of the contents of the joint cavity. In most patients with chronic arthritis, the joint washing with AS already in itself ensures a significant decrease in inflammatory changes. However, this effect is usually unstable. Introduction after washing the Civil Code gives significantly more favorable results. The clinical improvement achieved with intra -articular administration of the Civil Code after the AC is longer in most patients than with traditional local steroid therapy. We evaluated the effect of pre -washing the joints with AC on 55 knee joints of patients with RA. In 27 of them, the Civil Code was introduced in the traditional way after removing the exudate. 28 Before the introduction of the Civil Code were washed at the AC. 3 and 6 months after treatment, the decrease in arthralgia in these patients was significantly more significant than in the control group. A significant decrease in pain in the knee joints is observed after AS and in patients of OA [5]. Moreover, in contrast to chronic arthritis, the introduction into the joint of the Civil Code after AS in patients of the OA is not required. This phenomenon was noted even more than 50 years ago and is due, apparently, by a decrease in inflammatory changes characteristic of this disease. Rinsing the knee joints with AS allows you to remove the bulk of cartilage detritus and crystals from them. The elimination of these stimulants of inflammation can lead to a decrease in synovitis activity and a decrease in the severity of pain. It is also possible that such treatment can reduce the production of enzymes involved in the development of joint cartilage destruction, thereby slowing down the progression of the disease. The clinical effect of the AC largely depends on the technical features of its implementation. Thus, the authors who studied the results of the AC when using various volumes of fluid for its conduct, note that washing the knee joints with 3 liters of liquid gave a more favorable effect than 250 ml. The amount of detrit, removed during the procedure, also correlates with the degree of reduction in the severity of pain syndrome [7]. The favorable effect observed in patients with the joints after washing the joints at the AC prompted some researchers to use a simplified rinse procedure using puncture needles for the treatment of this disease. The results of such treatment are evaluated ambiguously. According to some authors, this procedure is no less effective than washing the joints with AS and gives a longer clinical improvement than the intra -articular introduction of the Civil Code. Others believe that it does not differ significantly from placebo [2]. Probably, in patients of the OA, as in chronic arthritis, the effect of washing largely depends on its technical characteristics. AS allows you to achieve significantly more complete removal of cartilaginous detritus and crystals from the cavity of the affected joint than washing through puncture needles. Therefore, despite the greater technical complexity, this procedure seems more promising than a simplified washing option. Literature 1. Panasyuk E.Yu., Tsvetkova E.S., Olyunin Yu.A., Smirnov A.V. Arthroscopy in the diagnosis of gonarthrosis. Scientific and practical rheumatology 2000, No. 2, p. 12–17. 2. Bradyy JD, Heilman DK, Katz BP, GSELL P, WALLICK JE, Brandt KD. Tidal Irrigation As Treatment for Knee Osteoarthritis: A Sham - Controlled, Randomized, Double - Blinded Evaluation. Arthritis Rheum. 2002 Jan; 46 (1): 100–8. 3. Centeno LM, Moore Me Preferred Intraarticolar Corticosteroids and Associated Practice: A Survey of Members of the American College of Rheumatology 4. Choyi Ehs, Panayi Gs Cytokin E PathWays and Joint InflamMatio in Rheumatoid Arthritis. New England Journal of Medicine, 2001, 344, 12, 907–916 5. Edelson R, Burks RT, BloEbaum RD, Short - Term Effects of Knee Washout for OsteartHritis. Am J Sports Med 1995, 23 (3), 345–9 6. Ghosh P, Smith M. Osteoarthritis, Genetic and Molecular Mechanisms. Biogerontology, 2002, 3, 85–88 7. Kalunian KC, Moreland LW, Klashman DJ, Brion PH, Concoff Al, Myers S, Singh Rw, Seeger LL, Rich E, Skovron Ml. Visually - Guuided Irrigation in Patience with Early Knee Osteoarthritis: A Multicenter Randomized, Controlled Trial. Osteoarthritis Cartilage. 2000 nov; 8 (6): 412–8. 8. Lindblad S., Hedfors E., Malmborg As Rifamycin SV in Local Treatment of Synovitis - A Clinical, Arthroscopic and Pharmacolagical Evaluation. J. RHEUMATOL. 1985, 12, 5, 900–903 9. Paus Ac, Pahle Ja Arthroscopic EvalUration of the Synovial Lining Before and Inter Open Synovence of the Knee Joint In Patys with Chronic INFLAMATORY JOIN T Disease. Scand J. Rheumatol. 1990, V. 19, p. 193–201. 10. Zscchabitz A., Neurath M., Grevenstein J. et al. Correlative Histologic and Arthroscopic Evalving in Rheumatoid Knee Joints. SURG ENDOSC. 1992, V. 6, p. 277–282.
Content is licensed under a Creative Commons Attribution 4.0 International License.
Share the article on social networks
Recommend the article to your colleagues
Antibiotic therapy
Antibacterial drugs are prescribed when diagnosing infectious synovitis. Preference is given to antibiotics from the macrolide group - Azithromycin, Josamycin, Erythromycin, Clarithromycin. To prevent a decrease in the sensitivity of microorganisms to the action of antibiotics, patients are prescribed semisynthetic penicillins:
- Amoxiclav;
- Panclave;
- Augmentin.
They contain a therapeutically inert compound - clavulanic acid. It prevents pathogenic bacteria from developing resistance to antibiotics. This allows you not to change medications throughout the entire treatment. After antibiotic therapy, patients are recommended to take a course (10-14 days) of eubiotics to restore the intestinal biocenosis.
Chondroprotectors
The use of these structure-modifying drugs helps prevent further destruction of the structural elements of the shoulder joint. Medicines are intended for long-term use over several months and sometimes years. After several weeks of regular use, chondroprotectors accumulate in tissues and begin to have anti-inflammatory and analgesic effects. The doctor gradually reduces the dosage of NSAIDs or glucocorticosteroids that have a toxic effect on the human body.
Chondroprotectors stimulate the production of the body's own chondrocytes. Their use contributes not only to the prevention of destructive and degenerative changes, but also to the gradual restoration of damaged tissues. What medications can the doctor prescribe:
- Alflutop;
- Structum;
- Don;
- Glucosamine-Maximum;
- Chondroitin-Acos.
To accelerate joint regeneration and increase the clinical effectiveness of systemic chondroprotectors, patients are recommended to combine them with ointments and gels. This could be Teraflex or Alezan cream, Arthro-Active or Shark oil with glucosamine and chondroitin, Honda.
Treatment of synovitis with folk remedies is not only inappropriate, but also dangerous. Temporary elimination of painful sensations is not able to stop the development of pathology in the shoulder joint. A timely visit to a doctor will help provide adequate therapy and avoid the development of severe complications.
Prevention
Certain actions cannot be guaranteed to prevent shoulder synovitis. However, taking a responsible attitude towards your health has always been considered the best prevention.
Doctors' recommendations include timely treatment of pathologies of infectious etiology, joint diseases, and moderate exercise. Try not to get too cold, get rid of bad habits and eat right. All this together will make your body stronger.
Author: Tatyana Grosova, nurse, especially for Ortopediya.pro