Osteophytes of the hip joint are bone growths that interfere with the free mobility of the lower limb and provoke the development of pain. The pathology develops gradually and is complex in nature. First, there is a gradual deformation of the cartilage tissue, which is designed to protect the bone tissue of the head of the femur and the acetabulum of the ilium. As the synovial cartilage tissue thins, cracks form on the bones, which are filled with deposits of calcium salts. This is how primary osteophytes arise.
You can find out more information about the causes, symptoms and treatment of osteophytes of the hip joint on this page. If you or your loved ones have the described clinical signs, we recommend that you immediately seek medical help. At an early stage, this pathology can be treated conservatively using manual therapy methods. In advanced clinical cases, surgical removal will have to be performed to remove osteophytes. In some cases, the patient can regain freedom of movement only as a result of hip replacement surgery.
In Moscow, you can make an appointment for a free appointment with an orthopedist at our manual therapy clinic. Experienced specialists work here. They will conduct an examination and make a preliminary diagnosis. They will give all the necessary recommendations for comprehensive diagnostics and treatment.
You can make an appointment directly on this page. At the bottom of it there is a form, filling which you will make an appointment with the selected specialist. You can also call us at the phone number listed on the page. The administrator will agree with you on a time convenient for your visit.
Why do marginal osteophytes of the hip joint develop?
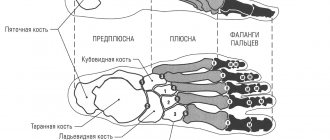
In order to understand in detail the question of why these pathological deposits of calcium salts develop, we suggest first learning some information on the anatomy and physiology of this bone joint.
The hip joint is formed by the head of the femur and the acetabulum of the ilium. All surfaces of the joint are lined with cartilaginous synovial tissue. It has the ability to absorb synovial fluid and release it back when performing various movements. When standing, the acetabulum is subjected to a colossal mechanical load under pressure from the body. When walking, the shock-absorbing load shifts according to the movement vector. Thus, a varied, multidirectional load is exerted on almost all surfaces of the femoral head and acetabulum.
Marginal osteophytes of the hip joint begin to develop only if the integrity of the cartilaginous synovial layer is disrupted. In places where bones are exposed, microscopic cracks form during active movements. They are filled with deposits of calcium salts. These formations injure nearby soft tissues, provoking a constant process of inflammation. Against this background, accelerated destruction of cartilage tissue occurs and osteophytes spread over the entire inner surface of the joint.
Risk factors that are highly likely to provoke the growth and development of osteophytes in the hip joint:
- excess body weight, each extra kilogram greatly increases the load on the articular surfaces and provokes the rapid destruction of cartilage tissue;
- maintaining a sedentary lifestyle (those patients who are engaged in sedentary work are especially at risk);
- incorrect placement of the foot, curvature of the legs and hips, valgus deformity of the foot;
- injuries in the upper thigh and joint area;
- lumbosacral osteochondrosis, in which the innervation of the tissues of the bone articulations is affected;
- poor posture and curvature of the spinal column, resulting in improper distribution of shock-absorbing load when the body moves;
- heavy physical labor associated with prolonged standing, lifting and carrying heavy objects;
- pathologies of the vessels of the lower extremities (atherosclerosis, obliterating endarteritis, varicose veins, diabetic angiopathy, etc.);
- rheumatoid lesions of cartilage tissue inside the joint (rheumatoid arthritis, gout, articular form of ankylosing spondylitis, systemic lupus, etc.);
- improperly composed diet and insufficient consumption of clean drinking water during the day.
Very often, osteophytes are a consequence of improper treatment of complex combined fractures of the pelvic bones. In older people, they can occur after a crack in the femoral head. In middle age, various endocrine pathologies that can lead to the destruction of cartilage tissue should be excluded. The risk group includes pregnant women - in the later stages of pregnancy, they experience physiological softening of all cartilaginous tissues. And against the backdrop of an ever-increasing physical mass of the body, there is an accelerated destruction of the cartilage tissue covering the articular surfaces.
During the initial diagnosis, after detecting cornerstone osteophytes of the hip joint, the doctor excludes bone tuberculosis and various tumor processes. In approximately 10% of patients, these processes can be triggered by hereditary factors.
Causes and symptoms
Factors that increase the risk of developing osteoarthritis and osteophytes are:
- heredity;
- hard work;
- sports activities;
- injuries;
- passive lifestyle;
- excess weight.
For a long time, osteophytes are asymptomatic. But as the pathology grows, they begin to compress the nerve endings, causing pain and restriction of movement. And due to compression of blood vessels, normal blood circulation is disrupted. Large osteophytes can cause inflammation of bone and muscle tissue.
Types of pathology
Various types of bone growths are diagnosed. Varieties of osteophytes are classified according to the place of their formation and etiological factors. Most often, modern people experience the following types:
- metaplastic post-traumatic - occur in places of fractures, cracks, chips of bone tissue, the risk of their formation increases if the rules of immobilization of the limb are violated after the discovery of a traumatic violation of the integrity of the bone;
- compact bone growths accompany the development of deforming osteoarthritis;
- osteochondral osteophytes can form in people experiencing serious physical overload (most often women over 40 years of age who are significantly overweight suffer);
- periosteal osteophytes occur in areas of aseptic and infectious inflammatory processes; they are often found after necrosis of the femoral head;
- degenerative dystrophic growths of bone tissue often accompany osteomalacia and osteoporosis and occur in women during menopause;
- massive tumor growths of bone tissue often have a metastatic nature and accompany various oncological pathologies.
Less common are endocrine and diabetic bone growths. Post-traumatic osteophytes of the hip joint are in first place in terms of frequency of diagnosis at a young age.
Clinical symptoms of hip osteophytes
The clinical picture largely depends on the location, size and shape of the osteophyte. If it is located in the acetabulum, then the movement of the hip in the frontal plane will be limited. Damage to the bone tissue of the femoral head produces symptoms such as crunching and creaking when moving.
Classic symptoms of osteophyte development in the hip include:
- pain of varying intensity, significantly increasing with movement or any physical activity;
- limitation of mobility (impossibility to abduct the leg, bend or perform a rotational movement in the usual range of mobility);
- the appearance of extraneous sounds when making movements (creaking, clicking, crunching);
- periodic inflammation of the soft tissues around the joint (redness of the skin, swelling, pain on palpation);
- change in the position of the femoral head in the cavity of the acetabulum;
- cramps in the leg muscles in the evening and at night.
At a late stage of the disease, symptoms of osteophyte of the hip joint may be accompanied by difficulties with movement. A characteristic change in gait appears; a significant shortening of the limb on the affected side can be detected with the naked eye.
A series of x-rays is sufficient to make an accurate diagnosis. They will show changes in the joint space, deformation of bone tissue, and the proliferation of osteophytes. For the purpose of differential diagnosis, CT, MRI, ultrasound, examination of blood vessels, blood tests, etc. are prescribed.
Methods for diagnosing coxarthrosis
An orthopedist, rheumatologist, and surgeon are involved in the diagnosis and treatment of pathology. A set of laboratory and instrumental methods is carried out to accurately determine the diagnosis.
Radiography
Thanks to the study, the stage of development of the pathological process is determined. The pictures show the changes:
- destruction of the hip joint;
- narrowing of the joint space;
- deformation of the articular surface of the bones;
- osteophytes.
The picture is taken only in 1 projection, so it is difficult to determine the full picture.
CT scan
Different projections of the articular cavity and surrounding tissues are determined. Changes are detected:
- degree of thickening of the bone structure;
- damage to hyaline cartilage;
- condition of the ligamentous apparatus, tendons;
- damage to nerves, muscles, blood vessels during extensive inflammatory processes and bone destruction.
CT is a method that simultaneously determines the condition of hard and soft tissues.
Magnetic resonance imaging
The affected area is scanned layer by layer. The doctor determines the condition of the joint, ligaments, muscles, nerves, blood vessels, and bones. This is the most informative method for diagnosing diseases of the musculoskeletal system. Violations are detected:
- difficulty in blood supply to tissues using MRI with the addition of a contrast agent;
- degree of damage to bones and ligaments;
- proliferation of fibrous tissue.
Doctors advise that if coxarthrosis is suspected, an MRI should be performed, but it is not available in all clinical institutions.
When to see a doctor
Coxarthrosis is a rather serious and, most importantly, irreversible disease of the hip joints; if not treated in a timely manner, it can threaten a person with complete disability.
The first manifestations of coxathrosis often do not cause concern in the patient. A slight pain in the joint after exercise is attributed to overexertion and fatigue. Usually, after rest, the unpleasant sensations go away and the person calms down, which is completely wrong. Already at this stage you should contact a specialist.
By catching the disease in the first stages and receiving qualified treatment, you can significantly extend the time of full functioning of the hip joints, maintain their performance and improve a person’s well-being.
Treatment of coxarthrosis
Only a doctor can determine whether a person has coxarthrosis. Home treatment requires the patient to fulfill the following requirements:
- Weight loss;
- Balanced diet;
- Maintaining a drinking regime (2 liters of water per day);
- Reducing the load on the joint (cane while walking);
- Performing a complex of exercise therapy.
With the second degree of the disease, the person should be sent to a hospital, since now the treatment methods will be more intensive. In addition to medications, laser therapy, ultrasound treatment and electrophoresis will be required. Physical therapy must be carried out under the supervision of a specialist. This stage of treatment is more long-term and relief does not come immediately.
If the disease is already diagnosed at the third stage, or despite the therapeutic measures taken, the patient’s condition has only worsened, more serious measures may be used. At this stage, they resort to surgical methods. The joint is completely replaced with a prosthesis. Endoprosthetics today is a fairly common way to get rid of coxarthrosis.
The dentures take root within one or two months. How quickly this happens is influenced by many factors, including the patient’s age, his physical condition at the time of surgery, and the correct implementation of all doctor’s recommendations. Usually, a prosthesis returns a person to his former mobility, relieves pain, and allows him to lead a normal life. The standard service life of a prosthesis is 15-20 years.
Recovery period
Such a serious operation as endoprosthetics requires patience from the patient during restorative procedures. Restrictions apply during this period:
- Complete cessation of sports activities;
- Elimination of physical stress on the joint;
- Walking only with crutches (2 months);
- Prohibition on dangerous exercises (sudden bending, squats).
In the first days after surgery, all movements should only be under the supervision of medical staff. For good wound healing and implantation of the prosthesis, you must follow all the doctor’s recommendations.
Usually, after full recovery, a person does not experience any particular pain, he can return to his usual lifestyle, play sports, and go hiking.
Advice from experts
Whatever degree of coxarthrosis a person has, it is worth following the general rules:
- After sitting for a long time, take a short walk;
- Do not lie in one position for a long time (on your side or back);
- Perform therapeutic exercises selected by specialists;
- Watch your weight.
How to get rid of osteophytes in the hip joint
Before getting rid of osteophytes in the hip joint, it is necessary to conduct a thorough diagnosis and exclude those pathologies that require special etiotropic treatment. For example, with the development of rheumatoid processes, such as systemic lupus erythematosus, ankylosing spondylitis, rheumatoid arthritis, suppression of the active functioning of the immune system is required. Tuberculosis infection requires special treatment.
Surgical removal of osteophytes of the hip joint is required when the disease is advanced and the cartilaginous synovial tissue in the joint is completely destroyed. In this situation, the only way for the patient to restore his mobility is hip replacement surgery.
In the earlier stages of osteophyte formation, surgery can be avoided. Conservative treatment methods allow you to start the process of reverse development of the osteophyte and restore damaged cartilaginous tissue of the bone articulation.
Diagnosis and treatment
Diagnosis of osteoarthritis and osteophyte is made after a medical examination and radiography.
The osteophyte treatment program depends on the size of the pathology and, accordingly, the severity of symptoms. In some cases, conservative therapy is sufficient (taking non-steroidal anti-inflammatory drugs, manual therapy, physiotherapeutic procedures). If the growth is significant, surgery is indicated. During the intervention, the surgeon removes the osteophyte.
Treatment of osteoarthritis can also be either conservative or surgical. Specific treatment tactics depend on the severity of the disease. Conservative treatment may include taking painkillers and anti-inflammatory drugs, physiotherapy, therapeutic exercises, massages, etc.
Surgical intervention is indicated when other methods do not give the desired effect. To do this, joint endoprosthetics is performed - that is, removing the affected joint and replacing it with an artificial one.
Osteoarthritis and osteophyte can greatly reduce the patient’s quality of life, so when the first symptoms and difficulty in movement appear, do not delay visiting a specialist. Registration for medical appointments is available 24 hours a day.