The famous French surgeon of the 18th century, who took an active part in wars, developed a method of fixation for injuries to the upper limb. In his honor it was named the Deso bandage, which is used to apply the shoulder joint to this day.
Modern traumatology uses it in the classic version and various modifications designed to immobilize the shoulder joint and the entire arm. The Deso bandage is indispensable when you need to provide first aid for an injury; the application technique is simple. Taking into account the high incidence of injuries at work and at home, everyone needs to master it.
Author of the article / Site experts Shulepin Ivan Vladimirovich, traumatologist-orthopedist, highest qualification category
Total work experience over 25 years. In 1994 he graduated from the Moscow Institute of Medical and Social Rehabilitation, in 1997 he completed a residency in the specialty “Traumatology and Orthopedics” at the Central Research Institute of Traumatology and Orthopedics named after. N.N. Prifova.
Features of the Deso bandage
The advantage of fixation is the ability to immobilize the entire upper limb, fixing it to the body, eliminating any movement in all joints. At the same time, wearing a bandage does not lead to compression of the tissues of the arm and disruption of its blood circulation if it is applied correctly.
In addition, an important point is the ease of application and availability of materials.
A wide bandage - gauze or elastic from the first aid kit - is enough to quickly provide assistance to the victim.
Medicine of the world
12/09/2019 admin Comments No comments
To apply the Velpeau bandage, you will need a gauze and elastic bandage. A healthy person makes several rounds around the patient's arm to firmly fix the shoulder joint and collarbone. Wearing is indicated until the moment of visiting a doctor and applying a plaster cast.
The Deso bandage on the shoulder joint itself appeared in the 18th century. It is named after the French surgeon P. Deso. Since then, this tool has been repeatedly improved. Today, the bandage is used not only to immobilize the arm after a fracture or other injuries, but also at the rehabilitation stage to recover from an injury to the collarbone or humerus.
A Deso bandage is applied to tightly fix the injured arm relative to the body.
When should a Deso bandage be applied?
The Deso bandage and its various variants can be used for both first aid and treatment.
Indications for transport immobilization for injuries are:
- shoulder dislocation;
- injuries of the shoulder joint - bruise, sprain and rupture of ligaments;
- collarbone fracture;
- humeral neck fracture;
- fracture of the forearm bones;
- damage to the elbow joint - bruises, sprains and ligament tears.
During treatment, fixation is used in the following cases:
- after surgery for a fracture of the collarbone, shoulder, ligament rupture;
- after closed or open reduction of shoulder dislocation;
- in the initial period of rehabilitation after injuries;
- with acute inflammatory process in the shoulder joint.
University
According to the calendar, it has long been spring, but due to frequent changes in thaws and frosts, pedestrians do not have time to adapt to changes in travel conditions and lose caution. Typical “ice” injuries are fractures of the radius, ankles, and shoulder dislocation.
Classic type fracture
The radius is usually damaged in the distal metaphyseal regions at a distance of 1.5–3 cm from the wrist joint gap.
Most often, the extensor mechanism of injury is observed: when the palm comes into contact with the plane of support, a sudden fixation of the hand and the closely associated articular apparatus of the distal epiphysis of the radius occurs. At the same moment, the very strong (and, as a rule, not susceptible to rupture) palmar ligament is greatly strained. The result is that the thinned compact substance of the bone is injured in this section, and the fracture line begins on the palmar surface of the ray in close proximity to the joint and goes from bottom to top - to the dorsal-ulnar surface. A so-called fork-shaped deformity of the hand and forearm occurs. This injury was described by Colles in 1814 and is called type I. When falling on a hand bent at the wrist joint, a flexion fracture of the radius occurs in the classic place, or a type II fracture (the so-called Smith fracture; described by an Irish surgeon in 1847), characterized by a bayonet-like deformity.
In almost 80% of cases with radial fractures, the styloid process of the ulna is simultaneously separated in a typical location. If there is no displacement of the fragments, immobilization of the limb with a plaster splint, tape cast bandage or orthosis from the proximal third of the forearm to the metacarpophalangeal joints for a month is indicated. A doctor of any specialty must remember that subcutaneous ruptures of the extensor pollicis longus tendon occur from 1 week to 1.5 years after injury. This occurs in 1 case out of 300 radial fractures in a typical location without displacement of the fragments due to chronic trauma in the groove behind the Lister tubercle on the dorsal surface of the bone.
For displaced fractures of the radius, closed reduction of the fragments is performed after adequate anesthesia (local, intravenous, conduction). A fixing bandage is applied on the side of the displaced distal fragment from the upper third of the forearm to the metacarpophalangeal joints.
For type I (Colles) fractures, the hand is given palmar flexion and ulnar deviation - the splint immobilizes the dorsum of the forearm. For type II (Smith) fractures, the hand and forearm are fixed with a splint along the palmar surface, giving the position of dorsiflexion and ulnar abduction.
Control radiography is performed after the plaster cast has hardened and after 6–8 days. After approximately three weeks, it is possible to change the fixing bandage with careful moving of the hand to a functionally advantageous position. And after 5–6 weeks from the moment of fracture, immobilization is stopped and restorative treatment begins.
The most complex category of injuries is represented by intra-articular comminuted fractures of the distal metaepiphysis of the radius. With them, two types of deformation are also observed - on the dorsal and palmar sides.
Simultaneous manual reduction of such fractures is performed according to general rules, but immobilization is carried out to keep the fragments in the reduced state: from the middle third of the shoulder with a supinated forearm to the metacarpophalangeal joints. After four weeks, the elbow joint is released from fixation and, having brought the hand into a functionally advantageous position, additional immobilization is carried out for 2–3 weeks with an orthosis or a plaster (scotch cast) splint.
In some cases, closed reposition of fragments does not provide accurate comparison of multiple fragments. Then, for intra-articular comminuted fractures of the distal metaepiphysis of the radius, the method of choice is open reduction and functional stable osteosynthesis.
"Deza" for Dezo dressing
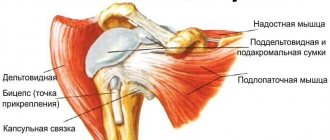
Shoulder dislocations most often occur when falling on an abducted, extended arm. Depending on the direction of displacement of the humeral head, there are anterior (75%), axillary (23%) and posterior (2%). Dislocations are always accompanied by ruptures of the joint capsule, sometimes with tears of the greater tubercle of the shoulder or damage to the rotator cuff.
The patient's injured arm is in a forced abduction position and supported by the healthy forearm. The head is tilted towards the dislocation. On examination, protrusion of the acromion process of the scapula and loss of the normal rounded contour of the shoulder are revealed. Retraction of the deltoid muscle is formed. It is always accompanied by a symptom of springing resistance: during forced adduction, the shoulder takes this position, but as soon as the doctor removes the hand, it returns to its previous forced position. This symptom is the most characteristic, therefore it is important in differentiating the diagnosis from fractures of the shoulder in its proximal part.
Reduction is carried out under full anesthesia using one of the traction techniques (Mukhina-Mota, Dzhanelidze). X-ray examination of the joint before and after reposition is mandatory. After repair of the shoulder dislocation, it is necessary to check the clinical symptoms of possible concomitant damage to the elements of the rotator cuff. If this is not available, the arm is fixed with a Deso bandage for three weeks. The rotator cuff consists of: m. supraspinatus, m. infraspinatus, m. teres minor, m. subscapularis. A rotator cuff tear can occur at any point, but most often occurs at the insertion of the supraspinatus muscle on the greater tuberosity or 1.5 to 2 cm proximally. The most typical symptom for such patients is the “falling arm” symptom: it is impossible to actively move it to a horizontal level and/or hold it in this position. Checked in all cases after reduction of a dislocated shoulder before immobilization. If a rotator cuff tear is suspected or its type and extent is clarified, either an MRI examination or arthroscopy of the shoulder joint is indicated. In case of partial damage (up to 30% of the width), conservative treatment is carried out; in case of extensive ruptures, early surgical treatment is performed.
Healing "boot"
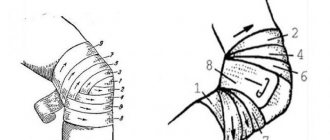
Ankle fractures occur more often after indirect trauma (more than 90%). Usually one of two types occurs: pronation (abduction-eversion), when a traumatic force turns the foot outward, abducts it and pronates, or supination (abduction-inversion) - when the foot turns inward, adducts and supination. If at the time of injury the foot is in a plantar flexion position, a fracture of the posterior edge of the tibia may occur, and in the case of the dorsum, a fracture of the anterior edge of the tibia. Often a subluxation or dislocation of the ankle joint occurs simultaneously.
Treatment is aimed at restoring the disturbed relationships of the elements of the ankle joint. Without precise reduction of fragments, complete elimination of displacement and restoration of contacting surfaces, normal functioning of the joint is impossible. Uncorrected displacement leads to constant pain, severe swelling and rapid progression of deforming arthrosis of the ankle joint.
For isolated fractures of one of the ankles without displacement or subcutaneous damage to the ligaments, treatment is carried out in a deep posterior plaster splint from the upper third of the leg to the tips of the fingers. If the fractures are displaced, then a one-stage closed reduction is performed under local or general anesthesia, and a plaster cast “boot” is applied for up to 10 weeks. The patient is hospitalized in the hospital for further observation due to the threat of compression of the limb by a circular plaster cast. Control radiographs are taken immediately after reduction and after 7–10 days (when the swelling of the limb subsides).
Surgical treatment is indicated for open ankle fractures, in cases of failed closed reduction, as well as in cases of secondary displacement of fragments in a plaster cast. The ankles are fixed using appropriate metal structures. After immobilization, therapeutic exercises, massage, physiotherapeutic procedures are prescribed, and orthopedic insoles or shoes are recommended. Patients' ability to work is restored in approximately four months.
“Clinical signs of an ankle fracture are pain, swelling, changes in joint contours, and dysfunction. As a rule, the patient is not able to lean on the injured leg, but in some cases the limb’s ability to support is preserved, although the load is painful. To clarify the diagnosis, an x-ray of the ankle joint is performed in standard projections. » Alexander Martinovich , Associate Professor of the Department of Traumatology and Orthopedics of the Belarusian State Medical University, Candidate of Medical Sciences. Sciences Medical Bulletin , April 18, 2013
When should you not apply a Deso bandage?
Despite all its advantages, the bandage cannot be applied to open injuries of the upper limb and shoulder girdle, when there is bleeding, measures to stop it and constant monitoring are necessary.
Also, in the case of complex fragment fractures and fracture-dislocations with pronounced displacement and deformation of the limb, it cannot be used, because to apply it you will have to straighten the arm and bend it at the elbow joint. This cannot be done when providing assistance; you must try to fix the limb in the position as it is, using the available means.
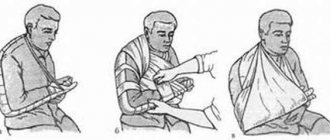
Overlay Rules
All you need to prepare is: a bandage at least 20 cm wide, scissors, a pin or adhesive tape, a small roller made of soft fabric or cotton gauze. In order for the bandage to perform its fixation function as much as possible and not cause inconvenience and undesirable effects, the following rules must be observed:
- Make the victim sit facing you, calm him down, and let him relax.
- Before application, a roller is placed in the axillary area of the injured arm, after which the arm is carefully brought to the body.
- Bend the arm at the elbow joint at a right angle, the hand should be relaxed, and the healthy arm is moved to the side.
- Wrap a bandage around the chest 2 times with the hand pressed to it above the level of the elbow. In this case, if the patient’s right arm is fixed, the bandage is placed around the chest from left to right.
- Having made 2 turns on the back, the bandage is led from the front of the chest obliquely upward to the top of the shoulder joint of the affected arm, bends around it and lowers the bandage along the back surface of the shoulder.
- Bending around the elbow area, the bandage is led obliquely upward into the axillary area of the healthy side, from there it is transferred to the back and the previous move is repeated.
- The end of the bandage cannot be tied; it is fixed to the main bandage with a pin or bandage.
When applied to the left hand, the algorithm of actions is the same with the difference that they begin to bandage in a different direction - from right to left.
How to properly apply a Deso bandage
Wearing rules
For recovery after fractures or sprains, Deso fixing bandages or bandage scarves are prescribed. The orthosis is worn until the person recovers and is removed with the doctor’s permission after approximately 2 months. The doctor determines the mode of wearing the bandage. When the position of the shoulder joint must be at a specific angle, an abduction orthosis is prescribed. It is worn only in the presence of an orthopedist and worn until final recovery.
Elastic bandages used for preventive purposes are used for sports training and during physical activity. They cannot be worn all the time, and sleeping in them is prohibited. In combination with medications, fixing bandages help speed up the rehabilitation period after injuries or operations performed. Bandages prevent the occurrence of various pathologies of the shoulder joint.
Possible errors during application
When applying a bandage, you should not make the following mistakes:
- fixing the hand in the wrong position, this can lead to displacement of fragments and increased pain;
- bandage too tightly, you can squeeze the blood vessels, causing swelling of the hand;
- bandage is not tight enough, leaving the possibility of hand movements when transporting the patient;
- use strips of fabric, sheets, scarves and other materials instead of bandages; they will not provide normal fixation.
Ready-made Deso dressings - indications and application rules
Today, industrially produced ready-made Deso bandages - bandages of various models - are very popular. They are easy to use, provide quick, reliable and adjustable fixation using hooks, Velcro, and locks.
At their core, these are fixing bandages for the shoulder and forearm; they can be purchased at pharmacies or medical equipment and orthopedics stores, as well as in online stores. The price varies from 800 to 4000 rubles, depending on the type of model, materials, and rigidity of fixation. All types of such fixing bandages are selected according to size; in most cases they are marked by clothing size - S, L, M, XL and so on, or their corresponding numbers 1, 2, 3, 4.
Contraindications for use
The use of the Deso bandage on the shoulder joint generally has no contraindications. However, in some cases the use of this tool must be abandoned. Relative contraindications are:
- malignant tumors that are located near the damaged area;
- shrapnel wounds;
- skin ulcers, wounds, dermatitis, boils and pustular formations, dermatitis of various origins;
- allergy to the materials used to apply the bandage.
Note! In such cases, the patient should not independently decide to use this means of fixation. It is necessary to consult a doctor and obtain consent.
Care of the bandage
If immobilization is imposed temporarily only to transport the victim to a medical facility, no care is required. You just need to make sure that the bandage does not move and the fixation does not weaken.
When wearing a bandage for a long time, you need to keep it clean so that the limb does not become infected with pathogenic microbes. If it gets dirty or wet, you need to reapply it, but at the same time make sure that during the process of removing and re-bandaging the hand remains in the same position.
Terms of use
Terms of use may vary widely. At the prehospital stage, the time of fixation of the limb using this method directly depends on the timing of delivery of the victim to the hospital.
When using the Deso bandage to fix the shoulder after a dislocation, the period of wearing it can range from 1 to 3-4 weeks.
At the same time, young patients are subject to longer immobilization than patients older than 30-40 years. This is due to the high physical activity of young people, which leads to repeated dislocations.
The wearing time for fractures of the shoulder or collarbone is approximately the same. It is worth noting that in such cases, fixation methods using a conventional bandage are used extremely rarely, only in situations where the application of a plaster cast or a full-fledged splint is impossible for some reason.
After removing the bandage, exercise therapy and proper nutrition are important during the rehabilitation period.
Alternative bandages for fixing the shoulder joint
Other types of bandages are applied to the shoulder joint area:
- plaster version of the Deso bandage - fixed only in a hospital setting for the purpose of rigid and long-term immobilization for fractures;
- Velpeau bandage is an alternative to the classic Deso bandage with the difference that the arm is bent at the elbow joint at an acute angle, the hand of the injured arm is fixed at the level of the shoulder girdle of the healthy side, it swells less, the indications for application are the same;
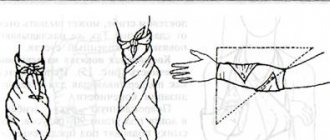
- figure-of-eight bandage and Delbe rings - applied to both shoulder joints, ensuring shoulder abduction in case of a clavicle fracture;
- scarf bandage - used only for first aid, suspends the arm from the neck, excluding movements in the shoulder and elbow joints.
- spica - for bandaging the shoulder and joint in the presence of open injuries, fixing the dressing material on the wound.
During treatment for injuries and diseases, the optimal dressing option is determined by the doctor in each specific case. And for providing first aid for injuries, the Deso bandage is the best option.
Alternative options for the Deso bandage
Shoulder bandage
If a more flexible method of fixation is required, the doctor may prescribe wearing a scarf bandage. It allows, as soon as the opportunity arises, to begin to develop the joint, thereby ensuring normal blood circulation in the area of injury.
Classic shoulder bandage Kerchief is a type of bandage in which the bandages cover the forearm and are attached to the back. In this case, the weight of the bent arm is evenly distributed on the healthy shoulder and the joint does not experience stress. At the same time, mobility is preserved, so a scarf bandage is used for minor injuries, as well as arthrosis and arthritis.
Modern ready-made models are made of durable, wear-resistant, washable material. The position of the limb is regulated by a strap on the shoulder girdle.