The hip joint (HJ) is the largest joint in the musculoskeletal system. It bears the main force load when a person makes physical efforts, moves or lifts weights. When problems associated with the hip joint arise, a person’s quality of life greatly deteriorates, unpleasant pain appears, and in some cases this can cause loss of ability to work. If you seek medical help late and do not start therapeutic actions in a timely manner, the condition may worsen. In this case, the acute hip disease transforms into a chronic pathology. This is fraught with partial or complete loss of motor activity in the damaged anatomical organ.
How to test pain in the hip joint?
The hip joint is called a multiaxial formation, which includes the head of the femoral bone tissue and the acetabulum, which allows the joint to perform the following movements:
- flexion and extension due to the frontal axial position;
- The sagittal axis allows the joint to be moved to the side and returned to its original position;
- implementation of pronation and supination of the hip joint - tilt and rotate outward. A vertical axis allows you to perform these actions.
The spherical surface, similar in anatomical structure to the hinge mechanism, allows you to perform circular movements of the hip.
The main difficulty of clinical diseases of the hip joint is the similarity in symptomatic painful manifestations with other pathologies affecting vital organs. These pathologies manifest themselves as painful manifestations in the lower extremities, lower back or sacroiliac joint tissue.
There are some simple tests that can help identify hip joint pathologies:
- Lie on your back and bend your leg at the knee joint. If, during the process of aggravating compressive pressure on the articular tissue of the knee in the inner part of the thigh, acute pain appears in the groin area, it means that there have been disturbances in the functionality of the hip joint. As the movement increases with the help of internal rotation of the femoral surface, the painful manifestations increase, which ultimately leads to pinching of the tissues in the hip joint in the front.
- Place the back of your hand on the groin area and press firmly. If a clinical disease exists in the joint tissue, acute pain can be felt.
- We find a trochanter in the hip joint and put pressure on it; if such actions are accompanied by painful manifestations, this may indicate the development of trochanteritis.
If you seek specialized help in a timely manner, it is possible to identify hip disease, and this will also allow you to correctly diagnose the pathology and prescribe the correct therapy.
Palpable anatomical landmarks[edit | edit code]
Front surface
- Rectus femoris muscle
- Vastus medialis muscle
- Vastus lateralis muscle
- Superior anterior iliac spine
Medial surface
- Adductor longus muscle
- Thin muscle
- Adductor magnus muscle
Lateral surface
- Iliac crest
Rear surface
- Superior posterior iliac spine
- Ischial tuberosity
- Gluteus maximus muscle
- Biceps femoris
- Semitendinosus muscle
- Semimembranosus muscle
Main causes, symptoms and diagnosis of hip joint diseases
Pathological conditions in the hip most often develop against the background of:
- mechanical damage to joint elements;
- a tendency to diseases of the articular tissue of the hip area at the genetic level;
- functional impairment due to infection;
- systemic diseases in connective tissue;
- damage to the integrity of the joint due to degenerative-dystrophic transformations.
Any disease of the hip joint is characterized by the appearance of common symptoms:
- pain on the inner or outer thigh surface and in the groin area is of an acute, aching or pulling nature;
- motor activity is impaired, movements become limited;
- the skin becomes inflamed, the local temperature rises to subfebrile levels.
To correctly determine hip disease, a high-quality biochemical study is required. In addition, to accurately establish the diagnosis, instrumental diagnostic methods are shown:
- CT and MRI;
- Radiography;
- Ultrasound;
- Scintigraphy.
Let's consider the most common clinical diseases of the hip joint.
Hip dysplasia
This clinical disease is a congenital disorder or inferiority of the joint tissue, which increases the risk of subluxation or dislocation of the femoral head. The maximum number of cases of inadequate development of hip joints is observed in those areas where socio-economic policy is stable.
In the Scandinavian countries, the congenital anomaly is 4%, in Germany – 2%, and in the USA – 1-1.5%.
In the Russian Federation and post-Soviet countries, congenital dysplasia is diagnosed in 50-250 newborns out of 1000 (approximately 5%). According to medical experts, this is due to the unfavorable environmental situation in the states that were formerly part of the Soviet Union.
For the most part, the congenital disease is detected in female infants (in 80% of cases), as well as in families where one or both parents suffer from “congenital dysplasia.”
This congenital orthopedic anomaly can develop due to:
- breech presentation of the unborn baby;
- medical correction of pregnancy, which is complicated by toxicosis;
- large fruit.
A baby can develop dysplasia if he is swaddled too tightly to straighten his legs.
Since 1975, the Japanese have refused to tightly swaddle newborns. This has reduced the number of hip dislocations in infants.
Dysplasia in infants is manifested by the following clinical signs:
- asymmetrical skin folds on the legs;
- pronounced shortening of the thigh;
- restrictions in abduction and adduction of the hip joint.
A characteristic sign due to which one can suspect the presence of congenital dysplasia in a newborn is the Marx-Ortolani symptom. If you abduct the hip joint towards the surface where your baby is lying, you may hear a typical clicking sound in the joint area. This indicates that the femoral head is slipping into the acetabulum area.
The only effective therapy is to use a corrective orthopedic orthosis, thanks to which the baby’s legs can remain in a bent and abducted position at the required angle for a long time. Over time, the newborn is recommended to undergo massage, perform therapeutic exercises with constant supervision by an orthopedist. If treatment is started on time, the child can most often be cured.
Arthritis of the hip joint
Arthritis (coxitis) is a disease characterized by the development of an inflammatory process in the tissues of the hip joint. The disease occurs in acute (primary manifestations), protracted (2-12 months) or chronic form, which lasts more than a year.
Arthritic damage to the tissue system in the hip joint is divided into groups. It happens:
- infectious (septic coxitis) – inflammation that forms against the background of damage to the synovial fluid by an agent of a fungal, parasitic, infectious-allergic or viral nature;
- reactive arthritis - an immune-inflammatory pathology that manifests itself in the process or as a complication of infection of the joint tissue;
- rheumatoid arthritis is an autoimmune disease caused by the formation and spread of granulation tissue in the cavity of the synovial capsule. Because of this, articular cartilage and subchondral bone are destroyed;
- psoriatic arthritis is a rare autoimmune disease of the hip joint, manifested as a result of damage to joint tissue by psoriasis.
Symptoms, signs and treatment of hip coxitis
The causes, symptoms and therapeutic measures for arthritis of the hip joint depend on the nature of the disease.
The development of septic (infectious) arthritis is observed as a complication against the background of severe infection, which penetrates into the joint tissues through the bloodstream. This form of pathology is accompanied by joint pain, limitation of motor activity in the joint, redness and swelling in the problem area, hyperthermia within 39-40 degrees.
For therapeutic purposes, for infectious coxitis, anti-inflammatory drugs are prescribed for intramuscular, intravenous and intra-articular administration, as well as antiseptic and antipyretic drugs. In some cases, surgical treatment of the hip joints is required, which can be performed in Moscow in specialized centers. Failure to contact specialists in a timely manner is fraught with negative consequences; sometimes this disease causes the death of the patient.
The cause of reactive arthritis is an intestinal or urogenital infection. Pathology can also be caused by ureaplasma, streptococci and other microorganisms. This form of coxitis is characterized by the appearance of:
- pain in the hip joint;
- increased temperature;
- hyperemia and swelling of soft tissue in the damaged area;
- pain while walking or other activities.
Which medications will be prescribed for therapeutic purposes for reactive coxitis depends on the type of pathogen. The disease is easily treatable, the patient fully recovers after six months of drug therapy. In this case, the joint tissue is not destroyed.
The exact cause of the development of rheumatoid arthritis has not yet been determined. According to doctors, this is due to immunogenetic disorders in the body. This type of disease is accompanied by stiffness and pain in the joint in the morning, hyperthermia to low-grade levels (37-38 degrees). For rheumatoid arthritis, pharmacological agents of the antirheumatic, anti-inflammatory and hormonal group are indicated in the form of a course of treatment. It is not possible to completely cure coxitis of the rheumatoid form, but regular use of medications helps relieve the main pain syndromes of the pathology.
The psoriatic form of coxitis is a rather rare disease; it develops against the background of a skin pathology – psoriasis. With this disease, soft tissues become covered with dry red plaques, swelling forms, the temperature rises, and aches in the joints. Non-steroidal anti-inflammatory drugs are prescribed for therapeutic purposes. The outcome of the disease is determined by the severity of the condition.
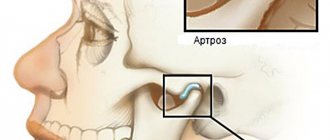
Arthrosis (coxarthrosis)
Pain in the hip joint is often a sign of arthrosis of the hip joint. This is a chronic inflammatory disease, against the background of which dystrophic destruction is observed in the articular tissue of the hip joint.
Due to a lack of lubricating fluid, friction between the bones increases. This leads to the formation of growths on the head of the joint, which makes the functional activity of the joint tissue difficult.
If coxarthrosis of the hip joint is not treated in time, the patient will certainly lose the ability to move.
The essence of diagnostic actions
As with any sprain, when the hip is injured, the degree of injury can vary from mild to severe (where part of the bone is torn off). Clearly determining the level of injury is the first task of diagnosing the hip. Why will the traumatologist perform:
- objective examination with palpation, percussion and functional tests;
- interview for conditions in which signs of strain appeared;
- arthroscopy.
X-rays may be required to monitor the integrity of bone structures. If there is reason to suspect inflammation of the ligaments, the doctor will recommend an ultrasound scan. Among the auxiliary tests, a clinical analysis of the synovial fluid of the hip joint is needed.
Causes, symptoms and therapeutic measures
The main source of dystrophic-degenerative destruction in the joint is the changes in the body that occur upon reaching 65-70 years of age. With age, the necessary elements are synthesized in the joint fluid in a smaller volume, as a result, the joint tissue becomes less elastic and durable.
Drying particles of cartilage settle on the joint capsule, which is why the acetabulum cannot function fully. The inflammatory process and necrosis of rubbing areas lead to the appearance of unpleasant painful manifestations.
In some cases, a significant acceleration of the onset of degenerative processes is possible. This can happen in the background:
- congenital dislocation of the hip joint (dysplasia);
- shock-mechanical damage or fracture of the femoral neck;
- hereditary disorders of the musculoskeletal system in the pelvic region;
- psoriatic infectious or rheumatic inflammation;
- sedentary lifestyle or increased physical activity on the pelvic elements;
- hormonal changes in the body.
The manifestation of clinical signs of pathology is due to the severity of the inflammatory process:
- Arthrosis of the first stage is accompanied by painful discomfort that occurs against the background of physical overload or prolonged movement. A little rest helps relieve pain. Laboratory diagnostics can determine the presence of a slight narrowing of the gap between the joints and fleecy growths along the contour of the acetabulum.
- After arthrosis develops to stage 2, pain symptoms increase, and they are disturbing even when stationary. Motor activity decreases, changes in gait occur, and lameness appears. The main symptom of this form of the disease is the inability to completely abduct the hip to the side, and the patient experiences acute piercing pain at the time of movement. During the X-ray examination, it is possible to examine bone growths on the outer and inner sides of the acetabular notch.
- The most difficult and difficult to correct disease is stage 3 coxarthrosis. With this form of arthrosis of the hip joint, the patient is bothered by constant pain. There is complete limitation of motor activity in combination with a decrease in leg length. On an x-ray, you can see that the surface of the cartilage is completely destroyed, and large osteophytes (bone growths) are formed in its place. Due to this condition, a person may find himself completely immobilized.
According to clinicians, the development of such problems with the hip joint in men is much less common compared to women. The reason for this is the physiological characteristics of the female body.
The goal of therapy for coxarthrosis of the hip joint stages 1 and 2:
- relieve painful manifestations with the help of drugs that have anti-inflammatory, analgesic and analgesic effects - Ibuprofen, Voltaren in gel form, Diclofenac, Ketanol, etc.;
- activate the supply of nutrients to cartilage tissue and start blood circulation with the help of Teraflex, Hondrex, Mucosat, etc.
In some cases, injections into the joint are indicated. For this purpose, they use Osteonil, Fermatron, etc. Also, for arthrosis of the hip joint of stages 1 and 2, physiotherapeutic procedures are prescribed, namely magnetic therapy, paraffin, high-frequency electrophoresis, physical therapy and massage.
If the patient is diagnosed with stage 3 coxarthrosis of the hip joint, surgical intervention – endoprosthetics – is indicated.
Trochanteritis: signs, symptoms and treatment
In this disease, inflammation directly affects the hip part of the skeleton, the greater trochanter of the hip joint (trochanter). This pathology is otherwise called trochanteric bursitis. Painful symptoms with trochanteric bursitis are often similar to signs of hip coxarthrosis. With trochanteritis, the inflammatory process covers the tendons and muscle ligaments located on the surface of the greater trochanter of the femur.
Most often, only one hip trochanter is affected. Moreover, trochanteritis, in comparison with arthrosis of the hip joint, is not accompanied by restrictions in motor activity.
Depending on the location of the inflammatory process, trochanteritis can be:
- aseptic form - inflammation covers the synovial membrane, but pathogens are not involved in the process;
- septic flow - an infectious, bacterial, viral or fungal pathogen spreads throughout the entire pelvic area. The purulent-inflammatory process also affects other surfaces in the vital organs;
- The tuberculosis form is a fairly rare disease, mostly diagnosed in childhood. A distinctive feature is the spread of inflammation both to the greater trochanter and to the tissue adjacent to the bones of the thigh.
Possible factors in the formation of inflammation:
- excess body weight;
- the presence of anatomical disorders in the pelvis and legs;
- hypothermia;
- problems with the endocrine system;
- excessive physical activity.
Most often, trochanteritis is diagnosed in women 25-30 years of age or during menopause due to hormonal imbalances.
Regardless of the age category and gender of the patient, pain symptoms characteristic of trochanteritis can appear against the background of problems with calcium metabolism and after severe damage to bones and joints by osteoporosis.
The doctor selects the treatment, taking into account the origin of the inflammatory process occurring in the greater trochanter. If the cause of the development of the pathology lies in infection of the body, antibiotics are indicated. The aseptic form of the disease involves treatment with non-steroidal anti-inflammatory drugs. If tuberculous trochanteritis is detected, the doctor prescribes anti-tuberculosis medications.
Thanks to intensive treatment, literally after 2 weeks a person can be completely cured. The main condition is to contact a specialist in time.
Treatment of the hip joint
Treatment of hip joint diseases is prescribed only after a comprehensive examination, taking into account the results obtained. For hip pathologies, not only medications are indicated, but also folk remedies (if there are no medical contraindications). During recovery, it is recommended to attend physiotherapeutic procedures. In an emergency, the patient may undergo surgery.
Medications
The selection of medications is carried out by a traumatologist or orthopedist, taking into account the diagnosed disease, the patient’s condition and the individual characteristics of his body. The main thing is to follow the prescribed dosage, since medications can provoke the development of negative reactions.
For problems with the hip joint, depending on the symptoms, treatment with medications from the following pharmacological groups is indicated:
- Non-steroidal anti-inflammatory drugs (Nalgesin, Diclak) to reduce painful manifestations and the inflammatory process. It is recommended to take 2-4 tablets of medication for 2 weeks.
- Chondroprotectors (Chondroxide, Structum) to activate regenerative processes in cartilage tissue. The maximum dose for an adult is 0.5 g orally twice a day. The duration of course therapy is six months.
- Angioprotectors (Pentoxifylline, Stugeron) to improve blood circulation in the hip region. The recommended dosage for adults is 0.2 g three times a day after meals. The duration of the course of treatment for the hip joint is from 1 to 3 months.
- Steroid drugs (Diprospan, Dexamethasone) for intramuscular administration. For an adult patient, the drug is administered once a week at a dosage of 1-2 ml.
- Analgesics (Lidocaine, Novocaine) for subcutaneous or intramuscular administration. For adults, the medicine is administered in a dosage of 5-20 mg.
- Muscle relaxants (Mydocalm, Baklosan) to relieve muscle spasms, reduce pressure exerted on the vessels of the circulatory system. Medicines should be taken 2-3 times a day, 50-150 mg.
- Vasodilator drugs (Trental, Actovegin) to dilate blood vessels, activate trophism and blood circulation in the hip joint. The recommended dosage for adult patients is 100-200 mg up to 2-3 times a day.
If the patient is experiencing severe pain, intra-articular injections are indicated to administer medications that can replace synovial fluid.
Alternative medicine
Complex therapy for hip pathologies involves the use of folk remedies. The main thing is that there are no serious medical contraindications. Before resorting to such methods, you should consult a doctor.
In combination with medications, you can use the following folk remedies:
- Ointment. To prepare, you need to mix an equal volume of liquid honey with glyceride, iodine and 96% alcohol. Place the resulting composition in a dark place to infuse for 12 hours. Apply the prepared product to the affected area and leave until the product is completely absorbed. Upon completion of the procedure, we take a 2-hour break.
- Walnut tincture. You need to pour a glass of partitions into a jar, pour 0.5 liters of vodka into it, seal it tightly and put it in a dark place for 21 days. Strain the finished product and use 1 teaspoon twice a day.
- Herbal collection. For it you need to take 2 tablespoons of the rhizomes of such plants - burdock, willow, parsley, as well as birch leaves and linden blossom. Pour boiling water (0.5 l) over the vegetable mixture, place it on the stove, and simmer over low heat for 10 minutes. Then cool and strain. We take the finished product orally three times a day, 125 ml.
Therapeutic prevention of the development of hip pathologies consists of compliance with sanitary and hygienic requirements, dietary nutritional standards in combination with mineral and vitamin complexes and moderate physical activity.
Price
Name of service
Price
Acceleration of engraftment of hip joint endoprosthesis
from 800 rub.
Make an appointment
Treatment of aseptic necrosis of the femoral head unilateral/bilateral
from 800 rub.
Make an appointment
Treatment of pseudarthrosis in the hip area
from 800 rub.
Make an appointment
Treatment of arthrosis of the hip joint unilateral/bilateral
from 800 rub.
Make an appointment