The optimal treatment option for an individual patient with an Achilles tendon rupture (ATR) is still unknown. The incidence of Achilles tendon injuries is increasing and currently ranges from 6 to 55/100,000 inhabitants. The typical patient is a physically active man in his forties, and since rehabilitation is long and labor-intensive, a thorough knowledge of how to optimize treatment for each patient is necessary.
Stages of rehabilitation
Rehabilitation after ASD can be divided into four stages:
- Controlled mobilization phase (0-8 weeks).
- Early mobilization phase (6-11 weeks).
- Late mobilization phase (10-15 weeks).
- Return to sports (3-12 months).
It is suggested that the decision when a patient can move from one phase to another should be made based on their recovery and the time that has passed since the injury. Pain following ASD is generally not a problem, but the dosage of activity must be controlled to avoid re-injury. Swelling and/or pain in the lower leg is often a sign of too much activity and/or too little recovery.
What should you know about secure fixation?
The application of a bandage plays an important role in recovery after an ankle sprain, and the type of brace directly depends on the individual characteristics of a particular situation. It may be medicinal. This variety is impregnated with a composition that accelerates tissue regeneration several times.
The immobilizing type is used for minor bruises or dislocations. It can effectively limit mobility and reduce pain. If the case was “severe”, then a rigid bandage is used for fixation, which is made of a durable frame and fasteners (straps, ties)
Controlled mobilization phase
During this phase, the injured foot is held in plantar flexion. In addition, a plaster splint or orthosis should be used for 6-8 weeks after injury. According to many modern rehabilitation protocols, controlled exercises focused on plantar flexion of the foot are introduced into the treatment program two weeks (when using orthoses) after injury. Foot dorsiflexion (both active and passive) should be limited during this phase to prevent lengthening and damage to the tendon.
Methods we use
Postoperative rehabilitation and recovery from ankle and lower leg injuries at the SPORTDOC studio includes the following elements:
- Gentle manual techniques aimed at restoring congruence (correct position) and mobility.
- Active rehabilitation techniques aimed at improving stability in all planes.
- If necessary, as an addition to the rehabilitation program, rigid sports taping, kinesio taping, dynamic taping is carried out, and various physiotherapeutic procedures are prescribed.
Early mobilization phase
Walking without an orthosis usually begins in this phase. It is extremely important to recognize both the importance of putting sufficient stress on the tendon and the fact that the risk of re-rupture is greatest at this stage. Stretching the tendon at this stage is not recommended to prevent it from lengthening. However, you can begin to perform active (without weight bearing) dorsiflexion of the foot. Below is a general rehabilitation protocol for this phase.
Friends, on April 24-25 in St. Petersburg, within the framework of the RehabTeam project, Georgy Temichev’s seminar “Ankle and foot (Block 3)” will take place. Find out more...
Early mobilization phase (sessions with a physical therapist 3 times a week, homework)
Exercise program
- Exercise on an exercise bike.
- Exercises to restore the range of motion of the ankle joint.
- Strengthening the calf muscles using an elastic band.
- Heel raises with a load of 25-50% of body weight.
- Lifting on toes (first on two legs, then on one).
- Walking training.
- Balance exercises.
- Leg press.
- Flexion/extension of the legs.
- Exercises for the foot.
If the patient meets the criteria of 5 calf raises on one leg at 90% of the height, then you can begin
- Bilateral jumping in place.
- Jog carefully in place.
In addition, during this phase it is useful to use compression stockings to prevent swelling of the lower leg.
The benefits of massage and physiotherapy
They help reduce the swelling that often occurs in such a situation. These methods are used in our medical center when the acute period ends, and it is not possible to restore the ankle ligaments after a sprain at home. Physical therapy is often given on days 3 or 7. It consists of:
- Diadynamic currents. The use of high-frequency electrical discharges (small) stimulates blood flow and accelerates regeneration processes.
- Ultrasound designed to improve lymphatic exchange during rehabilitation after ankle ligament rupture.
- Paraffin therapy, which is intended to normalize metabolic processes, eliminate residual pain, and prevent inflammation.
- Magnetotherapy. It effectively relieves swelling.
Doctors from Stoparthrosis claim that massage is a must when restoring the ankle joint after an injury. Such “operations” are carried out in equipped rooms. Only doctors with special education, license and the necessary qualifications are allowed to carry out therapy. Inexperienced employees do not perform complex procedures. The minimum course lasts from 10 to 12 days.
Calf muscle recovery
Inspection and palpation of the Achilles tendon
Short-term and long-term recovery deficit
One of the important goals that must be achieved in the early stages of rehabilitation is to perform heel raises (toe raises) while standing on the affected leg. The first step in early rehabilitation may be to perform at least 20 standardized calf raises at 50% body weight.
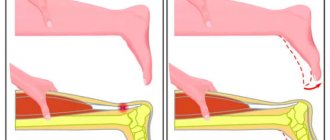
Elongation of the tendon after it ruptures affects the height of the heel rise when performing single-leg calf raises. It is noteworthy that in most patients the performance of the calf muscle is not completely restored. For example, there is evidence that recovery of the calf muscle takes a long time, and an increase in the height of the heel lift of the injured limb can take 7 years after the injury.
Influence of gender
There is some evidence that women and men respond differently when treated with the same methods. Differences are observed in symptoms and heel rise. Further research is needed to conclude whether men and women should be treated in the same ways and whether the hypothesized differences persist over time.
Effect of tendon lengthening
Regardless of treatment with or without surgery, the Achilles tendon lengthens during the healing process. Tendon lengthening affects the height of the heel rise during single-leg raises, as well as the activity of the gastrocnemius muscle. Moreover, kinematic variables depend on tendon elongation, while kinetic variables remain constant. Minimizing tendon lengthening during rehabilitation is important for gastrocnemius muscle recovery.
Effect of age
Older age appears to be associated with decreased ability to repair the gastrocnemius muscle, but individual differences are critical. The causes of deficits in gastrocnemius muscle repair in older adults are not fully known, but they may be related to a decrease in the ability of tendons to remodel due to the aging process. However, it should be remembered that if small positive changes occur during long-term follow-up of a patient, this may be important as patients age.
The effect of calf muscle repair on walking, jogging and jumping
Deficits in heel rise following Achilles tendon rupture appear to affect ankle biomechanics during walking, jogging, and jumping. The impact is greatest during jumping tasks. Early increases in heel lift are expected to be important in restoring ankle biomechanics during challenging exercise.
Predictors of function and symptoms
Early recovery of gastrocnemius muscle endurance and function, together with younger age, are strong predictors of good gastrocnemius muscle recovery, while a high body mass index is predictive of more symptoms and slower recovery from Achilles tendon rupture.
Returning to sports after an Achilles tendon rupture
There is a need for individualized criteria for safe return to sport after ASD, and an understanding that other joints (other than the ankle) may be subject to increased stress to compensate for the decreased load on the injured tendon. The impact of chronic deficits on long-term gastrocnemius muscle recovery requires further study.
To summarize, there is an urgent need for continued research in this area to be able to optimize and individualize the rehabilitation of such patients.
Prevention and treatment of diseases
During active sports, the risk of injury to the lower extremities is quite high, and approximately 25% of all sports injuries occur in the foot and ankle.
In 45% of cases, these are simple sprains of the lateral ligaments, but the presence of the word “simple” in the diagnosis does not mean that full treatment can be neglected. Statistics show that a common sprain without proper therapy in 40% of cases leads to chronic pathology of the ankle joint, which often prohibits further sports activities. What to do? For successful recovery from an ankle injury, you can contact our sports rehabilitation studio SPORTDOC in the center of Moscow. We provide post-operative rehabilitation, conservative (non-surgical) treatment of certain diseases and prevention of foot and ankle injuries. We can offer our clients the following programs:
1. Postoperative ankle rehabilitation:
- Achilles tendon rupture;
- ankle fracture;
- stress fractures, etc.
2. Non-surgical (conservative) treatment of injuries and diseases of the ankle and lower leg:
- torn ankle ligaments;
- subfascial hypertension syndrome;
- tibialis posterior tendonitis;
- Achilles tendonitis, etc.
3. Prevention of diseases and injuries of the ankle:
- anterior tibial-talar impingement syndrome;
- instability of the ankle joint, chronic subluxation;
- plantar fasciitis (spurs);
- hallux valgus;
- longitudinal, transverse flatfoot, etc.
TREATMENT AND RESTORATION OF THE MUSCULOCAL SYSTEM
The Achilles tendon is named after the hero of the ancient Greek epic Achilles, whose mother, the goddess Thetis, wanting to make her son immortal, dipped him, according to one version, into the oven of Hephaestus, according to another - into the waters of the River Styx, while holding him by the heel. According to one version, Paris struck him at this ill-fated heel, which remained the hero’s only vulnerable spot, and according to another, the god Apollo himself, which led to his immediate death.
The Achilles (calcaneal) tendon is the strongest and largest human tendon, capable of withstanding loads of up to 350 kg. Through it, the muscles of the back of the lower leg move the foot, which allows you to stand on your toes and push off the ground when walking or running.
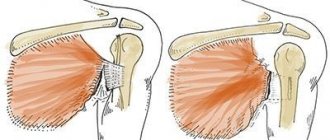
Achilles tendon rupture is one of the most common injuries among the working population. Most often occurs in men 30-40 years old who occasionally engage in sports. The rupture most often occurs at a distance of 4-6 cm from the heel tubercle (in this place the tendon is worst supplied with blood). The right heel tendon is more developed, because in most people, it is the right leg that experiences greater load and is the leading one, so the Achilles tendon of the left leg is more often damaged.
Symptoms of Achilles tendon rupture:
- sudden pain, similar to being hit with a stick on the shin and ankle;
- a crunching sound may be heard accompanying the rupture;
- it is impossible to stretch out the foot or stand on tiptoes;
- there is pain when walking;
- the foot and ankle swell.
If the above symptoms occur, do not massage the calf muscles and tendons. Apply something cold to the tendon and see a doctor.
Diagnosis of Achilles tendon rupture:
- examination by a specialist, conducting a series of diagnostic tests to confirm an Achilles tendon rupture;
- radiography;
- MRI examination;
- Ultrasound.
Despite the apparent simplicity of the clinical picture, Achilles tendon ruptures are not diagnosed in a timely manner in 25% of victims. Therefore, the doctors at our Dr. Grigorenko Clinic pay especially close attention to all patients with complaints of weakness of the plantar impulse and gait disturbance, especially if the injury occurred shortly before treatment.
Mechanisms of Achilles tendon injury.
1. Closed injury:
a. direct: a blow with a blunt object to the strained Achilles tendon leads to a sudden sharp contraction of the calf muscle and rupture of the tendon (more often this mechanism occurs when playing sports);
b. indirect: as a result of a sharp contraction of the lower leg muscles when the leg is extended (when trying to jump in basketball or volleyball); with unexpected sharp dorsiflexion of the foot (when slipping down a step of the stairs); when falling from a height onto a leg with an outstretched toe (at the moment of jumping or landing in volleyball players, gymnasts, ballet dancers).
2. Open injury:
as a result of a cut with a sharp object on the lower part of the lower leg.
3. Achilles tendon rupture can occur due to chronic disease from overuse.
Treatment for Achilles tendon rupture:
Conservative and surgical methods can be used to treat heel tendon ruptures.
Conservative method.
Conservative treatment for rupture is recommended:
- if the injury is fresh and the ends of the tendons can be compared;
- if the patient does not play sports;
- if the patient’s functional demands are reduced due to age, low physical activity or other reasons.
Conservative treatment is not much inferior in its results to surgical treatment, and most importantly, it is characterized by the absence of the risk of infectious complications. The disadvantages of conservative treatment are the longer rehabilitation period compared to surgical treatment. This treatment includes:
1. Immobilization of the leg with an extended toe for 1.5-2 months. This is necessary to bring the ends of the tendon closer to each other and ensure their fusion.
2. Development of the joint, it begins even during immobilization of the limb, and this approach allows improving treatment results. To restore the patient, therapeutic exercises and physiotherapy are recommended.
3. A course of osteopathy and manual therapy - helps accelerate tissue regeneration, gently corrects dysfunctions of the body, helps eliminate functional blocks of muscles, ligaments and joints, optimizes the circulation of fluids in tissues, activates internal reserves for natural healing.
4. Physiotherapy - has an effect on deep tissues, improves blood circulation, stimulates metabolism, maintains muscle tone in the damaged area, is aimed at improving muscle tone and elasticity, eliminating muscle spasms and eliminating congestion in the muscles, helping to avoid the appearance of edema.
5. A course of mud therapy - has a local analgesic, anti-inflammatory and absorbable effect on damaged tissue, normalizes metabolism, improves tissue nutrition, causes softening of scars, accelerates the process of tissue fusion, and reduces stiffness in joints.
6. A course of mechanotherapy - helps strengthen the muscular framework of the whole body and maintain the body in good shape, ensures functional restoration of joints, eliminates complications of diseases, develops physical qualities - strength, flexibility, endurance, mobility, develops correct stereotypes of movements and postures.
7. Functional training - helps to work out the movement mechanisms necessary for a person in everyday life, prepare the body for any load, promotes the development of coordination of movements, flexibility, increasing muscle strength and endurance, and strengthening the joint apparatus.
8. Therapeutic physical education – helps restore impaired properties of the musculoskeletal system, teach the correct and safe performance of movements, improve circulatory function, respiratory organs, metabolism, increase endurance, strength and coordination.
9. Acupuncture - helps improve blood circulation and nervous regulation at the site of injury, reduces the risk of loss of motor functions due to injuries.
10. Compliance with the necessary appropriate diet - muscle tissue must regenerate, and for this it is necessary to consume vitamins and minerals during the rehabilitation period and directly during treatment.
Surgical method.
Surgical intervention must be performed in cases where the Achilles tendon rupture was not diagnosed in a timely manner, the rupture occurred against the background of pre-existing connective tissue diseases, or conservative treatment did not produce the expected effect.
After surgical treatment, it is necessary to carry out a series of rehabilitation measures, similar to the methods used in the conservative method of treatment. Independent rehabilitation can be dangerous; transitions from one stage of rehabilitation to another should be carried out only under the strict supervision of a specialist.
Complications after an Achilles tendon rupture:
Complications of conservative treatment are considered to be a higher risk of re-rupture and fusion with elongation, leading to a weak plantar drive. However, timely and competent conservative treatment is rarely accompanied by these types of complications and is comparable in its effectiveness to surgical methods.
Complications of surgical treatment include primarily infectious complications, observed in 5-10% of cases. The less access to soft tissue during surgery, the lower the risk.