According to statistics, 54% of fractures and fracture-dislocations of the ankle joint occur at a young age, when it is important for a person to maintain working capacity. These injuries are classified as severe injuries to the musculoskeletal system. Even with high-quality treatment, they lead to disability in 3-12% of cases. Therefore, restoring the functions of the ankle joint requires a careful approach, individual for each patient.
The situation is similar with injuries to the ligamentous apparatus. The ankle is often injured in athletes and young, active people. In 30-50% of them, late diagnosis or poor-quality treatment leads to chronic instability of the ankle joint. It interferes with leading an active lifestyle, and over time even leads to disability.
Early diagnosis and quality treatment help reduce the risk of disability. Moreover, ligament injuries, sprains and fractures are much easier to treat initially, immediately after the injury. At the same time, the chances of restoring ankle function are much higher. And the treatment and rehabilitation itself is less invasive and takes less time.
Therefore, after an injury, it is better to immediately contact a good clinic, where they use the most effective diagnostic and treatment algorithms.
How to restore ankle function after injury
How doctors will treat depends on the severity of the injury and the nature of the damage to the joint. After all, ligament tears are much easier to treat than, for example, displaced fractures or fracture-dislocations. Specialists decide on treatment tactics only after examining the patient, having a complete understanding of his condition and the severity of the injury.
Several methods are used to restore the functions of the ankle joint:
- Conservative treatment. Effective for minor injuries that are not accompanied by fractures, dislocations and complete rupture of ligaments. The functions of the ankle are restored with the help of rest, fixation with an elastic bandage, painkillers and anti-inflammatory drugs, physiotherapy and exercise therapy.
- Plaster immobilization. Used in the treatment of fractures in which there is no displacement of the bone fragment and instability of the ankle. Plaster is also applied for fresh ruptures and tears of the ligaments (no later than two to three months after the injury). Plaster immobilization is also used after osteosynthesis and skeletal traction as a final treatment method.
- Closed reduction with further plaster immobilization. Used for closed displaced fractures. It is not recommended for use in cases of concomitant ankle subluxations due to the high risk of unsatisfactory treatment outcome.
- Open reduction with fixation with immersion structures. All open and some closed fractures are treated in this way. In some cases, after surgery, the joint is additionally fixed with plaster.
- Skeletal traction and transosseous compression osteosynthesis. Used to treat complex and chronic fractures in the ankle joint. It is carried out using special external fixation devices.
- Surgery. It is performed for chronic ligament injuries, post-traumatic osteoporosis, severe fractures and fracture-dislocations. Allows you to restore ankle function even when it is impossible to do this in other ways.
Development of ligaments and connective tissue
During the rehabilitation process after a serious ankle injury, additional devices can be used. Buy an elastic fitness band, it will help during exercise therapy. Such products differ in the degree of elasticity. Choose the variety with the least resistance. If you cannot afford such a device, or it is not commercially available, a Martens rubber bandage performs the same functions. It is sold at any pharmacy.
Sit on the floor, stretch your legs forward. Wrap the tape around your foot, forming a comfortable loop to prevent your foot from slipping. Now bend your leg at the knee and carefully straighten it, pulling the tape. This exercise strengthens all the muscles of the limb.
Ankle immobilization
For complete ruptures and significant tears of the ligaments, plaster immobilization or external fixation devices are used. However, they are effective only in the early stages, before a person has developed instability of the ankle joint. For old injuries that are more than 2-3 months old, these methods do not give the expected result.
If a person’s ligament rupture is not detected in time or he does not receive quality treatment, he develops ankle instability. In this case, no immobilization will help restore the function of the joint. And in order to return to work, it is necessary to undergo surgery.
Non-surgical treatment of fractures
Conservative treatment is possible only when there is no displacement of bone fragments and the ankle joint remains stable. In this case, the patient is given a plaster cast for 1-2 months or asked to wear a boot for rehabilitation walking.
Despite the availability and low-traumatic nature of plaster immobilization, it has a number of disadvantages:
- limits the mobility of the lower limb and complicates rehabilitation;
- disrupts peripheral circulation;
- causes irreversible changes in the neuromuscular system of the leg and foot.
In order to partially neutralize the harm of long-term immobilization, from the second or third day after applying the cast, a person begins to engage in therapeutic exercises. Exercise therapy helps relieve swelling, improve blood circulation in the ankle area, and strengthen the muscles of the foot, lower leg and thigh. And this speeds up recovery and prevents the development of post-traumatic osteoporosis.
After the cast is removed, rehabilitation continues for several more months. During this period, the patient is prescribed massage, physiotherapy, physical therapy, etc. The main goal of these procedures is to strengthen muscles and ligaments, improve metabolic processes in tissues, normalize blood circulation and restore the functions of the injured joint.
Why is physical therapy needed?
In order for ankle development after a fracture to be successful, a special set of exercises is selected at each stage of treatment and recovery. Each of them has its own specifics, but they have one thing in common: sudden movements of the injured leg cannot be made.
At the first stage of recovery, when the fractured leg requires complete rest, the patient engages in physical activity without the participation of the injured leg.
Such classes are needed at the first stage of recovery for the following purposes:
- Improve blood flow throughout the body to ensure adequate nutrition of organs and tissues;
- Prevent the development of stagnant processes;
- Prepare the ligamentous and muscular apparatus for subsequent exercises.
In the second stage, once the cast is removed, physical activity is necessary to restore muscle strength and reduce atrophy.
At the third stage, a period of active training begins. The ligaments and muscles prepared in the previous stages are involved in intense physical activity. At this stage, exercises on an exercise bike, treadmill, and in the pool are added to the usual exercises.
Let's look at the features of exercises for developing the ankle joint at each stage.
Exercises in the first stage
The first stage of rehabilitation is a difficult and responsible time: the patient must combine careful treatment of the broken leg and minimal stress.
The first exercises, which are started 3-4 days after applying the plaster, are performed lying down. When performed, they activate the muscle tissue located near the fracture.
- Consistently tense the muscles of the buttocks, thighs and calves up to 20 times;
- Move your toes, squeezing and unclenching them for 1-2 minutes.
After 7-14 days (the specific period for when to start more active exercises is prescribed only by the doctor), they move on to more active training. Their task is to step on the leg with a broken tibia, using it as a support when walking.
- Sit on a chair. Try to straighten the knee of the affected leg so that the limb takes a position parallel to the floor. “Return” your foot to the floor. Do 5-6 approaches.
- Without changing your position, pull the knee of your broken leg towards you with your hands. Lower your leg. Do 5-6 approaches.
- Stand with your hand on the back of a chair. Move your injured leg to the side. Place it on the floor. Repeat the movement 10-15 times.
- Move your injured leg back. Put it down. Repeat the movement 10-15 times.
- Smoothly “point” your leg forward. Put it down. Repeat the movement 10-15 times.
- Repeat the previous exercise. But after pointing your leg forward, fix it in this position for at least 3-5 seconds. Place your foot on the floor. Repeat the movement 10-15 times.
During training, listen carefully to how you feel. Fatigue and discomfort in muscle or joint tissue are evidence that exercise should be stopped. If the pain is minor, you can reduce the number of approaches or range of motion. At the beginning of training, it is better to take short breaks after each exercise performed.
Exercises in the second stage
As soon as the patient's plaster is removed, it is necessary to begin working on the injured joint itself. At first they practice every other day. After the muscles get used to the load, they move on to daily training.
The main position at this stage is sitting on a chair. It is important to remember that 2 legs are involved in the exercise: the sick one and the healthy one. All movements are repeated for 2-3 minutes.
- Without lifting your feet from the floor, alternately “roll” from heel to toe. The movements are made first with two legs, and then with each in turn.
- “Rise” on your toes and stay in this position for 2-3 seconds. Lower your entire foot.
- Press your heels together. Lift your socks up while turning them to the sides.
- Press your socks together. Lift your heels up while simultaneously turning them to the sides.
- Focus on your toes, slowly “rotating” your heels from right to left. Then change the direction of rotation.
- Focus on your heels, slowly “rotating” your toes from right to left. Then change the direction of rotation.
- Extend your legs forward. Make rotational movements with your entire foot from right to left. Then change the direction of rotation.
Exercises in the third stage
The goal of the third recovery stage is to restore the functionality of the broken tibia. Therefore, all exercises involve active walking. To “protect” the still weak joint, all loads are performed using an elastic bandage that secures the ankle joint.
- Walking on your heels.
- Walking on toes.
- Walking with rolls from heel to toe.
- Standing on the canvas, use your toes to “gather” it under your feet.
- Roll a plastic bottle with your feet.
At this time, it is important to take daily walks, go up and down stairs, attend massage sessions, physiotherapy, and maintain a proper and balanced diet.
Closed reduction with further plaster immobilization
This is a common treatment method used primarily for ankle fractures. Its essence lies in the manual reposition of bone fragments and subsequent fixation of the ankle with a plaster cast. This method is accessible and low-traumatic, but has its drawbacks.
Long-term plaster immobilization disrupts trophism and impairs blood circulation in the tissues of the limb, causing irreversible changes in the nerves and muscles of the lower leg, foot, and ankle joint. It does not provide sufficiently stable fixation and does not guarantee complete immobility of the fragments. All this can lead to improper bone fusion and the formation of a false joint.
In case of concomitant dislocations and subluxations of the ankle, it is recommended not to use closed reduction. The reason is the high risk of unsatisfactory treatment results.
The most common of them:
- postoperative contractures;
- false joints;
- severe deforming arthrosis.
Therefore, many specialists prefer a different approach to the treatment of displaced fractures. For patients of working age, they recommend open reduction with fixation of bone fragments with metal structures. And for patients in the older age group, reposition under image intensifier control and fixation with Kirschner wires.
Rehabilitation after an ankle fracture
Ankle fractures are most common in athletes, but are just as common in older people.
In the first case, this is easily explained by strong physical exertion, in the second case, by the fact that the bones of older people become more fragile and vulnerable. To restore motor function, not only proper treatment is necessary, but also rehabilitation after an ankle fracture. It allows you not only to quickly return to your previous lifestyle, but also to prevent possible complications.
The rehabilitation period after an ankle fracture includes a set of measures individually selected by the doctor for the complete restoration of all functions. The complex is selected individually, based on the physiological characteristics of the patient and the complexity of the fracture.
Open reduction with internal fixation
The method is used to treat complex fractures when manual reposition of fragments and holding them in the desired position with the help of plaster is impossible. To compare bone fragments and securely fix them, submersible elements and structures are used:
- tie bolts;
- screws;
- bolts with clamp terminals;
- Kirschner wires;
- bolts with flexible rod;
- lavsan ribbons and so on.
Open reduction ensures immediate accurate comparison of fragments and their reliable fixation. After surgery, early weight-bearing ability of the limb is often preserved, which allows it to be loaded soon after surgery. Nevertheless, many experts are confident that none of the methods of open reduction can ensure complete immobility of bone fragments. Therefore, after surgery, patients require additional plaster immobilization.
Operative comparison and fixation of fragments has other disadvantages:
- Injury to soft tissue at the surgical site.
- Risk of developing infectious complications.
- The likelihood of secondary displacement of fragments due to failure of fixators.
- High incidence of pseudarthrosis.
In some cases, closed fractures are best treated by skeletal traction or transosseous osteosynthesis. These methods exclude the intervention of a traumatologist in the natural healing process. Regeneration is accelerated because the doctor does not remove the hematoma and does not damage the muscles, blood vessels, or periosteum. And the opposition of fragments and stretching of soft tissues additionally stimulates regenerative processes.
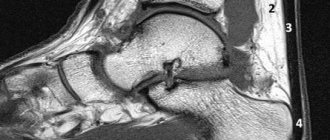
Transosseous osteosynthesis
Today, osteosynthesis is carried out using hinge-distraction devices and skeletal traction devices. The technique allows you to reliably fix bone fragments, which creates ideal conditions for their fusion.
The main advantage of transosseous osteosynthesis is that it does not require open surgery. The disadvantage is that it does not always allow bone fragments to be compared. Therefore, transosseous osteosynthesis can be combined with surgery. First, the fragments are connected surgically, and why the bones are additionally fixed with an external fixation device.
Reconstructive surgeries
Reconstructive surgeries are used to treat chronic ligament tears that are accompanied by ankle instability. The integrity of the ligaments is restored surgically, after which the joint is fixed with an Ilizarov apparatus. If the injury is less than 5 months old, surgery is often performed by arthroscopy. But old ruptures require open reconstruction.
The integrity of the ligaments can be restored:
- local tissues;
- allotissues;
- synthetic endoprostheses.
Plastic surgery with local tissue is associated with additional trauma to the donor site, so it is rarely performed. To restore ligaments, synthetic tissue or allotendon is often used.
Endoprosthetics and arthrodesis
Surgeries on the ankle joint are performed mainly for severe post-traumatic osteoporosis, which is accompanied by severe pain and limited mobility of the ankle.
Young patients often undergo endoprosthesis replacement - replacement of a joint with an artificial endoprosthesis. This operation allows you to completely restore the function of the ankle. When endoprosthesis replacement is not possible (old age, severe concomitant diseases), the patient undergoes arthrodesis - immobilization of the joint. This operation is resorted to as a last resort.
Let's summarize:
- Torn ligaments and ankle fractures often occur at a young age. They are difficult to treat and often lead to disability.
- Fresh injuries are much easier to treat. The sooner a person receives medical help, the higher the chances that joint function will be restored.
- To treat injuries, different methods are used, ranging from conservative treatment to surgical treatment.
- The choice of treatment method depends on many factors. The severity and duration of the injury, ankle instability, the degree of post-traumatic osteoporosis, etc. play a role.
- Surgery is a radical method of treatment. As a rule, surgery is performed when it is impossible to restore the function of the joint in other ways.
Ankle injury: symptoms
If an ankle injury , it is accompanied by sharp and severe pain in the area of the ankle ligaments and the joint itself. In most cases, a fracture prevents a person from putting weight on their leg. It is easy to determine the injury: just try to turn your leg inward. If the pain sharply intensifies, medical intervention is necessary. If an ankle fracture , pain will be felt under the ankle. There may be a visible deformity of the leg. Only an x-ray can determine the presence of a fracture.