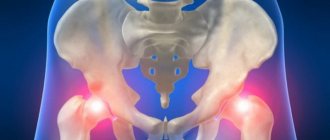
With severe arthrosis of the hip joint, conservative treatment does not give the desired result. The only way to relieve a patient of pain and return him to normal physical activity is hip replacement surgery.
As with any other surgical procedure, complications can develop after hip replacement. Their occurrence is influenced by the patient’s age, the nature of the pathology in the joint, concomitant diseases, and excess weight. Therefore, before the operation begins, all possible reasons are taken into account to minimize the risk of complications in the postoperative period.
Dislocation of the endoprosthesis: causes
According to statistics, endoprosthesis dislocation is more often diagnosed in females than in males. The risk group also includes people with:
- Aged people. This is due to their weak bone structure, which becomes more loose;
- Suffering from overweight and obesity. This is due to the fact that a large body weight will place too much stress on the prosthesis on a daily basis;
- Those who are tall.
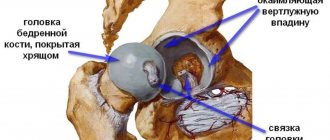
The diagnosis of hip replacement indicates that the implant previously implanted in the hip area has moved beyond the acetabulum.
There are several reasons for this:
- Other surgeries that have been performed in the hip area;
- Violation of the regimen prescribed by the doctor;
- Hip injury;
- Existing pathological defects in the hip area;
- Exercising too intensely or doing too much physical activity;
- Muscle weakness;
- Pushing out the cup itself;
- Diagnosis of dysplasia.
Since the endoprosthesis is an artificially created implant, it is worth considering that the cause of its dislocation can also be:
- Loosening the structure itself;
- Breakage of polymer parts;
- The size is too small.
A simple mistake when installing a prosthesis can cause its subsequent dislocation. Surprisingly, the vast majority of cases (almost 75%) of prosthetic dislocations occur within one year after installation.
Associated symptoms
There are the following accompanying symptoms of hip dislocation, indicating the presence of serious problems:
- arthroplasty led to inflammation of the affected area, weakening the functioning of the artificial joint;
- swelling of the legs, pain in the articular part of the hip;
- discomfort during physical activity, walking;
- the presence of osteoporosis, which reduces the density of bone structures, as a result of which the injured area becomes susceptible to infection;
- the appearance of blood clots in the lower extremities;
- the presence of osteoliosis, which disrupts the bone tissue of the joints;
- allergic reactions. This phenomenon may be associated with intolerance to the metal used in the manufacturing process of the prosthesis;
- spasms of the muscles of the hip region.
Endoprosthesis dislocation: symptoms and signs
Symptoms of hip prosthesis dislocation in most cases appear immediately after its occurrence. The patient begins to notice symptoms such as:
- Severe pain that gets worse when you move your leg or try to stand on it;
- Muscle tension in the thighs;
- Weakness in the leg. Even if the patient can walk, he will feel insecure. The gait will be very shaky and unstable;
- Limitation of limb mobility.
With a dislocated endoprosthesis, the patient can only walk with great difficulty.
Visual symptoms are shortening of the limb in which the prosthesis is placed. If the sprain was preceded by an injury, there will also be swelling, redness, and sometimes bruising.
It is rare that a person does not know about a dislocation for some time, since pain symptoms are completely absent. Unfortunately, this only aggravates the situation, because the earlier treatment is started, the lower the risk of developing serious complications.
Specific symptoms include increased body temperature. This phenomenon occurs when an inflammatory process develops in the body against the background of a dislocation.
Problems of endoprosthetics
joint replacement surgeries are performed . In Russia, the result is several times lower – up to 40–50 thousand manipulations. Although the need for such treatment significantly exceeds this number.
The high demand for surgery to install an implant and the activity of endoprosthetics is explained by the effectiveness of this treatment method. Remaining radical (surgical intervention), in many cases it becomes life-saving when non-surgical treatment is impossible.
But the surgeon’s responsibility is not limited to the invasion itself (the procedure for replacing part or the entire joint). In addition to the operation, monitoring the patient’s condition during the rehabilitation stage and after its completion is extremely important. The need for such control is explained by the aseptic instability of the endoprosthesis or its parts in the short or long term.
Failure of the endoprosthesis after endoprosthetics , as one of the complications of surgical treatment, is the main, but not the only problem:
- with all its achievements, orthopedics and traumatology have not yet found an ideal material for an implant that is guaranteed not to cause any damage to the human body after many years of use;
- even the most reliable materials begin to deteriorate over time - their smallest parts get into the tissue around the implant, causing inflammation, disruption of local blood supply and even cell death;
- against the background of inflammation, the prosthesis itself becomes loose, which accelerates its destruction and leads to infection with all the ensuing consequences, fractures of the hip bone, including one of the largest bones of the skeleton - the femur.
Diagnosis of pathology
Diagnosing a hip dislocation is quite simple. In most cases, the patient suspects prosthesis dislocation immediately after the first symptoms appear. Doctors with such a problem should consult a traumatologist or surgeon. During the visit, the doctor visually assesses the patient's condition and examines symptoms. But to confirm the diagnosis, it will still be necessary to seek the help of instrumental methods, namely:
- X-rays. The photo clearly shows the location of the joint and the fact that it is located outside the acetabulum;
- Computed tomography and magnetic resonance imaging. These are more advanced methods that are used when x-rays do not provide complete information about the cause of the sprain. Using these techniques may be especially important before surgery.
If necessary, additional testing procedures are performed.
Treatment of mobility impairment
Treatment tactics for hip joint dislocation depend on various factors. First aid in this case consists of the use of painkillers and anti-inflammatory drugs. You can try to straighten the joint itself. It is highly advisable that this procedure be performed by a doctor. To suppress pain during joint reduction, the patient is given mild sedatives, or, if necessary, general anesthesia can be used. The reduction method is selected depending on the direction of displacement of the implant head.
Please note! In most cases, simple reduction is effective and the joint falls into place. Then x-rays are performed to ensure the complete success of the procedure and to identify possible hidden causes of implant dislocation.
If the dislocation occurs again, surgery is prescribed, since the problem appears to be systemic in nature. The endoprosthesis is adjusted or replaced with a new one.
Prostheses with a smaller head diameter (22-28 mm) have optimal wear resistance, but they are more susceptible to the risk of dislocation. At the discretion of the doctor, a new implant with a large epiphysis (up to 40 mm) can be installed in accordance with the acetabular part of the joint.
Before reduction using the open method, a comprehensive diagnosis is performed to identify the causes of dislocation and choose the best method of surgery. If, as a result of dislocation of the prosthesis, an extensive hematoma has formed or the femoral or sciatic nerve has been pinched, open reduction can last several hours. During the operation, the damaged intra-articular membrane is removed so that the soft tissue can form a new pseudocapsule, which will give the endoprosthesis greater stability.
Implant dislocation on x-ray
Endoprosthesis dislocation: treatment
The prescribed treatment directly depends on the nature of the dislocation of the prosthesis. The primary case is usually treated conservatively. However, if a patient is repeatedly diagnosed with this problem, it is unlikely that surgery will be avoided.
Conservative treatment
Conservative treatment consists of traditional repositioning of the dislocated hip joint prosthesis. Since this procedure is quite painful, the doctor must use anesthesia or spinal anesthesia.
After the denture has been reduced, the patient should be advised to rest in bed. On average, this takes 8-10 days. The patient then begins to walk independently on crutches. The next stage is walking with a cane and, finally, walking without assistive devices.
Immobilization of the hip joint
To fix the prosthesis, a plaster cast can be placed on the patient immobilized in the correct direction:
- Gypsum bandage. It may cover the entire limb or only part of it;
- Orthosis. One of its varieties is derotational shoes;
- Longett. In this case, it is attached under the knee joint on the back of the leg.
The listed procedures are the basis of conservative treatment. But everything will not work without drugs. They are necessary to speed up the body’s regeneration process, as well as to prevent complications. Therefore, drugs are prescribed in a comprehensive manner: anti-inflammatory drugs, anticoagulants, microcirculation stimulants, vitamin complexes. Antibiotics are added if necessary.
Surgical treatment
Since hip dislocation can occur for various reasons, related to both internal processes occurring in the patient’s body and external factors, the course of the operation is individual in each case. Therefore, the surgeon conducts a thorough diagnosis, on the basis of which the operation will be performed.
In addition to returning the prosthesis to its original position, surgical intervention should be aimed at eliminating the causes of possible relapse. Thus, the surgeon can perform the following procedures:
- Restoring the strength of muscle tone surrounding the prosthesis;
- Enlargement of the prosthesis head;
- Increase in neck length;
- Replacement of prosthetic components;
- Replacement of prosthesis.
The nature of the operation is quite serious, and given that most patients are elderly with an already weakened bone structure, the surgeon must be aware of the responsibility of his work.
FIRST STEPS
The goal of this rehabilitation period is to learn how to get out of bed, stand, sit and walk so that you can do this safely yourself.
At this time, you still feel weak, so in the first days someone must help you, supporting you (you may feel slightly dizzy). Remember, the faster you get up, the faster you will begin to walk. The medical staff can only help you, but nothing more. Progress is entirely up to you. So, you should get out of bed in the direction of the non-operated leg. Sit on the edge of the bed, keeping your operated leg straight and in front. Before standing up, check that the floor is not slippery and that there are no rugs on it! Place both feet on the floor. Using crutches and your non-operated leg, try to stand up. Caring relatives or medical staff should help you in the first days. Using your healthy leg, move your two crutches forward. Then bring the operated leg to the level of the crutches, slightly bending it in all joints. Leaning on the crutches and transferring your body weight to them, move your healthy leg forward. Repeat all movements in the same order.
When walking in the first 10-14 days, you can only touch the floor with your operated leg. Then slightly increase the load on your leg, trying to step on it with a force equal to the weight of your leg. You can walk for as long as your well-being and the condition of your leg allow, without reducing the time of therapeutic exercises. If you don’t do gymnastics enough, incorrectly, or overuse walking, the swelling of your legs will increase by the end of the day. In this case, consult your doctor for clarification. Concomitant diseases can maintain leg swelling.
After you have learned to confidently stand and walk without assistance, physical therapy should be expanded with the following exercises performed in a standing position.
Knee Raise
Slowly bend the operated leg at the hip and knee joints at an angle not exceeding 90 degrees, while raising your foot above the floor to a height of 20-30 cm. Try to hold the raised leg for a few seconds, then also slowly lower your foot to the floor.
Taking the leg to the side
Standing on your healthy leg and holding the headboard securely, slowly move your operated leg to the side. Make sure your hip, knee and foot are facing inward. Maintaining the same position, slowly return your leg to the starting position.
Taking the leg back
Using your healthy leg, slowly move your operated leg back, placing one hand on the back of your lower back and making sure that your lower back does not arch. Slowly return to the starting position.
We recommend doing the exercises listed above up to 10 times a day for several minutes. They will help you significantly speed up the rehabilitation period and quickly start walking without assistance.
Almost every patient needs to walk up stairs. Let's try to give some tips: when moving up, you should start the lift with the non-operated leg. Using crutches, move your non-operated leg to a higher step. Shift your body weight to your non-operated leg on the step above. Then the operated leg moves - lift it and place it on the same step. The crutches move last or simultaneously with the operated leg. When going down stairs, place your crutches and your operated leg on the step below first, then your non-operated leg. Leaning on crutches, bend the non-operated leg at the joints and, maintaining balance, place it next to the operated leg.
If possible, use a handrail instead of one crutch. So, let us repeat once again the general rules for moving up the stairs - the healthy leg is always on the upper step, the sore leg is always below, on the lower step. The crutches remain for support on the same step as the sore leg.
Features of the rehabilitation period
The rehabilitation period for a dislocated hip prosthesis is as important as the treatment itself. If the patient treats it irresponsibly, there is a high risk of developing various complications, as well as the risk of displacement of the prosthesis.
Rehabilitation after hip dislocation replacement includes physical therapy and massage.
If the patient's condition is satisfactory, he can be helped to stand the next day after surgery. Basic rehabilitation measures include:
- Walking training. Spheres will be needed initially. They will help not to put too much pressure on the operated leg;
- Basic motor training, namely: independent sitting position;
- They undergo physiotherapeutic procedures. They are aimed at accelerating regenerative functions;
- Attending physical therapy classes. During these therapeutic physical exercises, all joints are connected so that in the future the limbs can be moved painlessly;
- Performing therapeutic massage. This is necessary in order to relax the thigh muscles.
Let us immediately note that the duration of the rehabilitation stay in each specific case is different. Each subsequent stage of rehabilitation is based on the patient’s well-being. Independent walking without crutches and a cane is possible on average 5-6 months after surgery.
How to avoid dislocations: a list of prevention rules
An artificial analogue of hip joints can serve efficiently for 15-30 years, but only under the condition of conscientious compliance with lifelong requirements. It is necessary to clearly understand that dislocations often occur due to the fault of the patient himself, who violated the principles of proper lifestyle and physical activity. So, to prevent postoperative consequences, including its relapse, it is necessary:
- regularly take control photographs of the operated area (for the first time they are taken after 3 months, then 6 and 12 months after the operation, then once annually);
- do exercise therapy daily - 1-2 times a day;
- avoid jumping, crossing legs, squatting, any sudden body maneuvers, overloading the section, twisting in the pelvic girdle area;
- sit on chairs of normal height with level back support, keep your spine straight while sitting;
- take all precautions to prevent traumatic situations;
- wear comfortable shoes with orthopedic soles, avoid high-heeled shoes and high-platform shoes;
- eat a balanced diet, monitor your weight (if your body weight is higher than normal, consult a nutritionist for help in losing weight);
- do not lift heavy objects and do not allow work associated with heavy physical labor;
- If you experience supporting and motor discomfort, pain, or swelling in the area of the endoprosthesis, immediately consult a doctor;
- if the problem persists, fully recover after the reduction of the head of the joint is performed in a medical facility.
Attention! To prevent dislocations, doctors recommend a special set of exercises aimed at effectively working out and increasing the endurance of the hip and gluteal muscles. It is extremely important to strengthen these muscle groups, because they are the main regulators of movement and stabilizers of the implant joint.
Possible complications
As mentioned above, prosthetic dislocation usually occurs shortly after surgery. This fact is not difficult to discover. The patient begins to experience all the same symptoms as before treatment, namely:
- Sharp pain in the thigh area;
- Limitation of limb mobility;
- Shortening of the diseased limb compared to the healthy limb.
In this case, the patient will undergo surgery to return the prosthesis to its original position. But in addition to this fairly standard phenomenon, various complications can also occur. They can be associated both with the body’s reaction and with mistakes made during the operation.
Possible post-operative consequences include:
- Infectious processes. This may be indicated by symptoms such as swelling or redness of the skin; nerve inflammation. This can be expressed in various manifestations, for example, a feeling of numbness in this area;
- Joint spasm. This means that the joint cannot perform some of its functions;
- Venous and arterial thrombosis.
- To reduce the risk of developing these and other complications, it is important to follow a number of preventive measures and follow all doctor's recommendations.
Since dislocation of the endoprosthesis, although rare, is quite unpleasant, it is important that people who have undergone surgery to put it on follow all the rules to prevent this situation. These measures are as follows:
When to wear a hip brace:
- During rehabilitation in the postoperative period (including after complete endoprosthetics or removal of the femoral head), as well as after hip dislocations and other injuries (operations) of a similar nature.
- Recovery after reductions and procedures aimed at eliminating the consequences (and the treatment itself) of damage to the ligamentous-muscular system.
- Treatment of intertrochanteric repositioning osteotomy.
- Inflammatory processes (for example, ligaments and tendons).
- To reduce pain, including pain due to inflammatory and degenerative processes.
- For the purpose of prevention aimed at preventing injury to the hip joints of the femoral neck: for example, with too intense fitness loads or due to occupational risks. In addition, the use of a bandage may be relevant for elderly patients, especially those suffering from osteoporosis.
- Pediatric medicine: treatment of congenital subluxations and pre-luxations of the hip in newborns, as well as therapeutic and preventive measures to alleviate the condition of infantile hip dysplasia.
- Other indications identified after an individual medical examination.
Thanks to the modern design, there are practically no contraindications for use. The exceptions are acute inflammatory processes (with a medical prohibition), individual intolerance and open wounds, cuts in the area where the product is intended to be worn.
What types of hip bandages are there:
- Special: for example, with fixation on the right or left leg. And also in the form of a thin (or wide) belt with Velcro and with stiffening ribs. In addition, in some cases, the use of derotational orthoses is relevant.
- For men or women, taking into account anatomical features. However, most modifications are universal - they are great for both men and women.
- For babies - special children's hip bandages, which also includes Freika's feather pillow.
With the correct selection of modifications and sizes, joint fixators can provide the proper level of support for tissues and the musculoskeletal corset.
How to choose a hip bandage?
- To purchase a model that really suits you, you need to consider several important factors during the search process:
- The material should be pleasant to the body, but at the same time practical and resistant to wear. For example, many modern models are produced with a combined composition: 40% polyamide, 40% elastane and 20% polypropylene. In this way, it is possible to achieve both excellent comfort properties and optimal moisture and breathability. There are options on the market that have a certain percentage of cotton. However, a hip bandage does not necessarily have to contain natural raw materials, since it rarely comes into direct contact with bare skin. While durable and perfectly shape-holding artificial fabrics are able to cope much better with the tasks of supporting the work area.
- Some series are created using perforated bandage tape, which plays an exclusively positive role (since the desired degree of tightening is achieved with safe micro-massage).
- If the model is equipped with special Velcro fasteners or additional adjustable fasteners, this can be a positive sign for the buyer of maximum ease of use. However, some modifications work excellently even with a minimal design (no secondary fasteners or tension bands), it all depends on the purpose of use and the level of complexity of the pathology of a particular patient.
- The manufacturer plays a significant role. Ideally, this should be a brand that is well aware of all the features and innovations of the medical and orthopedic industry, and also creates its products with the participation of leading experts in this field. Thus, the large Russian brand Kreit (St. Petersburg) has been successfully developing and manufacturing its products only in collaboration with practicing doctors for more than 20 years. That is why hip bandages from this manufacturer can be used with complete confidence not only for preventive, but also for therapeutic purposes.
- Cost is another important aspect that can be problematic for many buyers. Fortunately, most modern budget models of domestic production cope excellently with their role and even outperform many European analogues in efficiency. Therefore, there is no need to overpay for the same quality and performance: the main thing is to buy a bandage in a trusted store that has proven itself well in the market.
How to properly care for the product:
- To preserve the original properties and efficiency of the structure, it is recommended to follow a few simple care rules:
- Hand washing separately from other items is preferable, but washing machine use is allowed (only on delicate cycle). The washing temperature should not exceed 40ºC. Detergents - with a gentle composition.
- Strong friction and squeezing are not allowed, because this can lead to loss of shape. Dry cleaning and ironing are prohibited.
- After washing, rinsing under running water is sufficient to remove any remaining detergent. To dry, place the product on a flat surface, away from heating devices and direct sunlight.
- Store in a well-ventilated place.
Hip bandage: reviews
“I immediately felt relief when moving, the pain did not go away completely, of course, but it doesn’t bother me so much anymore. This has already become a huge achievement for me! The price of the bandage when ordering on the website turned out to be almost one and a half times lower than in the orthosalon, it was nice to save money. I still use it now, because even just walking without a bandage is problematic. Satisfied, everything suits me. I plan to use the same bandage to fix the joint after endoprosthetics.”
Irina, 46 years old
“I fell and received a severe bruise, the doctor said that I urgently needed to buy a bandage for the hip joint so that the recovery would go faster (probably tired of my constant complaints about aching pain, but I really couldn’t really take a step, even with crutches!) .
What can I say: the Crate brace that I eventually bought provided super support for the hip joint, and was not at all expensive. The main plus is that I needed it on the left side, and such a model was found without any problems (which was not possible to achieve from other companies), thank you!”
Olga, 25
“We took a retainer (feather pillow) for the child. Among the advantages, I can highlight the low price (this is important for young parents), as well as the lightness and good ventilation of the material. Very easy to care for - washed in a regular machine, on a delicate cycle. Behind
for the kind of money and for the benefits it brings, I would buy again without hesitation. Performs its function as it should."
Semyon, 35
If you need to buy bandages and orthoses for the hip joint or other medical and orthopedic products, we recommend that you look at the MegaMedShop online catalog. Here you can find the most extensive range at reasonable prices and with delivery throughout Russia. Do you want to pick up your order yourself? No problem: several of our offices are open for pick-up especially for you. All necessary certificates and supporting documents are available. Our experienced managers are always ready to give comprehensive advice on any issue that concerns you: from choosing the right model, size, to choosing the best payment and delivery options.
Prevention
Regular visits to the doctor to monitor the installation of the endoprosthesis;
- Carrying out all necessary procedures: massage, therapeutic exercises;
- Strict control of the amount of physical activity. Heavy loads and excessive physical activity are not allowed;
- Avoid excess weight. This means that the diet should be as healthy and balanced as possible;
- Wearing comfortable shoes, preferably orthopedic;
- Body position control. The more the patient's back is straightened, the less load on the prosthesis.
- The most important thing that a patient should do after surgery is to follow all the recommendations of the attending physician. If the patient is required to wear special equipment or take medications, this is to help you recover as quickly as possible and reduce the risk of spraining the prosthesis. However, if there are symptoms that directly indicate recurrent denture dislocation, do not try to wait it out or self-medicate. The best solution is to seek professional medical help immediately.
SHOWER AND BATHING
For the first six weeks after surgery, it is advisable to avoid bathing and prefer to wash in a warm shower. In this case, it is advisable to have someone nearby until you feel confident. If a bath cannot be avoided, then we advise you to adhere to some simple rules that make taking it as safe as possible. Firstly, avoid hot baths for up to 6 - 8 weeks - this is not at all related to the possible heating of your new joint, as patients mistakenly think. Rather, it is caused by the dangerous effect of hot water on the possibility of blood clots forming in the operated leg. Secondly, when entering the bathroom, always sit on the edge, holding the tub firmly with your hands. The legs are transferred one by one to the bathroom, while the entire load should be transferred to the hands, with which you must hold firmly. After this, you can carefully immerse yourself in the water, while the entire load should be transferred to the slightly bent healthy leg, and it is better to keep the patient straight.
You should also carefully exit the bath, again concentrating all the stress on your arms and healthy leg. The sore leg moves smoothly out of the bath, remaining in a straight position.
It is strictly forbidden to visit a bath or sauna during the first 1.5 - 3 months (due to thromboembolic complications).
We remind you once again that during this period:
- It is advisable to sleep on a high bed.
- After surgery, you should sit in high chairs (like bar stools). A regular chair should be cushioned to increase its height. Low, soft seats should be avoided. It is important to observe all of the above when visiting the toilet,
- It is strictly forbidden to squat, sit cross-legged, or “cross” the operated leg over the other.
- get rid of the habit of picking up fallen objects from the floor - you should do this with the help of any devices that exclude bending and squatting.