Endoprosthesis replacement is the most popular surgical method of the musculoskeletal system. During the operation, the damaged joint is replaced with an alternative option - an endoprosthesis.
For a person to be able to restore full functions and mobility, one operation is not enough. A course of rehabilitation is definitely recommended. In many cases, you have to recover after surgery on your own.
This will cause pain, lameness and low range of flexion. When practicing on your own, you need to take into account that not all movements from exercise therapy are suitable for every person.
You can use a simple simulator, which can be an ordinary ladder. This type of walking does not promote stretching, but it will help strengthen the muscles.
To ensure safe rehabilitation at home, you need to consult a specialist. This could be an orthopedist or a rehabilitation specialist. It is worth noting the main goals of the rehabilitation period:
- Prevention of the development of pneumonia and bedsores that can occur if you do not move after surgery.
- Restoring the tone of the operated limb and muscle system.
- Normalization of joint function.
- Prevention of thrombosis formation.
- Restoring self-care and walking skills.
Starting position: standing, leaning on a table, the back of a chair or on a handrail. Move your leg to the side as far as possible. Repeat 5-6 times. Then perform the exercise with your healthy leg. When performing the exercise, make sure that your back remains straight.
- It is ideal if the load on the leg increases very gradually.
- In a standing position, raise your knee parallel to the ground. Hold your leg in this position for 5 seconds, then lower it. This exercise requires multiple sets.
- Much depends on the patient’s age, his general condition and physical development of muscles. Accordingly, the older the patient, and also the more physically weakened he is, the longer the rehabilitation process will take.
- The next day after endoprosthetics, you can begin to walk slowly, leaning on crutches. Almost all patients are advised to immediately try to walk on the operated leg, the so-called pain tolerance principle. By the fourth day you can already walk 100-150 meters several times a day.
Bending-extension of legs while lying on stomach
When climbing up the stairs, they begin to move from the non-operated limb:
- Slowly straining the thigh muscle, straighten the leg and hold it in this position for five six seconds. Then we lower it just as slowly
- For the first two to three weeks, exercise therapy is performed while lying in bed. But you literally need to get back on your feet on the second day
- The following measures are used to prevent thrombosis:
- No one can avoid pain after surgery. The anesthesia wears off and inevitable pain attacks begin, accompanied by swelling. It is difficult for an already exhausted patient to endure this, and they come to the rescue:
- Thus, just 45 minutes a day dedicated to your health will help you literally get back on your feet after hip replacement surgery. At the same time, you need to be very careful. A fall can be fatal for the patient and lead to further surgery. While compliance with safety rules guarantees the service of the prosthesis for a long 15 years.
Principles of rehabilitation
Rehabilitation after hip replacement is considered successful if the following improvements are observed after completion of the course:
- there is no pain when moving the hip joint;
- the patient returns to normal life and does not need outside help;
- the work of muscles and ligaments is normalized, articular joints move smoothly;
- correct movement patterns and coordination in individual muscle groups are restored;
- weak muscles are strengthened.
Rehabilitation consists of physiotherapy, exercise therapy, and drug treatment. With the right approach, you can achieve the following results:
- blood circulation in the lower extremities improves;
- muscle strength and range of motion in the damaged joint increases;
- pain, swelling, signs of inflammation disappear;
- the statics of the spine is normalized;
- The body's protective functions are strengthened, which reduces the risk of complications.
Methods for effective rehabilitation after hip replacement are selected by the doctor. You should not self-medicate, as this can lead to negative consequences.
Description of the surgical process
Let's consider the classic scheme of the operating process.
- The limb is widely treated with an antiseptic and tourniquet.
- Next, the joint is opened through a certain approach without crossing the muscles and ligaments. Advantages are given to minimally invasive methods of creating access.
- Having carefully spread the soft tissues and secured them with a clamp, the specialist opens the joint capsule and removes it.
- This is followed by resection of the femoral head at the correct angle and, if the procedure is total, the acetabulum is cleared of damaged cartilage.
- A prosthetic cup (made of metal or ceramic) is placed into the pelvic cavity freed from cartilaginous tissue. Its dimensions perfectly match the dimensions of the natural bone notch. A polyethylene gasket is inserted into the installed bowl. In case of partial replacement, the cup is not implanted.
- Afterwards, a properly shaped channel is drilled into the transected femur, where a metal or ceramic leg of the endoprosthesis is placed, at the upper end of which a sphere (artificial head) made of the same material is attached.
- The head of the implant is set into the cup. The implanted hinge system is being tested.
- After making sure that the new joint is working perfectly correctly, the surgeon completes the procedure by washing the surgical field, installing drainage and suturing the wound. At the end, the operated leg is fixed with an elastic bandage in an advantageous position.
Terms of rehabilitation
The average duration of the rehabilitation period is 3 months. If the pain persists, you can continue to walk using a cane. You can start active training after 8-12 months.
But even after complete recovery, you must follow some rules throughout your life:
- do not bend the joint more than 90 degrees;
- regularly perform moderate physical activity;
- do not quit training after full recovery;
- visit a doctor regularly;
- stop smoking and drinking alcohol;
- Healthy food;
- Do not take any medications or herbs without consulting your doctor.
Drug treatment
Medicines are prescribed to relieve pain, signs of inflammation, accelerate regeneration and prevent the development of complications.
Main groups of drugs and their action:
- Broad-spectrum antibiotics prevent the development of secondary bacterial infections after surgery.
- Non-steroidal anti-inflammatory drugs - eliminate pain and manifestations of the inflammatory process.
- Vitamin complexes with calcium, chondroitin, collagen accelerate the regeneration of muscles and bone structures.
- Anticoagulants - prevent the formation of blood clots.
- Cardioprotectors - reduce the risk of developing heart failure.
- Gastroprotectors - protect the walls of the stomach and duodenum from the aggressive effects of other drugs.
- Anticholinesterase drugs - eliminate intestinal atony.
After antibacterial therapy, a course of probiotics and dental antibiotics is prescribed to restore the balance of the intestinal microflora.
Comprehensive physiotherapy
Physiotherapy is an important component of successful rehabilitation after endoprosthetics. The goals are to improve microcirculation, activate metabolic processes, increase muscle tone, and eliminate spasms.
Kinesiotherapy is a type of physical therapy, movement treatment, prescribed at an early stage of rehabilitation. Classes are held on a special simulator for the hip joint. The complex is compiled taking into account the individual characteristics of the body, the presence of certain diseases in the patient.
To achieve results, you need to practice regularly under the strict guidance of an instructor. The patient masters all exercises gradually, the loads increase gradually taking into account the body’s adaptation. During gymnastics you need to breathe correctly, this helps to cope with pain and engage deep muscles.
Contraindications: malignant neoplasms, infectious pathologies, open and closed bleeding. Gymnastics cannot be performed with high blood pressure, tachycardia, diabetes, thrombosis and thrombophlebitis.
Hydrokinesitherapy - therapeutic exercises in the pool. Allows you to avoid excessive loads on the joint capsule and the appearance of unpleasant sensations. Improves the functioning of the entire musculoskeletal system and immune system.
Effective physiotherapy after endoprosthetics:
- Cryotherapy. Forms filled with hydrogel are applied to the prosthetic site. The duration of the procedure is 15 minutes. Helps quickly get rid of pain and swelling.
- Electrical stimulation. Exposure of tissue to current of a certain frequency. Muscles contract, strengthen, and tone increases. The method activates metabolic processes and improves blood circulation in the surgical area.
- Magnetotherapy. The tissue is exposed to a high or low frequency magnetic field. The result is a decrease in pain, a decrease in signs of inflammation, a mild sedative effect, improved vascular elasticity, and accelerated tissue recovery.
- Watsu is a body-oriented technique. Combines body support, muscle traction, mobilization of cartilage tissue, joint healing, massage. Allows you to increase the range of motion of the hip joint to its natural amplitude. After the first session, mobility improves, spasms disappear, and pain decreases. Additionally, the protective and restorative functions of the body are activated, sleep improves, and emotional stress goes away.
- Orthotics. An orthosis is selected for the patient for fixation, correction of functions, and unloading of the limb during recovery after surgery.
- Laser therapy. The light beam improves the body's self-regulation. After the procedure, swelling and pain are reduced, and the immune system is activated.
Therapeutic massage is prescribed after relief of acute pain. Sessions are carried out to improve blood circulation, saturate tissues with nutrients and oxygen, and accelerate the regeneration process.
Distant phase
It is reasonable if rehabilitation after hip replacement takes place in a sanatorium at a later date. In addition to rehabilitation and physical education methods, which are implemented using various rehabilitation equipment and exercise equipment in the gym or in the aquatic environment, health clinics specialize in the use of natural healing sources, unique in their chemical and biological composition.
Start visiting the pool, it is very useful.
In sanatoriums, recovery after hip replacement is based on the use of peloid therapy courses (therapeutic mud applications) and balneotherapy in the form of brine (mineral), radon, carbon dioxide, pearl baths, etc. Swimming in the pool. Organic and inorganic substances contained in healing mud and waters penetrate into the body at the time of the treatment session and fruitfully contribute to:
- strengthening bones, increasing muscle endurance;
- resorption of skin, tendon, muscle scar formations, mobility increases not only at the site of the artificial joint, but also in other osteochondral organs;
- improving blood supply and nutrition in problem segments;
- eliminating swelling of soft tissue structures;
- getting rid of the pain factor, which often continues to disturb to one degree or another, even after a long time has passed from the moment of prosthetics;
- coherence of the central nervous system, mental harmony, positive attitude, normalization of sleep and daytime vigor.
Early period
It begins after surgery, lasts 3 weeks, and takes place in the hospital. Consists of two stages. Gentle - inflammation is observed in the area of the surgical intervention for 1-7 days. On days 7-15, the wound heals, this is called the tonic stage.
The patient is transferred from the operating room to intensive care. Heart rate, blood pressure, and breathing are constantly monitored. Antibacterial therapy is started and anticoagulants are administered.
What happens during this period:
- swelling decreases;
- blood circulation in the area of intervention is restored;
- postoperative sutures heal;
- the patient learns to sit and then get out of bed;
- The task of the medical staff is to prevent the occurrence of bedsores, thrombosis, pleurisy, and pneumonia.
What the patient needs to know:
- 2 hours after recovering from anesthesia, you must definitely go to the toilet; if you cannot do it yourself, the nurse will insert a catheter;
- for the first 3-4 nights you should not sleep on your side or stomach;
- You can start walking with crutches or a walker after 2-3 days, but only with an accompanying person;
- you can turn over on your side in a day, on your stomach in a week, while you need to spread your legs slightly to the sides, you cannot perform the movements yourself, only with the help of a nurse;
- you can sit down on the third day;
- Do not bend over or use a spoon to change shoes;
- stay in one position for no more than 20 minutes;
- Do not make sudden movements of the hip joint;
- for the hospital, choose shoes without backs;
- the operated leg can be bent at an angle of no more than 90 degrees;
- place a pillow between your knees, do not cross your legs;
- to sit up in bed, you need to lean on your hands;
- perform simple exercises to prevent congestion;
- When walking, do not lean on the operated leg.
Gymnastics for the early period:
- Move, bend and straighten the toes on both feet.
- Press down on the bed with your heels.
- Perform swings, circular movements with your arms, raise and lower your shoulders.
- Tighten the muscles of your healthy leg.
- Rotate and slightly bend the ankle of the operated leg.
- Slide your foot along the bed, bend your leg, pull it towards you.
- Move your legs away from each other one by one.
- Alternately, straighten your legs a few centimeters above the surface of the bed.
- Additionally, perform breathing diaphragmatic exercises.
Perform the first 5 exercises 6 repetitions every 10 minutes. After 2-3 hours, add exercises from the second part of the complex, do 10 repetitions. Perform all movements slowly and smoothly, inhale while tensing the muscles.
When the doctor allows you to get up and walk, you need to do other exercises:
- With emphasis on the headboard, lift your legs one at a time, bent at the knee.
- With emphasis on one leg, take the other one to the side and lift it slightly. Then change the supporting leg.
- The starting position is the same as in the previous exercise, but the leg is taken back. You need to feel how the hip joint works.
You should not lie in bed for a long time after surgery. This will lead to muscle contractures and other negative consequences. Before exercise therapy and training, you should not take painkillers.
Carrying out endoprosthetics: intervention algorithm
Before sending the patient on a gurney to the surgical ward, he will be asked to put on a compression stocking on the opposite leg, or bandage it up to the knee with an elastic bandage - this will prevent the formation of blood clots.
Next, the patient is given anesthesia - general or regional. Both types imply that the patient is in a state of medicated sleep, however, patient reviews of regional anesthesia are more optimistic - it is easier to wake up after it, and, in addition, even after waking up, pain relief continues for some time.
When the patient falls asleep, a catheter is inserted into his bladder.
The entire duration of the operation is usually 1-2 hours. In the process, the surgeon separates the damaged elements of the joint and installs artificial parts of the prosthesis in their place. To remove accumulated blood, a silicone drainage tube and a special “accordion” are installed in the wound to collect fluid from the postoperative wound.
After completing all the manipulations, the surgeon sutures the incisions, treats the wound and applies a certain type of bandage.
Late period
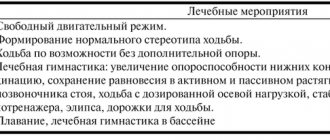
At this stage, rehabilitation after hip replacement takes place in the physical therapy room. You need to visit him immediately after discharge from the hospital. The goal is to restore the functionality of the limb, improve posture and the ligamentous-muscular center.
Stages and their duration:
- Early. It begins 2 weeks after the intervention and ends 2 months after the operation. At this stage, fusion of bone structures and the prosthesis occurs.
- Late. Terms - 60-90 days. Internal bone structures begin to recover.
In addition to physical therapy, from day 22 it is necessary to take walks. Walk with emphasis on a cane 3-4 times a day for 3-10 minutes, gradually increase the duration to 20 minutes. You can give up crutches and walkers when there are no problems with balance or self-doubt. This will take 1-2 months, depending on the method of fixing the prosthesis. Walking with a cane is necessary until the lameness disappears completely.
Exercise therapy for the late period, you will need a ball, an elastic gymnastic tape.
Exercises with tape:
- Secure one end of the tape to the door, the other to the shin. The back is straight, holding onto the support, stretch your leg forward.
- The starting position is the same. But raise your straight leg up.
- Do not change the starting position. Move your leg to the side.
Do all exercises smoothly 10 times.
Basic exercise therapy complex:
- Place the ball between your knees and squeeze rhythmically.
- While lying on your stomach, reach your buttocks with your heels.
- Starting position - lying on your back, knees bent, feet resting on the floor. Raise your pelvis, hold at the top point for a count of 5. Slowly return to the starting position.
- Lying on your back, alternately bend your legs, do not lift your feet off the floor.
- Lie on your stomach, slowly raise your straight leg, tensing the muscles of your buttocks. At the top point, fix the position for a count of 5. Return to the starting position and perform the exercise with the second leg.
- While sitting on a bed or chair, perform the “bicycle” exercise.
Do each exercise 6-10 times. Perform 2-3 approaches per day.
Functional recovery period
The longest stage lasts 3 months. During this time, subject to all rules, the femur acquires a normal anatomical shape and structure. It is better to stay in a sanatorium at this stage of recovery. Sanatorium treatment includes restorative physical education, therapeutic baths, mud applications, and exercises in the pool.
Treatment with mud and healing waters helps:
- strengthen bones, improve muscle endurance;
- get rid of scar formations;
- improve the mobility of all joints, blood circulation;
- eliminate swelling of soft tissues, pain;
- normalize the functioning of the nervous and immune systems, sleep, and mood.
At this stage, exercise equipment can be added to exercise therapy. On an exercise bike, lower the pedals so that your leg is completely straightened when moving. Pedal backwards or forwards for 15 minutes, 2 times a day. Gradually increase the time to half an hour, and the number of workouts to 3-4 per week. Walking backwards on a treadmill. Start at a speed of 1-2 km/h. Be sure to fully straighten your legs.
The day before surgery: what the patient can expect
To undergo endoprosthetics, the patient must be admitted to an inpatient clinic or hospital. After hospitalization, he is examined again by a therapist, a surgeon, and an anesthesiologist talks with him.
You should not drink alcohol the day before surgery. Meals during the day should be light, excluding foods that contribute to gas formation in the intestines.
10-12 hours before the start, it is forbidden to consume food and liquid. In the evening, you can do a cleansing enema and take a laxative.
The surgeon may require removal of hair from the surgical site, as well as removal of polish or gel coating from the nail plates.
Is it possible to carry out rehabilitation at home?
Rehabilitation after hip replacement at home is possible. But provided that there is a specialist in the family who has the necessary knowledge.
Benefits of home rehabilitation:
- you can study at a convenient time;
- classes in a familiar, comfortable environment;
- You can combine rehabilitation with work from home.
To avoid falls, you need to conveniently lay out all the necessary things so that you do not have to reach, secure or remove carpets. The house should have good lighting. Install special handrails in the bathtub. Despite all the advantages, rehabilitation should be carried out by specialists.
Minimally invasive and classical techniques
Orthopedists use classical or minimally invasive access techniques. Minimally invasive technology is based on making a small incision through a posterolateral or anterolateral approach. The length of the incision does not exceed 8 cm. The advantages include minimal trauma, which allows for shorter rehabilitation times and less painful recovery. However, minimally invasive technology is not widespread today due to the fact that it complicates the operating process due to insufficient visualization of the working field.
The size of surgical incisions with classical and minimally invasive techniques.
Suture after minimally invasive hip surgery.
In order to perfectly process and prepare the bones, and then flawlessly place the prosthesis, it is necessary to sufficiently expose the hip region. This is facilitated by a large incision of about 15 cm.
Nutrition rules
Within 6 weeks after the operation, the process of fusion of the head of the prosthesis with the pelvic bone occurs. The success of this process largely depends on proper nutrition. If the diet is not followed, the risk of dislocation of the head of the prosthesis, constipation, and enterocolitis increases.
Why is a diet prescribed after surgery?
- To normalize the functioning of the gastrointestinal tract. After application of anesthesia, temporary intestinal atony develops. You can only eat semi-liquid, pureed foods. These can be soups in vegetable broth with chopped dietary meat, slimy porridges. It is forbidden to consume any fast carbohydrates, fatty, fried, spicy foods.
- To compensate for blood loss. To restore the volume of circulating blood immediately after the end of anesthesia, you must regularly drink water in small sips. During the week you need to drink more, limit the daily amount of salt. To restore hemoglobin, consume foods high in iron, ascorbic acid, and vitamin B
- Strengthen the body's protective functions. Consume more fermented milk products to improve intestinal microflora.
- Accelerate the process of bone tissue restoration. The menu should include protein products.
Proper nutrition must be maintained even after rehabilitation is completed. This will help avoid excess weight gain and increased stress on the joint. Therefore, the basis of the diet is proteins, slow carbohydrates, and healthy fats.
Diet during rehabilitation:
- Proteins are necessary for the body to build its own proteins, collagen fibers of bone tissue. Sources of healthy animal protein include dietary meat and fatty fish. You definitely need to eat jelly and jellied meat - these dishes contain gelatin, which is a protein in its pure form. Plant sources of protein include soy, peas, beans, lentils, buckwheat and oatmeal.
- Complex carbohydrates. After endoprosthetics, you must give up sweets, pastries, white bread, and pasta. The menu includes foods with healthy carbohydrates - vegetables, grains, which contain few calories, but are rich in fiber and vitamins.
- Unsaturated fatty acids. After endoprosthetics, it is useful to consume foods with Omega-3 acids, which are found in fatty fish, crab meat, shrimp and red caviar. Unsaturated acids reduce the manifestations of the inflammatory process, cleanse blood vessels of harmful cholesterol, prevent the development of obesity, and accelerate wound healing.
- Bran as a source of fiber and vitamins. There is also a lot of fiber in flax seeds, dried mushrooms, and dried fruits.
- Calcium and vitamin D are essential to reduce the risk of osteoporosis and lysis. After endoprosthetics, it is necessary to consume 1-1.2 thousand mg of calcium per day. Sources: cheese, fish, sesame, almonds, herbs, garlic, hazelnuts. Calcitriol is required for normal calcium absorption. Vitamin D is found in cod liver, mushrooms, and egg yolk.
- Iron-rich foods. Chicken, shrimp, tuna, beets, pumpkin, nuts, buckwheat porridge.
Possible complications
In the absence of proper rehabilitation after hip replacement, negative consequences develop:
- decreased tone of injured muscles;
- formation of scars at incision sites;
- dislocation of the head of the prosthesis, inflammation of the nerve endings, fracture of the bone structures near the prosthesis.
Complications can also occur after surgery:
- bleeding in the area of suturing;
- displacement, rejection, destruction of the prosthesis;
- wound infection;
- limb asymmetry;
- pulmonary embolism;
- After the intervention, the pain does not go away for a long time.
Endoprosthetics are prescribed for hip fractures, coxarthrosis, osteonecrosis, and rheumatoid arthritis. Previously, these pathologies made a person disabled. But now, with proper treatment and compliance with rehabilitation rules, it is possible to completely restore the function and mobility of the joints.
Features of hip replacement surgery
The hip joint is formed by the head of the femur, which is connected to its body through the thinner neck of the femur, and the acetabulum. The latter is a cup-shaped depression in the pelvic bone. The head of the femur and the surface of the acetabulum are covered with thin, perfectly smooth hyaline cartilage, which is lubricated by the fluid produced by the synovial membrane. This ensures ease of sliding of the femoral head in the acetabulum and the ability to freely carry out movements in the hip joint.
If changes occur in any of these structures (hyaline cartilage, bones, synovial membrane) due to the action of certain factors, the functioning of the joint is inevitably disrupted. Initially, this is accompanied by pain, which tends to intensify over time, then restrictions on the range of motion are added and ultimately the joint may completely lose mobility. In such situations, different types of surgical interventions can be performed, but the most appropriate is hip replacement, since it ensures complete restoration of the functionality of the hip joint and provides the most lasting effect.
Hip replacement is a modern, high-tech operation that involves removing worn or damaged elements of the hip joint and installing an artificial endoprosthesis instead. They reproduce the anatomy of the hip joint as accurately as possible, which ensures complete restoration of its functions. At the same time, complications after endoprosthetics occur in less than 1-2% of cases, which is an extremely low figure. But in order for the operation to be successful, and for the installed endoprosthesis to function correctly and for a long time, it is better to carry it out in specialized centers where orthopedic surgeons have extensive experience in replacing hip joints.
Today, more than 500 thousand hip replacement surgeries are performed annually around the world, and patients respond very positively to the results. Example of a hip replacement surgery
The only drawback of endoprostheses is the need to replace them after 15-20 years (sometimes they last 30 years) or if the prosthesis fails prematurely due to traumatic or other factors. In such situations, a revision operation is performed and, if necessary, the endoprosthesis is replaced.
When is hip replacement required?
Hip replacement surgery has many indications. It is performed when conservative therapy can no longer ensure maintaining a person’s quality of life at a sufficiently high level, i.e., relieve him of pain and limitations in the mobility of the hip joint. In general, hip replacement is performed when:
- deforming arthrosis of the hip joint or coxarthrosis of 3-4 degrees, most typical for people of the older age category;
- degenerative-dystrophic changes in the hip joint against the background of rheumatoid or other similar systemic diseases;
- femoral neck fracture;
- neoplasms that have arisen in the area of the femoral head and acetabulum, requiring emergency removal;
- congenital or acquired hip dysplasia;
- aseptic necrosis of the femoral head, which can be a complication of degenerative changes in the joint or occur in isolation and then lead to the development of coxarthrosis.
In case of a hip fracture, especially in older people, endoprosthesis replacement is performed urgently, bypassing the stage of conservative treatment.
Types and progress of hip replacement
The tactics of the operation and the type of endoprosthesis are selected based on the nature of the damage to the hip joint. Even the endoprostheses themselves exist in different types. Thus, total endoprosthetics can be performed with a complete replacement of the hip joint or partial with the replacement of only the femoral head with an artificial prosthesis, etc.
Hip replacement takes on average 50-60 minutes. In most cases, the operation is performed under epidural or spinal anesthesia, although general anesthesia can also be used. In general, the essence of endoprosthetics can be reflected as follows:
- the patient is put under anesthesia using the chosen method and placed on his side on an orthopedic table;
- perform a longitudinal oblique incision along the intertrochanteric line 6-10 cm long;
- cut off the anterior part of the gluteus medius muscle from the greater trochanter of the femur and dissect the joint capsule;
- the head of the femur is removed from the acetabulum;
- resection and removal of the femoral neck is performed;
- using hemispherical cutters, the acetabulum is cleaned down to cancellous bone and a press-fit cup is inserted, as well as an individually selected type of liner (for total endoprosthetics);
- the end of the femur is brought out into the incision and a channel is formed in it for a seat for the wedge-shaped leg of the endoprosthesis (the size of the created channel must exactly match the size of the prosthesis leg, so its formation requires especially close attention and skill);
- the endoprosthesis leg is mounted into the femur;
- The endoprosthesis is fitted and the range of motion is checked;
- the head of the prosthesis is installed and adjusted into the preserved acetabulum or previously installed artificially;
- The wound is thoroughly washed with an antiseptic solution;
- the joint capsule, muscles, ligaments and skin are sutured in layers;
- The postoperative wound is covered with a sterile bandage.
The endoprosthesis can be installed using cement or in a cementless manner. In the first case, the surgeon uses special medical cement, which hardens in a matter of minutes. Typically, this technique is used to replace hip joints in elderly patients and those with osteoporosis.
With cementless fixation, the surfaces of the installed endoprostheses are characterized by the presence of roughness. Thanks to this, they firmly fuse with the bones, which takes about 3 months. This is the technique that is used most often.
Once again, we emphasize that it is better to entrust hip replacement surgery to orthopedic surgeons at specialized centers. After all, this operation requires a high level of skill.