Endoprosthetics of the hip or knee joint is the replacement of the affected joint with an artificial one. Pathology of the joint entails irreversible consequences in the form of limitation of movements up to and including disability. The patient is forced to constantly take medications that cause complications in the kidneys, liver, hematopoietic organs, and gastrointestinal tract.
Surgery can relieve pain, restore joint mobility, and prevent side effects of medications and disability. Surgery followed by rehabilitation can significantly improve the patient’s quality of life. But complications are possible during and after surgery. One of the most common consequences is leg swelling.
What is edema
Edema is the accumulation of fluid in organs and tissues. Why is this happening? According to the mechanism of formation, edema is:
- hydrostatic - as a result of increased pressure in the capillaries (due to poor circulation);
- hypoproteinemic – as a consequence of metabolic disorders (during prolonged fasting);
- membranogenic - caused by inflammatory processes, which leads to increased capillary permeability.
Based on localization, swelling is divided into:
- local - in a specific area of the body;
- general - cover all organs.
First, pre-edema develops - a significant accumulation of fluid in the body, then edema itself forms, which is visible to the naked eye (after pressing, a hole remains).
Fluid accumulation occurs due to hormonal imbalances. In diseases of the internal organs, there is an increased production of the hormone aldosterone, as a result, sodium ions and, as a result, fluid are retained in the body tissues.
In parallel with this process, the production of vasopressin, an antidiuretic hormone, increases, which leads to an increase in the absorption of water in the kidney tubules and the development of edema. Edema tissues after hip replacement surgery are hot to the touch, hyperemic, and painful when touched.
Knee replacement in the Czech Republic: guarantees, prices, rehabilitation, reviews and statistics.
Find out more
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
Why does swelling appear after endoprosthetics?
Swelling after surgery may appear for the following reasons:
- Hematogenous - penetration of pathogenic microorganisms into the blood when the operated site is infected, causing inflammation, accompanied by pain and swelling of the tissues.
- Lymphogenous - the infection enters the lymph nodes, which leads to inflammation and swelling.
- Thrombosis of the veins of the lower extremities is caused by stagnation of blood due to immobility of the joints.
- Damage to the prosthesis or change in its position - as a result of a fall or impact.
- Rejection of a prosthesis by the body is the incompatibility of the materials from which the prosthesis is made with the tissues of the body, which leads to inflammation and swelling.
The latter reason is quite rare, since research is constantly being carried out on new materials for prosthetics that provide maximum strength, compatibility and painlessness. Prostheses are made from special metal alloys, ceramics and heavy-duty polyethylene. Rejection occurs only when the body reacts individually to the components of the prosthesis.
The main cause of swelling is damage to tissues and small vessels during surgery, so a complete absence of swelling after surgery is impossible!
Clinical example No. 3
Patient Z., 28 years old, came to the clinic in September 2017, injured 7 years before treatment as a result of an accident, he received a fracture of the acetabular cavity, complicated by osteomyelitis, sanitation of the joint was performed, followed by arthrodesis. Walking was carried out using the lumbar spine.
Due to the lack of movement in the hip joint, active lifestyle and young age of the patient, a decision was made to perform total hip replacement. This type of operation is an extremely complex orthopedic intervention.
Another category of patients who are indicated for total hip replacement are patients with femoral neck fractures, especially subcapital fractures. For this category of patients, it is critical to perform surgery as quickly as possible, since, taking into account age and concomitant pathology, the risk of complications increases with every hour that passes from the moment of injury.
What is done in a hospital setting to prevent or reduce swelling
To avoid the occurrence of edema, the following measures are carried out in a hospital setting:
At the stage of preparation for surgery:
- carrying out therapy for chronic diseases until complete remission is achieved;
- clinical examination of the patient, laboratory and instrumental diagnostics to exclude inflammatory processes;
- within 2 hours, broad-spectrum antibiotics are used that act against pathogens of many infections;
- 12 hours before surgery, anticoagulants are prescribed - blood thinners (heparin) to prevent thrombosis;
- thorough disinfection of the operating room.
During the operation, it is performed in a highly professional manner with minimal trauma under sterile conditions. Individual selection of a prosthesis taking into account the age and condition of the patient. The prosthesis must be made from materials that are optimally compatible with body tissues. Prosthetics must be carried out in such a way that the integrity of the implant is not compromised and infection and inflammation do not occur.
In the postoperative period:
- continuation of therapy with antibiotics and anticoagulants for another 5 - 7 days after the intervention;
- the beginning of rehabilitation from the first day to avoid blood stagnation and the development of edema - exercise therapy, physiotherapy, breathing exercises;
- professional wound treatment to prevent infection;
- in case of swelling (usually on the 2nd - 3rd day) - elimination of the cause that led to the problem, the use of diuretics, ointments and gels that reduce swelling, a special set of therapeutic exercises;
- specialists perform lymphatic drainage - alternating light stroking of the skin and deep massage of the lymph nodes;
- training the patient to perform exercise therapy at home, informing about possible complications and preventive measures to prevent them.
Compression cuffs to prevent swelling and thrombosis.
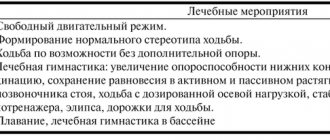
Rehabilitation after hip replacement
Memo to a patient who has undergone hip replacement
You have undergone a complex, high-tech intervention. Doctors have restored the damaged structures of your hip joint, but the surgery is only half of the way to restoring movement in the joint. Your goal is to fully adapt to stress at home and at work, and continue to lead an active lifestyle.
This instruction will help you properly restore your activity step by step. Unless your doctor orders otherwise:
First day after surgery
With the doctor's permission and under the supervision of an instructor, we sit on the bed and dangle our legs. No need to fall over on the side of the healthy or operated leg!!!
Exercises that must be performed from the first day after surgery.
1. Move the feet of both legs towards you, holding them in this position for 2-3 seconds, and then away from yourself and holding them for 2-3 seconds. Tension of the feet should be done “at half strength” and avoid the appearance of sudden pain. Repeat 10 times. Perform 5 times a day.
2. Tension the quadriceps muscles of both thighs, pressing your knees to the bed for 3-5 seconds. Repeat 10 times. Perform 5 times a day.
3. Squeeze your buttocks together, tensing your gluteal muscles, for 3-5 seconds. Repeat 10 times. Perform 5 times a day.
4. Bending the healthy leg at the knee joint. Repeat 10 times, perform 5 times a day.
5. Raising the pelvis with support on the elbows and foot of the healthy leg. The healthy leg is bent at the knee joint, the operated leg is straight. Repeat 10 times. Perform 5 times a day.
Second day after surgery
With the doctor's permission and under the supervision of an instructor, we get out of bed and walk around the ward with the support of rehabilitation equipment.
How to walk with crutches .
First, crutches are placed, then the operated leg (when stepping, we first bend the leg at the knee), then the healthy one. It is necessary that from the first steps the correct movement pattern be developed: first the heel touches the floor, then the foot, then the toes. You need to move rhythmically and calmly, without rushing.
“Rule of the triangle”: the healthy leg should never be on the line of the crutches - it is either in front of or behind the line connecting the support points of the crutches. First, we try to walk with an “added step”: when performing a step with crutches, the operated limb is brought to the line of the crutches and placed on the floor without transferring the weight of the body to it. Then the body weight is transferred through the hands to the crutches, and an extension step is performed with the healthy leg, after which a step with crutches is performed again, etc.
We bend the affected leg at the knee, lift it above the floor and place it on the heel, fully straightening the leg.
Exercises that must be performed from the second day after surgery.
1. We continue to do the exercises of the first day.
2. Lying in bed, lift up 30 degrees, alternately, first with the healthy leg, and then with the operated leg (the operated leg with the help of a crutch). Repeat 10 times, perform 5 times a day.
3. Lying in bed, abduction to the side by 20-30 degrees, first with the healthy leg and then with the operated leg (operated leg with the help of a crutch). Repeat 10 times, perform 5 times a day.
4. Bending the operated leg at the knee joint. Repeat 10 times, perform 5 times a day.
5. Legs straight, feet towards you. Simultaneously pulling down (lengthening) one leg and shortening the other (imitation of walking). Repeat 10 times, perform 5 times a day.
6. Bend the healthy leg at the hip and knee joints, pull it towards the stomach with your hands, and press the heel of the operated leg on the bed for 10–15 seconds until you feel slight pain. Repeat 5 times, perform 5 times a day.
7. Bend your healthy leg at the knee joint (the operated leg is straight), slowly lift your pelvis, resting on the foot of the healthy leg and the heel of the operated leg, hold for 5 seconds, then slowly lower your pelvis. Repeat 5 times, perform 5 times a day.
8. In a sitting position, bend and straighten your legs at the knee joints, holding them in an extended state for 5 seconds. Repeat 10 times. Perform 5 times a day.
4-5 days after surgery
With the doctor's permission and under the supervision of an instructor, we walk with crutches along the corridor and up the stairs.
How to walk down stairs (with crutches).
1. Crutches (crutch).
2. Operated leg.
3. Healthy leg.
How to walk up the stairs (with crutches ).
1. Healthy leg.
2. Operated leg.
3. Crutches (crutch).
Exercises that need to be performed from 4-5 days after surgery. Perform 5 times a day.
Starting position - lying on your back, feet shoulder-width apart, arms along the body.
1. Raise your straight arms up and to the sides - inhale, lower - exhale. Repeat 3 times.
2. Feet towards yourself, away from you. Repeat 10–30 times.
3. Arms to the sides. The healthy leg is bent. With your support on the foot of the healthy leg and the heel of the operated leg (the operated leg is straight), and also slightly on your elbows, lift your pelvis and hold the position for 3–5 seconds. Repeat 6 times.
4. Alternately bend your legs at the knee joints, sliding your feet along the couch. 10–20 bends.
.
5. Alternately move your straight legs to the side while maintaining the position. Monitor the position of the foot (foot towards you). Repeat 6 times.
6. Alternately lift your straight legs (not high) and hold them for a count of 3–4. (foot towards yourself). Repeat 6 times.
7. Imitate walking at a slow pace. Legs straight, feet towards you, simultaneously pulling down (lengthening) one leg and shortening the other. Repeat 10 times.
8. Isometric tension (without movement) of the gluteal muscles for 5–7 seconds (repeat 10–15 times).
Starting position: lying on your healthy side (pillow between your legs).
1. Raise the straight, operated leg and hold the position for 3-5 seconds. (foot towards yourself). Repeat 5-8 times.
Starting position: sitting on a chair.
1. Alternately straighten your legs at the knee joints and hold the position for 5 seconds. Repeat 10 times.
Starting position: standing.
1. Hands on a support. Raise on your toes with tension in your buttocks and maintaining balance for 3-5 seconds. Repeat 10 times.
2. Bend the operated leg at the hip and knee joint. Make sure that the shin does not go back. Repeat 6 times.
3. Exercise “Rumba” - feet shoulder-width apart, slowly transfer the weight of the body from one leg to the other, and there should be no pain in the operated leg. Repeat 10 times.
4. Move the operated leg to the side and return to its original position. Move your operated leg back and return it to its original position. Leg straight, foot towards you. 10 times.
Exercises of the 5th day. Performed while sitting on a chair.
1. “Sliding” the feet back and forth along the floor in turn. When the foot moves forward, the toe is pulled towards itself. You can help with your hands, pressing lightly on the operated knee as you move your foot forward.
2. Sitting on a chair, stretch your legs forward, toes towards you, tense your leg muscles, while simultaneously pressing your hand on the operated knee. Hold the tension in the muscles for 30 seconds, then relax the muscles.
3. Roll your feet on the floor from toe to heel. In one direction (both feet first on the heels and then on the toes) and in the opposite direction (one foot on the toe and the other on the heel).
4. Move your thigh to the side, “waddling” your foot from toe to heel on the floor, hold your thigh in the abducted position for 10 seconds, bring your leg to the previous position, also “waddling” with your foot. Perform first with the healthy leg, then with the sick one.
5. Using the movement of your buttocks, “crawl” deeper into the chair and return to your previous position.
6. Exercise No. 1 + simultaneous raising and lowering your arms in front of you. When the left leg goes forward, the right hand goes up, and vice versa.
7. Exercise No. 2 + turning the hands over with the palm and back on the knees: left foot on the heel, right on the toe, left hand with the back on the knee, right hand with the palm on the knee, then vice versa.
8. Sit on the edge of a chair, lean back, straighten your legs forward. Movement of the toes of the feet back and forth. The operated leg can be supported with your hand.
9. We remain on the edge of the chair with our legs extended forward. Circular movements of the feet in one direction and the other.
10. Place a ball under the foot of the healthy leg. Roll the ball back and forth across the floor with your foot. Repeat with the sore leg. Perform without shoes.
11. Place the ball between the feet apart. We “pass” the ball from one foot to the other.
12. We hold the ball between our feet and lift the ball up using our knees. And then at the hip joints, we lower the ball.
Exercises that need to be performed from 6-7 days after surgery.
We continue to perform the exercises of the previous days.
Exercises 6-7 days. Performed while standing, holding hands on a stationary support.
1. Transferring body weight from the left leg to the right without lifting the feet off the floor.
2. Standing on the healthy leg, we swing the operated leg straight back.
3. Standing on the healthy leg, we swing the straight operated leg to the side.
4. Standing on the healthy leg, we swing the operated leg, bent at the knee, forward, and then straight back.
5. Standing on the healthy leg, we move the operated leg to the side, bent at the knee joint.
What you can and cannot do after surgery
| NOT TO DO | YOU CAN DO |
| 1. It is forbidden cross your legs! — You can’t sleep on your healthy side without a cushion between your legs - You can’t sit cross-legged | 1. Roller between legs - when we sleep on our healthy side - when we sleep on our back - when we sit, our legs should be 10-15 cm wide |
| 2. It is forbidden bend the leg at the hip joint more than 90 degrees! - You cannot sit on low beds and chairs — You can’t sit on a low toilet - You can’t bend forward with straight legs | 2. — High beds and chairs — Toilet nozzle Or — when we sit down, we move the operated leg forward — when bending forward, we move the operated leg back - wearing shoes only with a long spoon |
| 3. You cannot rotate the operated leg in the hip joint internally or externally. | 3. Turn on the healthy leg towards the operated side |
| 4. You can’t sleep on your operated side. | 4. Sleep on your healthy side with a bolster |
| 5. — It is forbidden turn on your stomach in the first 3 weeks after surgery. — You can’t turn on your stomach without a bolster 6. Limitation of sexual life for up to 6 weeks. 7. Physiotherapy should never | 5. - Sleep on your stomach from 3 weeks -turn over your healthy side with a roller 6. Sexual life 6 weeks after surgery. Poses that do not lead to dislocation of the hip joint are acceptable. |
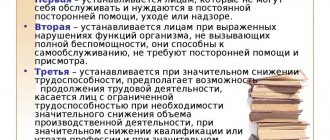
General issues of rehabilitation
The total rehabilitation time takes about 3 months. Of these, the first 6-8 weeks you need to walk with crutches , then 4 weeks with a cane . The cane is held on the side of the healthy leg.
Dressings after surgery are carried out daily. If the integrity of the bandage is damaged, restore it as quickly as possible. Usually the doctor recommends removing the stitches on the 14th day after surgery. You can wet the seam (take a shower) 2 days after removing the seams, but do not rub it with a washcloth.
Pain after surgery subsides by 3-5 days. A common cause is tissue swelling at the site of the operation. The more swelling, the more pain.
The pain usually intensifies in the evening. An elevated position of the leg and the use of an elastic bandage help reduce swelling and pain. For a while, place your leg higher - on a pillow, bolster. Move your feet (toes “away from you - towards you”). Take pain medication if necessary.
Hot bath, steam bath or sauna – 6 months after surgery.
You can drive a car 6-8 weeks after surgery (after you stop walking with crutches).
The elastic bandage must be used for 6-8 weeks after surgery. Instead, it is possible to use compression hosiery of class I compression.
You can check the recommendations with a rehabilitation specialist or your attending physician. Do not do exercises if you doubt the correctness of their implementation - seek help from a physical therapy instructor or your doctor.
Before removing the sutures, avoid movements in the operated joint that cause severe pain.
Contact your doctor if:
- Pain in the operated joint continues for more than 2 weeks after surgery. With increased swelling and bruising.
- An injury occurred in the area of the operation.
- The temperature rose to more than 38 degrees.
What will make rehabilitation at home easier?
- Firmly fixed grab bars in the bathroom or shower.
— Strong handrails along all stairs.
— A stable chair with a strong back, two armrests and a firm seat to keep your knees below the level of your hip joints.
— High seat in the toilet.
- A stable bench in the shower or a chair in the bathroom.
— A washcloth with a long handle.
— Shoe spoon with a long handle.
- Help when putting on socks, a long spoon for putting on and taking off shoes without excessive flexion of your new hip joint.
- Assistive devices to help you grasp objects without excessive hip flexion.
- A durable cushion to keep your knees below your hips while sitting for chairs, sofas and cars.
— Removing loose carpets and electrical wires from the area where you walk.
What to do at home
After surgery to replace the hip joint, in the absence of complications, the patient is discharged on days 8–10. If swelling persists by this time, it is necessary to carry out complex treatment at home, including drug therapy, folk remedies, exercise therapy, massage and diet.
Traditional treatment includes taking diuretics (Veroshpiron, Furosemide, Diacarb). It should be taken into account that, in addition to Veroshpiron (potassium-sparing), other drugs in this group remove potassium along with the liquid. Therefore, drugs containing potassium (Potassium orotate, Asparkam) are simultaneously prescribed. Medicines are taken orally according to a special regimen; in case of severe swelling, injections are given.
Ointments and gels that normalize fluid circulation in tissues (Troxevasin, Heparin ointments, Essaven gel) are indicated locally.
Traditional medicine uses decoctions, infusions, compresses, and baths. Folk remedies are only an addition to the main therapy. Before using traditional medicine, you should consult your doctor.
Therapeutic gymnastics and massage
The exercise therapy complex is selected individually for each patient by hospital specialists. The complexity of the exercises depends on the etiology of the edema, the severity of the operation, the condition and age of the patient. Upon discharge, the complex continues to be carried out at home. General rules:
- perform exercises at a slow and smooth pace;
- combine exercises with breathing exercises to avoid pulmonary edema;
- do gymnastics in the first days only on your back, and then while sitting in bed.
- Walk barefoot at home every day for 10-15 minutes, alternating with raising on your toes.
An addition to the treatment of edema is massage, which helps normalize blood circulation. Classic – improves lymph outflow, increases the drainage properties of intercellular tissue. Cold is carried out with ice cubes and medicinal herbal decoctions.
Discharge home
While at home, you need to continue doing therapeutic exercises and follow the recommendations of your doctor.
Also, take basic precautions at home. Wear low-heeled shoes, temporarily remove moving rugs and wires from the floor, walk carefully on wet surfaces, and try to prevent pets from getting under your feet. Do your homework as much as you can. Alternate the time of work, rest, and gymnastics. Try to go for walks with the help of relatives and friends.
Recommendations for swelling
To achieve optimal effect, you must follow these recommendations:
- Follow a diet - reduce salty and spicy foods that retain fluid in the body, add fruits and vegetables that have a diuretic effect. If it is well tolerated, eat more fermented milk products. Eat at regular intervals, without large intervals, in small quantities.
- Keep the swollen leg elevated.
- Reduce physical stress on the hip joint.
- Do not take hot baths, which cause swelling, take a contrast shower, which improves blood circulation.
- Try to avoid direct sunlight.
- Wear comfortable shoes.
- Use compression hosiery (socks, tights), which improves blood circulation in the extremities.
- Avoid drinking alcohol.
If swelling persists for more than a month, despite therapeutic measures taken; If you develop fever or other signs of inflammation, you should immediately consult a doctor.
Clinical example No. 4
Patient R., 74 years old, was brought to the K+31 clinic by an ambulance team in September 2021, injured 3 hours before admission, at home, fell on her left side.
She was hospitalized in the Russian Academy of Education, examined, water and electrolyte disturbances were corrected for 5 hours, after which the patient was taken to the operating room. Total endoprosthetics of the left hip joint was performed.
On the second day of hospitalization, the patient was transferred to the hospital ward. In K+31, patients in this category are provided with the highest possible comfort and safety in the early postoperative period by providing single rooms with an individual nurse. After a course of dressings, antibiotic prophylaxis, and physical therapy, the patient was discharged for outpatient follow-up treatment.
Another category of patients for whom total hip replacement is indicated are patients with congenital hip dislocation. When treatment for congenital hip dislocation is not carried out, or is carried out incorrectly, underdevelopment of the entire proximal femur and acetabular cavity occurs. Due to the reduced area of the articular surface, the load on them increases significantly, which leads to the early development of coxarthrosis.