Studies show that complications after hip replacement develop in 1% of young people and 2.5% of older patients. Despite the miniscule likelihood of developing negative consequences, they can affect anyone, and especially those who did not strictly follow the rehabilitation program.
Image of the position of the endoprosthesis in the human body.
Complications after hip replacement are caused by improper postoperative care and physical activity after discharge from the hospital. The second reason is the mistakes of the surgeon. And third, this is an incomplete preoperative examination, as a result of which hidden infections (tonsils, cystitis, etc.) were not cured. The success of treatment is influenced by the qualifications of the medical staff, where the patient received high-tech medical care - surgical and rehabilitation treatment.
The pain varies, but there is “good” pain – after moderate physical activity. And there is a “bad” one, which speaks of problems that need to be urgently diagnosed.
Complication statistics as a percentage
Surgery to install a hip joint prosthesis is the only method that “puts” the patient back on his feet, relieves him of debilitating pain and limited ability to work, and allows him to return to healthy physical activity. Unpleasant pathological situations associated with implantation occur infrequently, about which the patient should be informed. According to ongoing randomized controlled trials, the following data were obtained:
- dislocation of the head of the prosthesis develops in approximately 1.9% of cases;
- septic pathogenesis – in 1.37%;
- thromboembolism – in 0.3%;
- periprosthetic fracture occurs in 0.2% of cases.
They develop not through the fault of the surgeon, but of the patient himself, who did not continue rehabilitation or did not adhere to a special physical regimen after the end of recovery. The deterioration of the condition occurs at home, when there is no close monitoring from doctors that was in the clinic.
Minimally invasive endoprosthetics in the Czech Republic: doctors, rehabilitation, terms and prices.
Find out more
Not a single orthopedic specialist, even with rich and impeccable work experience, can 100% predict how a particular body will behave after such complex manipulations on the musculoskeletal system, and give the patient a complete guarantee that everything will go smoothly and without incidents.
How to prevent the problem
If you decide on joint replacement, be prepared for regular visits to doctors and clinical examinations. Periodic x-rays will help to identify the problem in advance - changes in bone tissue or implant. You should sound the alarm at the slightest hint of “problems” in the endoprosthesis - disturbances in its functions, redness, swelling.
If you have not yet decided on a treatment method for arthrosis or osteoarthritis, consider an alternative option that does not cause complications and has a minimum of contraindications. Intra-articular injections of Noltrex, a synovial fluid substitute, are indicated for arthrosis of the second and even third degree. The course includes several injections at weekly intervals, after which the viscosity of the joint fluid is restored, the cartilage stops rubbing against each other - the patient can return to their usual lifestyle for a long period.
Unlike surgery, Noltrex intra-articular injections are not hazardous to health and do not require significant effort from you during the recovery period. Infection and postoperative complications are excluded if you complete the course in a medical office, under ultrasound control, at the recommended frequency. The operation, in turn, is a huge risk, and it does not matter at all whether it is emergency or planned.
Differentiation of pain: normal or not
Pain after hip replacement will be observed in the early period, because the body has undergone a serious orthopedic operation. The painful syndrome during the first 2-3 weeks is a natural response of the body to a recent surgical injury, which is not considered a deviation.
Until the surgical injury heals, the muscle structures return to normal, until the bones and the endoprosthesis become a single kinematic link, the person will experience discomfort for some time. Therefore, a good pain reliever is prescribed, which helps to cope with early painful symptoms more easily and to better concentrate on treatment and rehabilitation activities.
Well-healing suture after surgery. It is smooth, pale and has no discharge.
Painful sensations must be differentiated and examined: which of them is normal and which is a real threat. This can be done by the operating surgeon. The patient’s task is to notify the orthopedic doctor if there are any uncomfortable signs.
Clinically Relevant Anatomy
Clinically Relevant Anatomy
The hip joint is a ball-in-socket joint. This means that the head of the femur, which is the “ball,” is located inside the acetabulum, the “socket.” This connection of the femur and pelvis allows for multi-axis movements of the hip. The acetabulum has the shape of a cup, inside which the head of the bone rotates with a fairly large degree of freedom. The head is enclosed by the acetabulum beyond its maximum diameter. The head and the inner surface of the cavity are covered with a thin layer of cartilaginous tissue. Once this layer is completely worn out or damaged (usually occurring with arthritis), the surfaces of the bones become highly sensitive to friction, leading to pain, decreased mobility, and possible shortening of the affected leg. Replacing these surfaces is aimed at eliminating pain and immobility, as well as returning the patient to the ability to lead an active life without physical discomfort.
Main risk factors
Surgical intervention does not exclude complications, and serious ones at that. Especially if mistakes were made during the intra- and/or postoperative period. Even small errors during surgery or during rehabilitation increase the likelihood of unsatisfactory hip arthroplasty. There are also risk factors that increase the body’s susceptibility to postoperative consequences and often become their cause:
- advanced age of a person;
- severe concomitant disease, for example, diabetes mellitus, arthritis of rheumatoid etiology, psoriasis, lupus erythematosus;
- any previous surgical intervention on the “native” joint aimed at treating dysplasia, femoral fractures, coxarthrosis deformities (osteosynthesis, osteotomy, etc.);
- re-endoprosthetics, that is, repeated replacement of the hip joint;
- local inflammation and purulent foci in the patient's history.
It should be noted that after hip joint replacement, elderly people are more susceptible to complications, and especially those over 60. In addition to the underlying disease, elderly patients have concomitant pathologies that can complicate the course of rehabilitation, for example, reduce resistance to infection. There is a reduced potential for reparative and restorative functions, weakness of the musculo-ligamentous system, osteoporotic signs and lymphovenous insufficiency of the lower extremities.
It is more difficult for older people to recover, but this can be done successfully.
Diagnostics
Diagnosis of patients requiring total hip replacement is carried out mainly on the basis of existing symptoms. Pain, decreased range of motion, and dysfunction are the most common. For patients complaining of hip pain, it is also necessary to carry out a comprehensive differential diagnosis, because often it can indicate diseases of the spine and pelvis, but have no connection with the hip joint. The surgeon must lead the diagnostic process and its organization.
Read about examination of patients with hip joint problems here.
The consultation with the surgeon should include the following elements:
- Observation.
- Patient interview:
- Complaints of pain, deformity, stiffness and/or lameness.
- Previous diseases associated with hip pain (congenital or childhood diseases, past injuries).
- Physical examination:
- In a standing position.
- Trendelenburg test.
- While walking.
- Lying on your back (including measuring leg length).
- Objective observation (posture, deformities, muscle atrophy).
- Assessment of range of motion.
Special research methods
- X-ray examination. This method is used primarily, and in most cases only X-ray examination is necessary, since it is this that makes it possible to make a large number of diagnoses when there is a need to replace the hip joint. Its results will determine the need for further research.
- Other methods: computed tomography, magnetic resonance imaging.
Concept and methods of treating consequences
Symptoms of complications after hip replacement will be presented below in the table for better understanding. A quick visit to a doctor at the first suspicious signs will help to avoid the progression of adverse events, and in some situations, to save the implant without revision surgery. The more advanced the clinical picture becomes, the more difficult it will be to respond to therapeutic correction.
Dislocations and subluxations of the endoprosthesis
Negative excess occurs in the first year after prosthetics. This is the most common pathological condition in which the femoral component is displaced in relation to the acetabular element, resulting in separation of the head and cup of the endoprosthesis. Provocative factors are excessive loads, errors in the selection of the model and installation of the implant (defects in the placement angle), the use of a posterior surgical approach, and trauma.
Dislocation of the femoral component on x-ray.
The risk group includes people with hip fractures, dysplasia, neuromuscular pathologies, obesity, joint hypermobility, Ehlers syndrome, and patients over 60 years of age. Individuals who have undergone surgery on a natural hip joint in the past are also particularly vulnerable to dislocation. The dislocation requires non-surgical reduction or open repair. If treated in a timely manner, it is possible to adjust the endoprosthetic head using a closed method under anesthesia. If the problem continues, the doctor may prescribe a repeat operation to reinstall the endoprosthesis.
Paraprosthetic infection
The second most common phenomenon, characterized by the activation of severe purulent-inflammatory processes in the area of the installed implant. Infectious antigens are introduced intraoperatively through insufficiently sterile surgical instruments (rarely) or after intervention they move through the bloodstream from any problematic organ that has a pathogenic microbial environment (often). Poor treatment of the wound area or poor healing (in diabetes) also contributes to the development and proliferation of bacteria.
Discharge from a surgical wound is a bad sign.
A purulent focus has a detrimental effect on the strength of fixation of the endoprosthesis, causing its loosening and instability. Pyogenic microflora is difficult to treat and, as a rule, requires removal of the implant and re-installation after a long time. The main principle of treatment is a test to determine the type of infection, long-term antibiotic therapy, and abundant lavage of the wound with antiseptic solutions.
The arrows indicate areas of infectious inflammation, this is exactly what they look like on an x-ray.
Thromboembolism (PE)
PE is a critical blockage of the branches or main trunk of the pulmonary artery by a detached thrombus, which formed after implantation in the deep veins of the lower limb due to low blood circulation resulting from limited mobility of the leg. The culprits of thrombosis are the lack of early rehabilitation and necessary drug treatment, prolonged stay in an immobilized state.
This complication is dealt with quite successfully at this stage of medical development.
Blocking the lumen of the lungs is dangerously fatal, so the patient is immediately hospitalized in the intensive care unit, where, taking into account the severity of the thrombotic syndrome: administration of thrombolytics and drugs that reduce blood clotting, NMS and mechanical ventilation, embolectomy, etc.
Periprosthetic fracture
This is a violation of the integrity of the femur in the stem area with an unstable and stable prosthesis, occurring intraoperatively or at any time after surgery (several days, months or years). Fractures more often occur due to reduced bone density, but may be the result of incompetent development of the bone canal before installing an artificial joint, or an incorrectly chosen method of fixation. Therapy, depending on the type and severity of the damage, consists of using one of the methods of osteosynthesis. The leg, if necessary, is replaced with a more suitable configuration.
Implant failure occurs very rarely.
Sciatic nerve neuropathy
Neuropathic syndrome is a lesion of the peroneal nerve, which is part of the structure of the greater sciatic nerve, which can be caused by lengthening of the leg after prosthetics, pressure of the resulting hematoma on the nerve formation, or, less commonly, intraoperative damage due to careless actions of the surgeon. Nerve restoration is performed through etiological treatment with the optimal surgical method or through physical rehabilitation.
When an inexperienced surgeon works, there is a risk of injury to the femoral nerves.
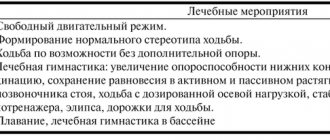
Rehabilitation after hip replacement
Your doctor, based on the results of the postoperative period, the extent of surgical intervention, and X-ray data, will determine your individual rehabilitation program. Since revision endoprosthetics is a major traumatic operation, recovery after it can be quite slow. The date when a patient can begin walking without crutches with full weight bearing on the leg depends on many factors and is determined individually by your doctor. In some cases, the rehabilitation period can last up to one year. After revision endoprosthetics, follow-up with an orthopedic surgeon is necessary, which consists of periodic preventive examinations and diagnostic studies.
Symptoms in the table
| Syndrome | Symptoms |
| Dislocation (impaired congruence) of the prosthesis |
|
| Local infectious process |
|
| Thrombosis and pulmonary embolism (thromboembolism) |
|
| Periprosthetic bone fracture |
|
| Lesser tibial nerve neuropathy |
|