Procedure information
Exercise therapy after knee arthroscopy
Alcohol after knee arthroscopy
Rehabilitation after shoulder arthroscopy
Rehabilitation after arthroscopic knee surgery
Learn more
Bandage after arthroscopy of the shoulder joint
Learn more
Free movement of human joints occurs with the help of a complex system of joints consisting of menisci, muscular apparatus, synovial fluid, joint capsule and much more. If the functioning of at least one element is disrupted, it becomes difficult for a person to move a limb, and a disease of the musculoskeletal system occurs.
Arthroscopy is a minimally invasive procedure performed to diagnose damage within a joint and for therapeutic or surgical purposes. Arthroscopic interventions are performed on any of the joints.
Types of intervention
1. Knee arthroscopy is one of the most common types of this intervention. When moving, the knee takes on a huge load, which gradually disrupts the normal processes in the joint and contributes to inflammation and destruction. Both diagnostic and therapeutic procedures are recommended mainly for ligament ruptures, meniscus damage, arthrosis, etc. Knee arthroscopy is also performed before surgery to replace a damaged joint.
2. Arthroscopy of the shoulder joint. The shoulder joint is also often injured during sports. Arthroscopy is performed as a diagnostic and therapeutic procedure for rotator cuff and labral tears. The operation is also minimally invasive.
3. Arthroscopy of the elbow joint. Arthroscopy of the elbow joint is performed for both diagnostic and therapeutic purposes. The elbow joint can be injured by a fall or destroyed due to arthritis or arthrosis.
The procedure is not performed at Garant Clinic.
3. Arthroscopy of the hip joint. Hip pain syndrome can occur for many reasons. Most problems are caused by diseases that can affect several parts of the joint at once. It is in order to identify a clear picture of the disease that arthroscopic intervention is performed in this joint. Therapeutic arthroscopy of the hip joint is performed only after a complete diagnosis.
The procedure is not performed at Garant Clinic.
4. Arthroscopy of the ankle joint. Ankle arthroscopy involves a minimally invasive endoscopic intervention using special equipment. Due to the fact that the operation does not require significant damage to surrounding tissue, the consequences are minimal, and most patients tolerate it well.
The procedure is not performed at Garant Clinic.
For any type of intervention, a person must undergo standard preoperative preparation, and afterward, recovery procedures. A set of rehabilitation measures is selected individually for each patient.
Arthroscopy is also used for diagnostic purposes for arthritis or arthrosis, since this method allows the doctor to see the condition of the diseased area from the inside.
Why do you wrap your legs with an elastic bandage before surgery?
Surgery is a serious stress, during which the clotting ability of the circulatory system increases. An increase in blood viscosity can lead to the formation of blood clots, and it is moderate compression that helps prevent their occurrence. To reduce the risk of complications (formation of blood clots and air emboli) in people at risk of developing embolism, their legs are bandaged before surgery.
The application of compression bandages is possible not only in the pre-, but also in the postoperative period. In particular, this applies to cases of vein removal.
Prices
Treatment of Hallus Valgus (“bones” on the leg). One leg - 70,000 rub. Two legs - 120,000 rub.
Arthroscopy of the knee joint—from 35,000 to 150,000 (excluding anesthesia, hospitalization and consumables) depending on the volume of the operation. Consultation with a GarantKlinik specialist is required.
Arthroscopy of the shoulder joint - from 30,000 to 65,000 rubles (excluding anesthesia, hospitalization and consumables) depending on the volume of the operation. Consultation with a GarantKlinik specialist is required.
GarantKlinik is the base of the Sechenov Moscow State Medical University, so our prices are similar to the state ones.
Preliminary preparation:
- Conduct an initial examination by a specialist. For arthroscopy, this will be an appointment with an orthopedist.
- Conduct general blood and urine tests.
- Undergo x-ray examinations of the lungs and the area of the affected joint. In some cases, several x-rays in different planes may be required.
- Blood chemistry. It is taken from a vein on an empty stomach.
- Blood clotting test. As a rule, additional blood sampling is not required for this analysis; it is carried out on an already existing amount of biomaterial.
- Test for HIV, hepatitis B and C, syphilis. The need for these tests is related to the safety of both the patient and the personnel performing the operation.
- ECG and examination by a cardiologist. This is necessary to study the reaction of the patient's heart to the effects of anesthesia or sedation.
- Magnetic resonance imaging or computed tomography. They are done if indicated or if a more detailed examination of the condition of the joint is necessary.
- Ultrasound of the veins of the lower extremities. Ultrasound is indicated if there are suspicions of varicose veins.
If there is a suspicion of cancer, then all diagnostic measures are taken to examine malignant tissues. In this case, surgery can only be performed after a full course of radiation therapy and chemotherapy, as well as after the body has fully recovered after treatment. Otherwise, even such a minimally invasive operation can lead to a significant deterioration in the patient’s condition.
Removal of leg veins: low prices, high quality!
If you suspect varicose veins, contact our doctor immediately. At an early stage, conservative treatment methods can still be used:
- compression jersey,
- specific drugs,
- exercise therapy complexes.
However, it is often necessary to remove veins in the legs. Prices in our clinic are quite reasonable. You can definitely afford it. In addition, the operation itself is relatively easy for the patient.
Physical therapy after phlebectomy – only with our specialists!
Our clinic does not leave patients immediately after surgery. We provide physical therapy after phlebectomy, which helps you quickly get in shape and return to normal life.
The best exercise therapy specialists will work with you. They will select a set of exercises specifically for you. They will also always be ready to help the patient, tell him how to behave in a given situation, and how best to restore health to his legs.
By listening to them, you can quickly return to your usual rhythm of life. You can continue to enjoy every minute - because now you will have absolutely healthy legs! Our specialists will do everything to achieve this goal! Contact us to make sure of this!
Carrying out the operation
The operation can be performed under the following types of anesthesia:
- Intravenous anesthesia,
- In some cases, general anesthesia is used.
The specific technique of the operation itself should be determined by an orthopedic surgeon, who makes decisions based on diagnostic data, x-rays and MRI results. Most often, the choice of technique is determined by the degree of joint damage.
When performing arthroscopy, two punctures measuring 4-5 mm are made. The first puncture is necessary to insert an arthroscopic camera, which records all changes and condition in the joint. The image is transmitted to the monitor, and the doctor can accurately know the internal condition of the joint capsule and effectively carry out treatment. A second puncture is necessary to insert the instrument
Indications for surgery:
Shoulder arthroscopy is performed in the following cases:
- For instability of the shoulder joint.
- If the patient has a diagnosis of “Habitual shoulder dislocation.”
- If the rotator cuff is damaged.
- Impingement syndrome
- Injury to the biceps tendon.
- Arthrosis.
For the knee joint the list is somewhat smaller and includes mainly traumatic injuries:
- Meniscus damage
- Injury to the anterior and posterior cruciate ligaments.
- “Habitual dislocation” of the knee joint or patella.
- Deforming arthrosis of the knee joint.
Contraindications:
- The presence of allergic rashes, purulent wounds, fibrous lesions in the operation area,
- Fresh injury to the periarticular area.
- It is prohibited to perform arthroscopy on people who have malignant neoplasms in the body. In this case, it is recommended to first undergo full treatment (radiation therapy and chemotherapy), and then allow the body to recover.
In some cases, even if there are any local problems or allergic reactions, it is possible, together with the doctor, to select a method of arthroscopy that will have minimal consequences for the patient.
Consequences and prognosis
Minimal punctures after arthroscopy usually disappear within 3-4 weeks after surgery. This is very small compared to scars from full-scale operations: the marks remain with the patient for life or for many years.
Immediately after the intervention, the patient will feel some discomfort; it is advisable to completely eliminate any stress on the operated joint. If arthroscopy was performed on the leg joints, the patient is advised to use crutches for 2-4 weeks.
A week or two after the intervention, the person can return to their normal activities. Until this point, it is recommended to reduce the load on the joint to a minimum, and also to follow the doctor’s recommendations for restoring the body after surgery.
The prognosis is favorable. Almost all patients, with the help of this operation, got rid of their joint problems, successfully recovered and returned to their normal lives. No significant negative reactions were recorded. If the intervention is performed correctly, the patient does not have to worry about the result.
Phlebectomy: an operation that helps cope with varicose veins!
Phlebectomy is an operation prescribed when less radical methods of treating varicose veins have exhausted themselves. They can no longer prevent further development of the disease. In such situations, the risk of life-threatening complications such as thrombosis or trophic ulcers increases.
The stronger the changes, the more difficult it is to cope with them. In such a situation, the operation cannot be postponed. Phlebectomy involves surgical removal of a section of a vein damaged by disease. Thus, blood flow is normalized. Since only the saphenous veins, which carry only one tenth of the total blood volume, are removed, this procedure is generally safe for the circulatory system.
How is phlebectomy of the lower extremities performed?
Phlebectomy of the lower extremities is performed using specific probes. A blood vessel damaged by varicose veins is ligated and crossed at the point where it flows into a deep vein. A guide probe is then inserted into the vessel through the incisions, and this section is then pulled out.
All work is carried out through miniature incisions followed by cosmetic stitches. Traces after the operation thus remain almost invisible. Sometimes stitches are not applied at all, the edges of the incisions are glued together with special strips of adhesive.
Recovery
Complete rehabilitation occurs 4-5 weeks after surgery.
Since in the case of arthroscopy, tissue damage is minimal, the rehabilitation period is short.
As a rule, after the intervention, a person is allowed to get out of bed on the second day. Movement during the period of hospitalization is not prohibited. Already on the 2nd day, the patient can be discharged and continue recovery at home. The doctor gives each patient a list of necessary procedures that speed up healing and develop the joint.
On days 7-12, the doctor examines the healing site and removes the sutures. After 2-3 weeks a person can already put on his usual shoes
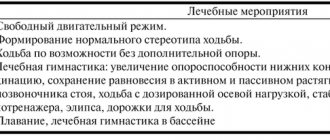
When carrying out rehabilitation, the following methods are used to accelerate healing and restore the functionality of joints:
- Physiotherapy. Exercises aimed at developing the operated joint. A set of exercises is selected individually by an orthopedic surgeon.
- Careful hygiene, especially if the operation is performed on the joint of the lower extremities. The rate of healing of postoperative sutures directly depends on maintaining cleanliness.
- Wearing special orthopedic shoes with soft insoles. In some cases (if the operation was performed to eliminate valgus bursitis), structures are used to separate the toes or additional devices that hold the operated area in its natural position.
- Physiotherapeutic procedures: massage, magnetic therapy, laser therapy. Physiotherapy is prescribed by a physiotherapist and only after a personal examination of the patient.
Arthroscopy does not require long-term wearing of correction devices. Most rehabilitation techniques can be used at home by the patient after consultation with the attending physician.
Memo to the patient during coronary artery bypass surgery
We consider it necessary, before coronary bypass surgery, to present you with an abbreviated version of the manual for a patient who is about to undergo coronary bypass surgery. It gives very important advice on many issues regarding your upcoming operation.
The manual briefly presents tips and tricks, the use of which will provide you with a calmer and more effective passage of the postoperative period, and will help you avoid many mistakes and incorrect actions that are fraught with complications. You will also need this manual later after the operation to improve the long-term results of the operation.
With wishes for a speedy recovery!
To train the respiratory muscles, along with the use of breathing exercises, various breathing simulators can be used, as well as improvised means, such as a tube, a balloon, a rubber bladder.
When using them, it is recommended to blow into a tube, inhale as deeply as possible, and exhale as long as possible, timing the exhalation time. During subsequent exercises, try to increase the exhalation time. In addition, breathing through a tube can be done in the following way: inhale in 3-4 small breaths, as if in portions, and exhale calmly evenly; or inhale evenly and deeply, and exhale in portions into a tube.
When using special simulators, you should consult with your doctor about the possibility of use, and if approved, follow the instructions included with this simulator.
One of the very important points in the preoperative period is the acquisition of abdominal breathing skills , which you will need in the early postoperative period for easier full breathing, improved gas exchange and good discharge of sputum from the lungs:
- I.p. – lying on the bed or sitting on a chair, one hand lies on the stomach, the other on the chest, the body is relaxed: take a calm breath through the nose, inflating the stomach, while the hand lying on the stomach rises, and the second one, on the chest, remains motionless .
- The duration of inhalation is 2–3 s. When you exhale through a half-open mouth, the stomach drops. The duration of exhalation is 4–5 s.
- After exhaling, there is no need to rush to inhale again, but should pause for about 3 seconds until the first desire to inhale appears.
- During one lesson, you need to perform from 5 to 10 repetitions, at least 4-5 approaches (times) per day. If you are a smoker, it is very important to stop smoking as soon as possible before surgery. Every day and even an hour before anesthesia that you spend without a cigarette will reduce the likelihood of lung problems that arise after surgery. Quitting smoking will significantly improve the long-term results of the operation: coronary bypass grafts formed during the operation will work for many years and will relieve you of heart pain and other problems with your health. Remember that if you continue to smoke, you may significantly reduce the effectiveness of your surgery.
If your operation is scheduled for the next morning, you will not be allowed to drink or eat after 20:00, if in the afternoon, you will be allowed to eat some liquid food early on the morning of the operation. On the day of surgery, be sure to take all medications prescribed by your doctor and drink them with the minimum required amount of water.
Another serious complication in the postoperative period is suppuration of the postoperative wound. To prevent this complication, you need to wash with soap in the evening (it reduces the number of bacteria on the skin, thereby reducing the risk of infection).
It is necessary to remove hair on the day of surgery from where the incisions are planned (from the chest, from the legs from the feet to the groin and from the groin area), using electrolysis or using depilatories. When using depilatories, to avoid an allergic reaction, apply a small amount of cream to the inside of the forearm the night before; if there is no redness (allergic reaction), you can apply it to the desired area. Avoid shaving the skin in the area of surgery, as shaving causes microdamage to the skin and the possible formation of pustules - micropustules, which is a very good environment for the development of bacteria.
Before the operation, you will definitely need to ensure that you have a postoperative bandage (corset) for the chest and, possibly, elastic bandages for bandaging the legs. The corset (bandage) is designed to prevent the divergence of the two halves of the cut sternum, and elastic bandages are designed to cover the wound of the leg after taking your vein from it, which will serve you to supply blood from the aorta to the muscle of your heart. Place the corset and elastic bandages in your personal belongings so that you can easily get them out and start using them as soon as you are transferred from the intensive care unit to the recovery room.
Before the operation begins, doctors will connect special tubes (catheters) to you. This is necessary to continuously monitor your vital signs during and immediately after surgery. Catheters are inserted into arteries and veins after you fall asleep.
After operation. When you wake up after surgery, you will find a breathing tube in your mouth connected to a respirator. Under no circumstances should you grab it or try to pull it out. A respirator will help you breathe until you can do it on your own. Once the breathing tube is removed, you will be able to breathe deeply and
cough to remove mucus from the lungs.
There is no need to be afraid of coughing; thanks to it, accumulated phlegm is removed from the lungs. But for normal healing of a postoperative wound, it is necessary to protect the sternum and shoulder girdle from excessive stress. Therefore, you need to cough correctly. Remember that when coughing, the post-operative bandage (corset) must be properly fastened to your chest.
When coughing, you need to clasp your shoulders with your hands and fix your chest, and perform coughing movements using your abdominal muscles, trying to keep your chest motionless. This is where belly breathing comes in handy. To properly support the chest when coughing, it is convenient to use a pillow, pressing it tightly to the chest, as if hugging it.
If there is no means at hand, you can fix the chest with your palms.
How to stand up correctly. After surgery, the process of getting out of bed is the most difficult and difficult for the body. Even walking during this period is an easier process. Therefore, you need to get up for the first time with the help of medical personnel. Remember that stress on the shoulder girdle when standing is unacceptable, as it may have a negative effect on the healing of the sternum. If you lean on your hands or pull yourself up with your hands when standing up, the sutures on the sternum may become loose, which can lead to a serious complication, i.e. divergence of the sternum.
Before getting up, do not forget to fasten your corset and follow certain rules. When rising, you need to roll onto your side and then lower your legs from the bed, using your upper torso and arms to try to sit up.
Don’t rush to get to your feet right away; first, try pressing your feet on the floor one at a time, as when walking, and only then get up. You cannot lean on your back with two elbows, turn on your side without lowering your legs to the floor.
How to walk correctly. After you gain confidence in your legs, and this happens quickly, you need to walk, but little by little, much less than before the operation. On the 1st day after surgery, it is better to only walk around the room.
If your condition is more stable the next day and you are able to sit up in a chair, you can walk around the room for a short distance. You will be transferred to an inpatient ward, where you will continue to be monitored.
In the inpatient department. In the department, your activity will increase every day. On the 1st day after transfer from the intensive care unit, it is better to walk around the ward. The next day you can go out into the corridor. Your task is to walk little by little, without any unpleasant sensations in the chest. For some this distance will be 5 m, for others it will be 50 m, but at one time it should not exceed 150 m. During the day you can walk from 1 to 15 times. Focus on your well-being. You should continue to do breathing exercises and belly breathing to stimulate coughing. Remember to keep a pillow nearby and use it when you cough. You need to continue the exercises you started in the intensive care unit for your arms, legs and chest.
Getting up from a chair: move to the edge of the chair, place your feet under you, try to stand up using your leg muscles.
Sitting: Sit up straight with both feet on the floor. Your knees should be level with your hips. Don't cross your legs.
Lifting objects from the floor: without bending at the waist, bend your knees, lowering your body vertically; your back should remain straight.
In order to prevent sternum divergence in the first 2–3 months, it is not recommended:
- in a lying position, place your hands behind your head;
- spread your arms in different directions;
- move your hands behind your back (in different positions);
- cross your arms in front of you;
- raise both arms up;
- perform exercises with both hands;
- move around the bed, leaning with both hands;
- in a lying position, raise your legs up;
- in a lying position, perform the “bicycle” exercise;
- bend the body forward, sideways, backward, and rotate the body;
- sleep on your stomach or side;
- pull up;
- perform push-ups (even from the railing).
Tips for breast corset:
- The corset is worn over underwear made of cotton fabric and does not irritate the postoperative seam. It is strictly not recommended to wear it on a naked body!
- The corset should be worn while lying on your back.
- The postoperative corset is worn around the clock for up to 3 months after surgery.
- A break from wearing a corset is a must. Unfasten the Velcro or hooks periodically for 15–20 minutes. Making sudden movements at such moments is strictly prohibited!
- Remember that the corset must be fastened tightly enough to keep the breastbone stationary and heal well. Take as deep a breath as possible, then fasten the corset tightly.