Preparing for surgery
During the consultation, a specialist (neurologist, vertebrologist-orthopedist) will question the patient in detail, conduct a medical examination, and prescribe the necessary examination.
All preoperative examination and preparation can also be completed quickly and in comfortable conditions in our hospital using high-precision digital tomographs (MSCT 128 slices; MRI 1.5 Tesla), an X-ray system made by Philips. In our radiology department, we can take an image of the entire length of the spine, which is rare even for Moscow, which is sometimes necessary when planning orthopedic operations.
Based on the results of the examination, doctors at the Yauza Clinical Hospital will quickly and accurately determine the cause of back pain, make a clinical diagnosis and determine the optimal treatment method. If necessary, the patient will undergo minimally invasive surgery, which will relieve him of pain for a long time.
Before the operation it is also necessary to undergo a standard examination:
- X-ray of the chest organs
- Tests for hepatitis C and B, syphilis, HIV
- General blood and urine tests
- Determination of blood group and Rh factor
- Detailed biochemical blood test with electrolytes and coagulogram
- ECG
- Consultation with a therapist
TREATMENT OF DIAPHRAGMAL HERNIA
Who needs surgical treatment for hiatal hernia? Elimination of a hiatal hernia is necessary for patients with a paraesophageal (paraesophageal) hernia due to the risk of strangulation, regardless of the severity of existing symptoms, as well as for patients with a sliding hiatal hernia, which has pronounced clinical manifestations in the form of heartburn, regurgitation (regurgitation) of food and requiring constant drug treatment.
Patients with extraesophageal symptoms of a diaphragmatic hernia (recurrences of pneumonia and bronchitis, night cough, chronic laryngitis), Barrett's metaplasia, side effects from therapy with acid-lowering drugs are also candidates for surgical treatment.
Figure - Main types of hiatal hernia
Progress and advantages of surgery for endoscopic removal of intervertebral hernia
- The operation is performed under epidural anesthesia and lasts approximately one hour. The patient remains conscious and can be contacted, but does not feel pain. To maintain calm before surgery, the patient is often given sedative (calming) medications. For comparison, surgical interventions performed using the traditional open approach can last up to 6 hours and are performed under general anesthesia.
- The incision in the skin usually does not exceed 1 cm and is more like a puncture through which a special thin spinal endoscope is inserted. The device is equipped with light guides and a miniature video camera, which provides the surgeon with the opportunity to visually control all his actions; the image is displayed on the monitor.
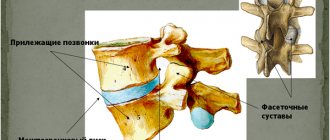
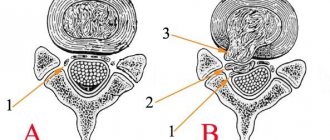
- If the localization of the hernia allows, then its removal is carried out through the natural foraminal opening, where the spinal nerve root exits the spine (transforaminal approach). This is the most gentle surgical technology performed through a puncture.
- When the endoscope penetrates, the tissues are not cut, but are moved apart using special manipulators, which allows them to be kept practically intact.
- The surgeon can quickly stop the bleeding thanks to a coagulator and thermal effects on the tissue.
- The doctor removes the sequestrum - a hernial protrusion, as well as damaged fragments of the intervertebral disc, restores the integrity of the fibrous ring between the vertebrae, which prevents recurrence of the hernia.
Indications for the procedure
This formation (from 1 to 1.5 cm in size) is a common pathology that arises against the background of progressive chronic osteochondrosis. It develops when the fibrous ring around the intervertebral disc ruptures, which leads to prolapse of its nucleus into the spinal canal. As a result of this, irritation of the nerve endings occurs, and when the protrusion reaches 5-7 mm, compression of the roots occurs, which leads to severe pain.
Indications for surgical treatment may be:
- Severe pain lasting at least 6 months
- Muscle atrophy and paralysis.
- Lack of the desired result from conservative therapy, which was carried out for 3-4 months (provided that medical prescriptions are followed regularly and correctly).
- Radicular syndrome.
- Disorder of the functioning of the pelvic organs (intestines, genitourinary tract).
- Spinal stenosis.
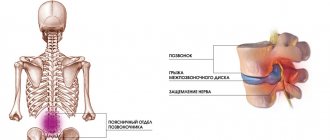
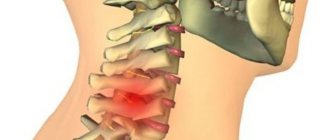
- Poor cerebral circulation (if localized in the cervical region), caused by compression of the arteries of the neck.
Modern equipment
The operation is carried out using special equipment from the world's leading manufacturers of medical equipment, such as DePuySynthes, Karl Storz, Joimax and others.
Radiation diagnostics at the stage of surgery planning, intraoperative visual control, and evaluation of treatment effectiveness are carried out using Philips expert systems, which show a detailed picture of the condition of the spine and surrounding tissues.
The results of spinal surgeries performed by our spinal surgeons were highly appreciated by colleagues from the USA, Germany, specialized orthopedic centers in Russia, as well as numerous grateful patients who were saved from pain, regained mobility and a decent quality of life.
Rehabilitation
The recovery period lasts from 1 to 3 days. Rehabilitation measures are carried out in a hospital, under the close supervision of the attending physician (monitoring continues for 1-2 weeks). In the first 5-10 days, the patient will need to regularly take antibiotics, NSAIDs and counter-current medications. For the first month, you must wear a rigid orthopedic corset and minimize physical activity. If the operation was performed on the lumbar region, then strong flexion and extension of the back must be prevented. Sports and exercise therapy are allowed only after 2 months.
Why us
- Doctors. The Department of Neurosurgery employs spinal surgeons with extensive experience in the successful treatment of intervertebral hernia. At the Yauza Clinical Hospital you can be advised by well-known specialists from Germany, Israel and other countries.
- Expert equipment. The Yauza Clinical Hospital is equipped with equipment from the world's leading manufacturers; operations are carried out using modern equipment from Karl Storz, DePuySynthes, and Joimax.
- Innovative design of operating rooms. Infection-resistant seamless monolithic blocks, 5 levels of sterility thanks to a sophisticated ventilation system.
- Fast recovery. The patient can return home the next day after the operation. Complete recovery occurs much faster compared to traditional hernia removal.
- Low morbidity . There are no noticeable postoperative scars - operations are performed endoscopically through small incisions.
- Safety. Minimal risks of developing postoperative complications. There is no harmful effect of anesthesia on the patient.
You can make an appointment with specialists at the Center for Vertebrology and Endoscopic Spine Surgery at the Yauza Clinical Hospital using a special form on the website or by calling the phone number indicated on this page.
You can see prices for services
The article was checked by an orthopedist-vertebrologist, MD. Abakirov M.D. , is for general informational purposes only and does not replace specialist advice. For recommendations on diagnosis and treatment, consultation with a doctor is necessary.
Establishing diagnosis
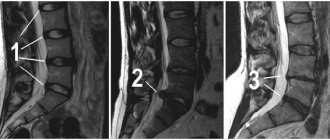
Diagnosis of intervertebral hernia is of key importance for choosing a treatment regimen and is carried out using the following methods:
- MRI of the spine. “Gold standard” for identifying pathological changes in muscles, ligaments and nerve structures.
- CT scan of the spine. Allows you to assess the condition of bones and soft tissues.
Ultrasound for intervertebral hernias is not the main way to diagnose spinal diseases. X-rays are prescribed only to determine the traumatic or non-traumatic nature of existing disorders.
Complications
But even with successful manipulations, in some patients (approximately 25%) the radicular syndrome remains or recurs after some time, and neurological and movement disorders persist or arise. A clinical examination of patients who fell into the group of people with unsatisfactory results found that the causes of unsuccessfully operated spine syndrome are mostly:
- recurrence of hernia formation at the same level (8%);
- narrowing of the spinal canal due to exostoses and arthrosis of the intervertebral joints (4.5%);
- the appearance of a hernia on a disc adjacent to the operated segment (3.5%);
- formation of pathological scars and adhesions in the spinal canal (3%);
- scar-adhesive formations in the nerve roots (3%)
- postoperative pseudomeningocele and spinal-epidural hematomas (1%).
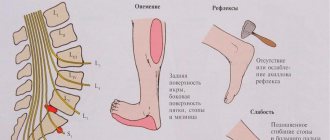
Areas where pain may be felt.
As can be seen, relapses of the disease in the same place where the hernial tissue was resected are of particular concern. And quite often this is a consequence of mistakes and inaccuracies made during the rehabilitation period, ignoring in the long term the requirements and restrictions regarding everyday lifestyle.
Those who, after high-quality rehabilitation, continue to recover in a sanatorium are less likely to face the consequences than others. Therefore, this fact should be taken into account by all patients, since consolidation of the achieved functional results immediately after the end of the main rehabilitation program plays a far from secondary role.
What may be the intraoperative consequences? Mostly they are associated with injury to the nerve or dura mater of the spinal cord.
- The first complication will be manifested by pain and loss of sensitivity in the legs or arms, depending on the location of the injured nerve. If the nerve structure is severely damaged, the prognosis for its recovery is, unfortunately, disappointing.
- If the dura spinal membrane is damaged, if the surgeon detects the defect in a timely manner, he will suture it. Otherwise, cerebrospinal fluid will leak. Impaired circulation of cerebrospinal fluid will cause problems with intracranial pressure and, as a result, the patient will experience severe headaches. The dura can heal on its own in about 2 weeks.
Negative reactions can be postoperative, early and late:
- Early complications include purulent-septic processes, including epiduritis, osteomyelitis, suppuration of the suture, and pneumonia. In addition, the group of early postoperative consequences includes deep vein thrombosis of the lower extremities and pulmonary embolism.
- Late negative reactions are repeated relapses, secondary degenerative pathologies. This also includes rough scar-adhesive growths, which in turn compress nerve formations, which, as with intervertebral hernias, is manifested by pain and/or paresthesia spreading along the pinched nerve.
If the operation was carried out at an exemplary level, all preventive measures were followed and medical recommendations were flawlessly followed, the likelihood of any consequences occurring is reduced to the very minimum.