Among the various variants of the course of complicated osteochondrosis, there is the most dangerous one. This is a sequestered hernia of the spine. How does intervertebral disc sequestration occur and for what reasons does it develop? Is it possible to be cured radically without surgery, or does the condition require only radical treatment? But before answering these questions, a definition should be given: what is sequestration of the intervertebral disc?
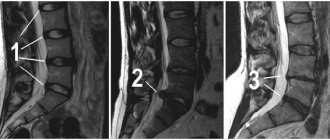
Sequester in the image on the right.
What is a sequestered hernia
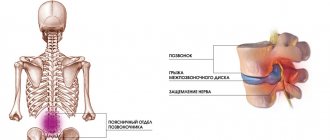
Sequestrum is a separated and necrotic part of tissue located among living tissues. A hernia is called sequestered, in which part of the nucleus pulposus is separated from its main mass.
The mechanism of pathology formation is as follows. First, the integrity of the fibrous ring is disrupted. A part of the nucleus pulposus (which is a hernia) emerges into the resulting defect. With great or too sudden physical activity, this part is separated from the main mass of the disc and moves up or down.
With a sequestered hernia, part of the intervertebral disc becomes separated from its main mass. It is located freely in the spinal canal, where it can touch the nerve roots. It is this effect on the spinal roots that poses the main threat.
What contributes to the formation of sequestration, and who is at risk?
In order for a sequestration hernia of the spine to form, two conditions are necessary: the presence of a normal vertebral hernia and a sharp traumatic effect, leading to the separation of the protruding part from the total mass of the nucleus pulposus. It can also appear in people with a healthy spine as a result of severe trauma, in which fragments of cartilage tissue and bones act as sequesters. Most often, a sequestering hernia appears when:
- falling on ice in icy conditions;
- sudden lifting of heavy loads;
- sudden movements of the spine: bending, twisting;
- inflammation of the vertebrae: discitis, spondylitis;
- advanced osteoporosis.
People who lead a sedentary lifestyle with rare periods of excessive physical activity are most susceptible to this disease. Physical inactivity weakens the structures of the vertebrae, as a result of which they cannot withstand a sharp increase in loads during periods of excessive activity.
Reasons for development
The etiology of this disease is not precisely known. There are several predisposing factors for the development of sequestered hernia:
- osteochondrosis;
- congenital pathology of the spine;
- spinal injuries.
People facing at least one of the listed factors are at risk. Under certain circumstances, they may experience a herniated disc. Such circumstances may include physical activity, heavy lifting, or falling from one’s own height. The more pronounced the predisposing factor was, the greater the chance of the formation of a sequestration of the intervertebral disc.
Additional factors play a role in the development of disc herniation. These include excess weight, a sedentary lifestyle, and poor posture. By themselves, they cannot lead to the disease, but they increase the chances of its occurrence. Thus, overweight people are more likely to develop degenerative spinal diseases. With a sedentary lifestyle, the ligamentous apparatus of the spine suffers, which also predisposes to the occurrence of the disease. With scoliosis or kyphosis, the problem most often occurs in places where the spinal column is curvature.
What is the danger
Destruction of the intervertebral disc goes unnoticed for a long time. The disc is not innervated and has no blood supply in adults. If the sequester does not affect any structures of the spinal cord, it does not pose a danger. The main problem is that there is no free space in the spinal canal. One way or another, some brain structures remain compressed by part of the disc.
The sequester can put pressure on the nerve roots. This stops the transmission of impulses along the nerve fibers. This leads to disruption of the functioning of those organs and parts of the body that were innervated by these fibers. This can cause paresis or even paralysis of the upper or lower limbs.
A sequestered cervical hernia can lead to compression of the vertebral arteries. These arteries supply brain tissue. Poor blood supply to the brain leads to headaches and fainting. Squestered hernias of the lumbosacral region are especially dangerous. They can cause the so-called “cauda equina syndrome”. In this case, the fibers innervating the lower limbs, pelvic organs, and perineum are affected.
Stages of development of a sequestered hernia
In severe cases, a sequestered hernia leads not only to paresis of the lower extremities, but also to disruption of the functioning of the pelvic organs. Urinary retention caused by compression of the cauda equina provokes the development of an infectious process in the bladder. Its complication can be pyelonephritis, an infection of the renal pelvis.
Constipation due to impaired innervation leads to intestinal obstruction and intoxication. The reverse process - urinary and fecal incontinence - is also possible with the described pathology. This significantly complicates social functioning and leads to disability.
Localization of sequestered hernia
A sequestered hernia of the spine can be observed in any of its parts. Accordingly, hernias of the cervical, lumbar, sacral and thoracic regions are distinguished.
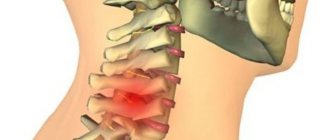
Sequestrated cervical hernia
It often occurs between the fifth and sixth (C5-C6) or sixth and seventh (C6-C7) cervical vertebrae. It can develop in case of osteochondrosis or cervical injury. With osteochondrosis, the pathology occurs gradually, with injury - more acutely. In the cervical region there are small vertebrae and their openings; accordingly, there is a narrow spinal canal. A protrusion in this section can compress the spinal cord, disrupting the efferent innervation of all organs and parts of the body. Compression of the vertebral artery, which also lies close to the vertebral bodies, leads to disruption of the blood supply to the brain.
Want to learn more about the symptoms and treatment of a cervical hernia? Read our article.
Each type of intervertebral hernia has serious complications, so you should not delay treatment.
See how easy it is to get rid of a hernia in 10 sessions
Sequestrated lumbar hernia
In 75% of cases it occurs between the fourth and fifth lumbar vertebrae (L4-L5). Develops due to degenerative changes in this area. Triggering factors can include physical exercise, especially heavy lifting, as well as injury. At this level, damage to both efferent and afferent nerve fibers going to the lower extremities is possible. The result is sensory or motor dysfunction of the right or left leg.
Read all about lumbar hernias in this article.
Sacral sequestered hernia (l5 s1)
Occurs between the fifth (last) lumbar vertebra and the sacrum. It is also a consequence of osteochondrosis and excessive or sudden physical exertion. A sequestered hernia l5 s1 can affect the cauda equina, leading to damage to its fibers. This entails not only impaired sensitivity or movement in the lower extremities, but also dysfunction of urination and defecation. Erectile dysfunction is also possible in men.
Sacral sequestered hernia affects the l5 s1 vertebrae and can cause sensory impairment in the lower extremities
Sequestrated thoracic hernia
In this department, problems can occur with equal frequency between any vertebrae. This is a rare pathology. It is observed in people with spinal curvature (kyphosis), as well as with severe injuries and playing contact sports. Compression of the spinal cord at the level of the thoracic spine leads to disruption of the innervation of the legs, as well as difficulty in respiratory function. Disease in this department is more difficult to diagnose, since it often imitates symptoms of diseases of other organs and tissues (heart, pleura, stomach, muscular frame of the chest).
More information about thoracic hernias here.
Peculiarities
The L5–S1 intervertebral disc is located between the last lumbar vertebra and the sacrum. This is the largest disc in the spine, the diameter of which significantly exceeds the height. But due to the high load placed on him, he more often than others suffers from the development of osteochondrosis, then protrusion and, ultimately, a hernia.
But if previously such changes were mainly observed in older people, today intervertebral hernias have become much younger and are increasingly occurring even in young people. The main reason for their formation is advanced osteochondrosis. Create the prerequisites for its development:
- sedentary lifestyle, sedentary work;
- overweight;
- regular performance of heavy physical labor;
- back injuries;
- spinal deformities in any plane;
- genetic predisposition.
Thus, under the influence of these factors, degenerative-dystrophic changes begin in the tissues of the L5–S1 intervertebral disc. Initially they affect the inner part of the disc - the nucleus pulposus. Tears gradually form in its fibers, which leads to an uneven distribution of pressure on the surrounding fibrous membrane. Under the influence of the shifting nucleus pulposus and pressure from the vertebrae, it experiences serious overloads, as a result of which the fibers of the fibrous ring also begin to gradually stretch and tear in the place where their strength is minimal as a result of injury or other factors.
Thus, the symmetry of the intervertebral disc is disrupted. At a certain point there is a slight protrusion of the nucleus pulposus and the entire disc beyond the vertebral body. But since the nucleus pulposus still remains within the annulus fibrosus, in such situations L5–S1 disc protrusion is diagnosed.
The shock-absorbing properties of the disc begin to decline immediately after the first changes occur in it. Even a slight protrusion can lead to disturbances in the patient’s well-being and pain syndrome.
If no action is taken at this stage, the deformity will worsen, since the pressure of the vertebrae on the disc does not disappear, and the fibers of the fibrous membrane continue to be subject to constant pressure. As a result, it cannot withstand and ruptures, against which prolapse and herniation of the L5-S1 disc are diagnosed.
Thus, a passage is formed in the fibrous ring, through which the nucleus pulposus is able to get out, that is, into the spinal canal. This is what leads to the development of acute neurological symptoms characteristic of a hernia, since a mass of nerve endings from the cauda equina pass through the spinal canal. Therefore, the appearance of even a small foreign body in it leads to their infringement and the occurrence of corresponding disturbances in the functioning of those organs for the innervation of which they are responsible.
Therefore, with a hernia of the L5–S1 spine, severe pain is observed not only in the lower back, but also in the legs, feet, toes, sacrum, buttocks, etc. There is also a violation of their sensitivity, extinction of reflexes and other changes. Moreover, the nature of the clinical picture largely depends on the type of hernia.
Types of sequestered hernia
Sequestered spinal hernias are divided into types in relation to the plane of the spinal column. Thus, they distinguish:
- dorsal (posterior)
– protrude into the lumen of the spinal canal, are most common, are subject to conservative and surgical treatment; - median
- rarely found, mainly between the lumbar and sacral vertebrae, causing concern only in case of intense increase in size; - paramedian
- in this case, the hernia protrudes in the projection of the nerve root and touches it, they are the most painful and quickly lead to complications.
Detailed qualifications in our article “Types of spinal hernias”.
Is it possible to avoid the formation of a hernia?
A hernia develops as a consequence of those degenerative processes that only increase with age. By influencing risk factors, you can reduce the likelihood of its formation.
- If you have a sedentary lifestyle or sit for long periods of time at work, you must remember to take breaks and warm up;
- engage in low-intensity physical activity, join a swimming pool;
- if you are overweight, you should work towards reducing it;
- do not lift heavy loads or do it technically, using the abdominal muscles and lower extremities;
- if an injury occurs, you must consult an osteopath as soon as possible;
- When working at a computer, it is recommended to follow the principles of ergonomics that we teach our patients.
Treatment of sequestered spinal hernia should begin immediately after diagnosis. But if you don’t think about changing your lifestyle and habits, it won’t be as effective; risk factors will continue to affect the spinal structures.
Treatment of a disc herniation should act on the causes and mechanisms of its development, be timely and comprehensive.
The use of osteopathic treatment restores the normal position and movement of the spine and body as a whole, speeds up recovery, and reduces the risk of relapse.
Did you like the article? Add the site to your browser bookmarks
Symptoms of a sequestered hernia
The manifestations of this disease largely depend on in which part of the spinal column the sequester is located. The leading pain syndrome in all situations will be pain, but its intensity and localization may vary.
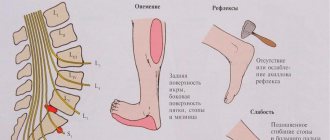
Symptoms of sequestered lumbar hernia and l5 s1 hernia
The pain is localized in the lumbar spine. It can vary in intensity. In mild cases, pain occurs when performing certain movements. In severe cases, the pain from a spinal hernia is constant and decreases only in one body position. In this case, the patient constantly strives to take the position in which the pain is minimal.
Pain sensations can be localized along the sciatic nerve. In this case, the buttock, the back of the thigh, the lower leg, and sometimes the foot hurt. In addition to pain, sometimes there is a decrease in the sensitivity of the lower limb, and in the most severe cases, a violation of motor functions. Some patients cannot step on their heels and walk on their toes. In rare cases, disorders of the pelvic organs are observed.
Symptoms of sequestered hernia of the thoracic and cervical spine
Cervical hernias are most often accompanied by pain in the neck, scapular region and upper extremities. Sensory disturbances occur on the skin of the upper extremities. In some patients, the pathology is manifested by motor disorders, for example, transient or permanent paresis of one or more fingers.
In the most severe situations, the hernia does not affect the nerve roots, but the spinal cord and can disrupt the innervation of any organs and parts of the body. It is also possible that cerebral circulation may be impaired due to compression of the vertebral arteries.
In the thoracic region, hernias are most often accompanied only by pain. In this case, pain can be located not only in the back, but also radiate throughout the chest. So they imitate intercostal neuralgia, myocardial infarction, stomach ulcers and other diseases.
Thoracic and cervical regions
These sections were united, because the spinal cord passes through them in the central canal of the spine. We will not dwell in detail on the typical symptoms of osteochondrosis, which indicate the existence of a disc herniation. These are, for example, symptoms such as:
- pain in the neck or chest, which radiates to the arm or shoulder, girdle pain like intercostal neuralgia;
- diffuse sensitivity disorder, numbness, tingling in the neck,
- weakness in the neck, arm muscles, hands or fingers;
- autonomic disorders associated with changes in blood pressure, coldness and redness of the skin, changes in skin temperature.
In addition to the above symptoms, it is necessary to list the dangerous signs of spinal cord damage. They should be regarded as a complicated course of a sequestered hernia in the cervical and thoracic spine, and require immediate hospitalization in a neurosurgical hospital on the board, with transportation according to the rules of a probable spinal fracture. These symptoms include:
- progressive weakening of pain and temperature sensitivity on one half of the body, which indicates compression of the lateral column of the spinal cord;
- the presence of severe weakness in the legs, or even at the level of the body on one side, and on the other side - loss of pain and temperature sensitivity, which indicates transverse myelitis, or compression, pronounced swelling of half the diameter of the spinal cord;
- The most dangerous symptom is compression of the entire diameter of the spinal cord by sequestration (hematoma, edema, complete transverse myelitis). In this case, the patient will have a complete absence of all types of sensitivity downward from the localization of the sequestrum, and at the same time central paralysis and the presence of central type urinary disorders will be observed.
In the event that we are talking about a thoracic or lower thoracic lesion, then this will be paralysis in the legs. If we talk about the most unfavorable localization of a complicated sequestration in the area of the upper cervical thickening, then we will be talking about spastic tetraplegia, that is, complete paralysis of the arms and legs and loss of all types of sensitivity.
Thus, in the event of a sudden development of edema or injury to the structures of the spinal cord, both the thoracic and especially the cervical and upper cervical localization of a sequestered hernia is a “time bomb.” In the event of the development of injury or compression of the spinal cord, a transformation of the usual complaints occurs - the cessation of pain impulses, and the transformation of complaints towards the appearance of loss of sensitivity and the development of paralysis.
Diagnosis of sequestered hernia
This pathology is diagnosed and treated by several specialists. Vertebrologists deal with pathology of the spinal column. Innervation disorders that arise as a result of the development of a hernia are identified by neurologists. Surgical interventions on the spinal cord are performed by neurosurgeons. The best results can be achieved through the coordinated work of all doctors.
Diagnosis begins with a detailed examination of the patient. It allows you to identify the level of damage to the spinal column and the depth of damage. Then they move on to additional diagnostic methods. The gold standard for making a diagnosis is magnetic resonance imaging (MRI).
MRI allows you to visualize in detail each vertebra, intervertebral discs and ligaments of the spinal column. In this way, it is possible to detect a sequester, determine its type and location.
Less informative, but more accessible is CT - computed tomography. It also shows soft tissue, but with a lesser degree of visualization of structures. Another diagnostic method is radiography of the spinal column. It does not show soft tissue, but allows you to assess the integrity of bone structures and their position relative to each other. X-rays are performed in conjunction with MRI or CT.
Laboratory tests will not help make a diagnosis. They are necessary if surgical treatment is chosen. A general and biochemical blood test, a coagulogram and a urine test are the standard list of preoperative preparations.
What types of intervertebral hernias are most difficult to treat?
4 stages of treatment for intervertebral hernia
Treatment of sequestered hernia without surgery
The success of treatment largely depends on the timeliness of diagnosis. The earlier therapy is started, the better the effect. Treatment of a sequestered hernia without surgery is possible in mild cases. Conservative treatment includes drug therapy, treatment with folk remedies, the Bubnovsky method, physiotherapy, massages, exercise therapy. Even for a sequestered lumbar spinal hernia, treatment can begin conservatively.
Drug treatment
Drugs for the treatment of sequestered hernia
With the help of drug therapy it is impossible to remove sequestration, but it is possible to make the course of the disease asymptomatic. For this purpose, the following groups of drugs are used:
- Local analgesics
are used in the form of blockades. To do this, drugs (Novocaine or Lidocaine in combination with glucocorticosteroids) are injected directly into the area of the sequestered disc herniation. This leads to the disappearance of pain. - NSAIDs
– non-steroidal anti-inflammatory drugs (Diclofenac, Ibuprofen, Ketanov, Celecoxib, Nimesulide) are used in the form of tablets or injections to reduce back pain. - Muscle relaxants
- drugs that can relax striated muscles (Sirdalud, Meloxicam) help reduce pain and eliminate the feeling of stiffness in the back. - Chondroprotectors
are medicinal substances (Chondrolone, Chondroflex) that do not affect an already formed hernia, but prevent the development of protrusions in other parts of the spine.
Folk remedies
Doctors do not recommend treating a sequestered hernia exclusively with traditional methods. They can be used in combination with other methods of therapy. The following types of treatment are used in folk medicine:
- applications with anti-inflammatory and analgesic ointments (Capsicam, Fastum gel, Nise)
- they are placed on gauze, applied to the back and secured with an adhesive plaster; - alcohol compresses
- gauze is soaked in alcohol and aloe juice or garlic juice, placed on the sore spot and covered with film, the compress should be kept for 2-3 hours; - a wool belt for the back
- used for protrusions of the lumbar region, prevents increased inflammation.
Bubnovsky method
This treatment method is a type of physical therapy. Dr. Bubnovsky proposed a number of physical exercises according to a special program, which are aimed at the prevention and treatment of spinal diseases.
Bubnovsky’s gymnastics are exercises with your own body weight, as well as exercises on special multifunctional simulators. The technique is relatively new, but its author speaks of good treatment results.
Exercises according to the Bubnovsky program
For a sequestered hernia, Bubnovsky gymnastics are rarely used, since displacement of the sequester can lead to complications. But the method can be used in complex treatment or after surgery.
Physiotherapy
Physiotherapy is one of the main methods of treating spinal diseases. For sequestered hernia, it is used in patients without complications. The following treatment methods are used:
- magnetotherapy - exposure to a constant or alternating low-frequency magnetic field, helps eliminate swelling, muscle spasms and reduce pain, used for severe inflammatory processes;
- acupuncture is a Chinese technique of influencing Qi energy using acupuncture with needles, which improves blood circulation in the spine and eliminates muscle spasms;
- electrophoresis is the movement of medicinal particles using an electric field; electrophoresis with cariprazyme is most often used to treat hernias; it reduces swelling and treats inflammation.
Read more about electrophoresis here.
Exercise therapy
Physical therapy should accompany both conservative therapy and surgical intervention. You need to start it with an instructor. All exercises are performed from a position lying on your stomach or lying on your back. They should be performed slowly and smoothly. Gymnastics may look like this.
From the starting position lying on your back with arms and legs extended:
- raising your arms up, stretching, lowering your arms;
- flexion and extension of the knee alternately between the right and left legs;
- pulling your legs bent at the knees to your chest with your hands.
From the starting position lying on your stomach, arms and legs extended:
- bending the legs at the knee joints, touching the buttocks;
- bending and straightening the legs, moving to the sides;
- abduction of the leg bent at the knee from the body.
Massage and manual therapy
Massage and manual therapy are not indicated for every sequestered hernia. In some cases, pressure, on the contrary, can displace the sequester and lead to complications. Massage should be prescribed by the attending physician, based on the location and size of the hernia.
Massage helps relax the back muscles and reduce pain. In order for it to be beneficial, the softest, most gentle techniques are chosen. At the same time, they try to minimize pressure and friction. Massage is indicated after completion of treatment to avoid relapse.
Technique
The operation has now been brought to perfection. Through the use of modern microsurgical techniques, open surgery is the most effective method of treating disc herniation. This makes it possible to remove hernias of any size, location and, in the vast majority of cases, significantly restores the patient’s quality of life.
The operation is performed under epidural anesthesia.
In the area of the projection of the damaged disc, a longitudinal skin incision 1.5-2 cm long is made. To access the compressed nerve root, the ligamentum flavum is partially removed, and sometimes the edge of the vertebral arches is excised. The paravertebral muscles are not damaged during the operation, but are retracted to the side. After such surgical access is performed, the nerve root, compressed by the disc herniation, becomes accessible for inspection. Next, the surgeon moves the nerve root aside and removes fragments of the prolapsed nucleus pulposus that form a disc herniation, as well as all those fragments from its cavity that can cause a relapse. No materials are used to replace the removed disc tissue. At the end of the operation, layer-by-layer suturing of the surgical wound is performed. Thanks to the use of modern microsurgical technology and the vast experience accumulated by neurosurgeons, the risk of damage to nerve structures during surgery is minimized. Advantages of microsurgical removal of a herniated disc:
- quick and effective relief of acute pain;
- the possibility of simultaneous removal of two hernias at once;
- reduction of hospitalization periods;
- reducing the period of temporary disability;
- gentle nature of the intervention;
- rare occurrence of complications.
Removal of sequestered hernia
With a sequestered hernia it is often necessary to resort to surgical treatment. This is a necessary measure when the sequestration does not resolve on its own.
Indications for surgical treatment
If the sequester has not undergone resorption after a long time, surgery is necessary
Surgical treatment is indicated in the following cases:
- Paresis and paralysis of the upper or lower extremities.
- Fibrillary twitching of the muscles of the legs or arms.
- Dysfunction of the pelvic organs.
- Erectile disfunction.
- Compression of the vertebral artery.
- Hernia more than 10mm in diameter.
- Failure of conservative treatment.
Types of surgical interventions
- Microdiscectomy
is the removal of the entire intervertebral disc. It is carried out using a small incision in the projection of the disc. Removal occurs with small instruments under a microscope. Used when relapse is possible. - Laminectomy
is the removal of part of the intervertebral disc, also occurs through a minimal incision, has fewer complications than discectomy, but recurrence of the hernia is possible. - Prosthetics
– used when the intervertebral disc is completely removed and there is a need to replace it. Replacing a disc with a prosthesis avoids the negative consequences of a discectomy. - Spondylodesis
is the fusion of several vertebral bodies with each other. Helps avoid recurrence of hernia. It is used for excessive mobility of the vertebral bodies and for spinal injuries. It is a complement to the operation to remove sequestration. - Laser removal
is one of the newest treatment methods. Allows for artificial resorption of sequestration without violating the integrity of other tissues. Used in cases where there is no threat of relapse. - Sequestrectomy
, an operation that exclusively involves the removal of sequester, was the most gentle operation before the invention of laser removal.
Rehabilitation after surgery
In the postoperative period, pain may persist, and the likelihood of hernia recurrence is high. To prevent this from happening, you must follow your doctor's recommendations. During this period, physiotherapy is prescribed. For example, electrophoresis with vitamins is actively used, and for severe pain - with novocaine. Physical therapy is also used. A set of exercises under the guidance of an instructor will create a muscular frame that will prevent further displacement of the vertebrae.
After the postoperative wound has healed, you can proceed to swimming. Preference should be given to dosed training in the pool. Sudden movements and heavy lifting should be avoided during this period.
Types of surgical interventions
Typically, surgical intervention for uncomplicated sequestration is a three-stage procedure. First, measures are taken to remove the sequester itself - sequestrectomy, as a source of potential danger. Then the remains of the destroyed intervertebral disc at this level are eliminated, and the third stage is reconstructive plastic surgery. In ideal cases, for example, as in neurosurgical clinics in the Czech Republic and other developed countries of Western Europe, this is prosthetics, that is, replacing the disc with a new one. Modern materials have such good shock-absorbing properties that they can not only successfully compete with the cartilage tissue of healthy young people, but also surpass them in physical and biochemical characteristics.
In domestic clinics, sometimes it is necessary to perform a spinal fusion operation, that is, to fuse two adjacent vertebrae into a single monolith. Quite often, when sequestering a hernia, it is simply impossible to perform traditional surgical interventions, such as microdiscectomy, or laser removal of the hernia due to the significant removal of the sequestration into the cavity of the spinal canal, as well as the massive destruction of cartilage tissue in this segment.
Approach to hernia treatment at the Paramita clinic
The Paramita Clinic has everything necessary to treat patients with sequestered hernia. The clinic employs such specialists as: neurologists, vertebrologists, reflexologists, massage therapists, chiropractors, kinesiotherapists.
Paramita specializes in diseases of the spine. Here they diagnose hernias, as well as all types of conservative treatment, including physiotherapy, acupuncture and massage. The patient can receive the entire range of treatment procedures in one clinic.
We use non-surgical hernia treatment techniques
Read more about our unique technique
An integrated and professional approach is the key to successful treatment. The clinic prefers therapy that combines Western and Eastern techniques. The risk of postoperative complications is often unjustified, therefore surgery should be resorted to only in the most extreme cases.
Prevention and prognosis
Prevention of a sequestered hernia can be called anything that eliminates the factors predisposing to it. It is important to maintain correct posture and avoid excessive stress and lifting heavy objects. To prevent osteochondrosis, preference should be given to moderate but regular physical activity, swimming, and avoid obesity. In old age, it is recommended to take chondroprotectors.
The prognosis depends on the timeliness of its diagnosis. The smaller the hernia, the better the prognosis. If the sequestration affects the roots and leads to complications, the prognosis is less favorable. The longer the complications exist, the longer it will take to recover.
FAQ
How to relieve pain with a sequestered hernia?
Novocaine and lidocaine blockades fight pain most effectively. They are performed only in medical conditions. At home, you should use an NSAID, for example, diclofenac. The drug is available in tablets, ampoules for intramuscular injections and ointments.
Is there a chance to cure a sequestered hernia without surgery?
Cure means getting rid of sequestration. There are cases when independent resorption (resorption) of sequestration occurs. That is why the disease is treated conservatively at first. If the hernia is complicated, it is impossible to wait or the sequester has not undergone resorption after a long time, surgery is necessary.
How long does the recovery period take after surgery?
The rehabilitation period ends when the patient ceases to be bothered by any symptoms. With a favorable outcome, the rehabilitation period ranges from 4 to 6 weeks.
Bibliography:
- Bersenev V. Spine and pain.
- Rodionova O. Health of the back and spine: Encyclopedia
- Krotenkov P.V., MRI tomography in the diagnosis and treatment of herniated thoracic intervertebral discs. (Russian) Bulletin of radiology and radiology.
- Kaplan L. Lumbar disc herniation. Per. from English N. D. Firsova.
- Tkachev A.M., Epifanov A.V., Akarachkova E.S. “Patophysiological aspects of resorption of intervertebral disc herniations,” Consilium Medicum.
Themes
Intervertebral hernia, Spine, Pain, Treatment without surgery Date of publication: 10/22/2020 Date of update: 12/23/2020
Reader rating
Rating: 5 / 5 (2)