What is a herniated disc?
The spine is the main support of the body and consists of 32-33 vertebrae (seven cervical C1-C7, twelve thoracic T1-T12, five lumbar L1-L5, five sacral S1-S5, and 3-4 coccygeal). Between two adjacent vertebrae there is an intervertebral disc, which is a flat round platform of connective tissue with a complex morphological structure (23 in total). The main function of the disc is to reduce the shock absorption of static and dynamic loads that inevitably arise during physical activity.
With age, intervertebral discs undergo degenerative processes that over many years make the fibers of the annulus fibrosus (the hardened edge of the disc) around the core brittle. In addition, the nucleus pulposus itself ages, with age it decreases its ability to retain water, hardens, becomes smaller and loses its shock-absorbing properties, as well as its ability to redistribute loads on the vertebrae. At the same time, the distance between the vertebrae decreases, the ligaments are weakened, and the fibers of the ring around the core are deformed. At the same time, the load on the spine, as a rule, does not decrease, and sometimes, on the contrary, increases - with increasing weight or physical activity.
At the MART clinic on Vasilyevsky Island
- Experienced doctors (including those practicing in the USA and Europe)
- Prices affordable for everyone
- Expert level diagnostics (MRI, ultrasound, tests)
- Daily 8:00 — 22:00
Make an appointment
Thus, the disc, under the influence of degenerative processes in the spine, cannot withstand. A hernia may occur: shift, protrusion and leakage of tissue of the nucleus pulposus from the intervertebral disc. The process occurs either in the spinal canal towards the back, or in the opposite direction - towards the abdomen, which happens much more often due to anatomical reasons, since the posterolateral sections of the fibrous ring are less strong and do not have protection in the form of a longitudinal ligament, like the anterior ones. Sometimes even extrusion of the nucleus (extrusion) occurs into the adjacent vertebra.
Symptoms and treatment of intervertebral disc herniation l4-l5 and l5-s1
Intervertebral hernia is a disease in which the core of the intervertebral disc is displaced through a gap formed in the fibrous ring.
It should be noted that this disease does not occur overnight; it is preceded by disc protrusion (protrusion without rupture of the fibrous ring).
But it often happens that the protrusion is asymptomatic, so the appearance of a disc herniation is often unexpected for a person.
Most often, this disease appears in the lumbar spine, much less often it occurs in the cervical spine, and extremely rarely in the thoracic spine.
The lumbar region is a vulnerable area of the back
Why is the lumbar region most often the site of intervertebral disc herniation? The reasons are simple. It is this part of the spine that takes on the maximum load; it is here that the center of gravity of a person is located. At the same time, the spine in this section has a fairly large range of motion, being one of the most mobile.
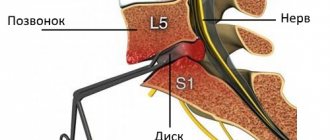
The most common disc herniation is l5 s1, slightly less common is disc herniation l4 l5. It is these intervertebral discs that are loaded to the maximum; they almost never “rest”. Even if a person is just lying down, they are under load.
We often simply don’t think about how heavy the load is on the lumbar region. And often, without understanding this, we do everything to make the disks “give up.” Just lifting a load with your back is worth it. But we rarely lift heavy loads correctly.
Causes of the disease
The cause of a spinal hernia can be either too active or too passive lifestyle
How does a disc herniation form?
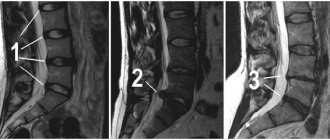
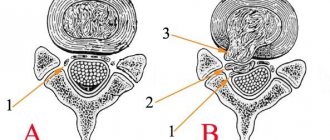
The process of the appearance of a hernia, its main stages, is illustrated in the figure.
The above diagram is conditional - for example, not every protrusion (bulge, protrusion) ends in sequestration.
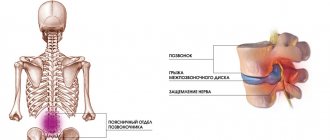
There is an extensive classification of intervertebral disc herniations based on the speed of appearance, shape, and distribution. At the same time, a disc herniation is dangerous not in itself, but because it affects surrounding tissues, primarily nerves, causing inflammation and swelling in the area of nerve endings. The consequence of the pressure of a hernia (median, foraminal, extraforaminal types) on the nerve roots can be pain, paresis, paralysis and sensory disturbances in the limbs, the intensity and nature of which directly depends on the location of the hernia in a particular part of the spine and inside the spinal canal.
Types of intervertebral hernias
The following types of intervertebral disc herniation are distinguished:
- protrusion;
- sequestered;
- median;
- extraforaminal;
Causes of medial disc herniation L4 L5 and treatment methods
Median disc herniation l4 l5 is a dangerous disease, since it damages the spinal canal. This type of hernia is more often diagnosed in people with a sedentary lifestyle. The disease is also provoked by constant flexion of the spine and its frequent injuries.
What does the diagnosis of “L4 L5 medial disc herniation” mean?
An intervertebral hernia is formed when the discs of the spine are displaced. If the displacement occurs in the middle of the spine, a median (medial) hernia is diagnosed. Often during this process, the fibrous ring is torn, it protrudes in the anterior or posterior direction.
In half of the cases, violations occur in the fourth and fifth vertebrae, as indicated by the corresponding numbers. The letter L means that these vertebrae are in the lumbar region.
If you do not seek medical help in a timely manner, a median hernia can lead to serious consequences.
Main symptoms of the disease
Medial disc herniation l4 l5 has different sizes.
At the beginning of the disease, a small protrusion appears, the painful sensations are weak, they start from the lower back and spread to the sacrum and the sides of the thighs. When the hernia grows, the pain goes below the knee. Symptoms of the disease usually appear as follows:
- aching pain of an intermittent nature in the lower back, it intensifies over time;
- pain and numbness in the legs;
- weakness when extending the foot;
- change in posture;
- marbling of the skin;
- sweating disorder.
Not all symptoms appear after the hernia begins to form; they develop as it grows.
If treatment is not started for a small disc herniation, it will gradually grow and rupture. Usually the posterior longitudinal ligament is torn. Because of this, the functioning of internal organs is disrupted, as a result of which the lower limbs can be paralyzed.
Diagnosis and treatment
To treat a hernia, it is better to consult a neurosurgeon.
A specialist can make a primary diagnosis based on the location of the pain. But to prescribe the correct treatment, the patient is sent for radiography, myelography or MRI. In the initial stages, the disease is treated with medication; surgery is performed in severe forms.
Operations for such a diagnosis are more complex, since due to the anatomical features, access to median hernias is inconvenient.
Due to the close location of the spinal cord, if manipulated incorrectly, there is a risk of severe complications.
A particular danger during surgical intervention is a median-paramedian hernia, in which protrusion occurs in the center and side.
Causes of intervertebral disc herniation
The process of a hernia can be sudden, for example, due to injury, stress, causing a sharp rupture of the fibrous ring, and gradual, for example, due to osteochondrosis - the contents of the disc can be partially squeezed out, diffusely through cracks in the edge of the disc.
The most common causes of a herniated disc include the following.
- Years of working with poor posture, such as bending over: e.g. office work
- Hard physical labor.
- Underdeveloped back muscles always increase the risk of disease because the vertebrae are less stabilized by ligaments and muscles.
- Excess weight also undoubtedly contributes to the wear of intervertebral discs.
- Pregnant women or women after pregnancy are also often affected.
- Sports loads, jerks, injuries, fractures, sudden movements carry the risk of a hernia.
- Sometimes we can talk about a genetic predisposition to instability of the intervertebral discs.
If you have any questions, ask our specialist! Ask a Question
Intervertebral hernia can occur in any part of the spine. The most common is intervertebral disc herniation in the lower lumbar spine (90 percent). The discs most often affected by deformation are the discs in the lower lumbar region of the back, especially at the L3-L4, L4-L5 and L5-S1 levels, because this part of the spine bears the brunt of the body's weight. Less common is a hernia of the cervical spine, and the thoracic spine is much less common.
In the lumbar spine, the likelihood of a hernia occurring between the ages of 30 and 50 years, the cervical spine suffers from a hernia more often between 40-60 years, and then the likelihood decreases. Disc protrusion can occur much earlier.
What symptoms does a herniated disc cause?
Many forms of disc herniation do not cause any discomfort (in about a third of cases). Pain occurs only when the bulging disc or extrusion of the gelatin core presses on sensitive nerve tissue. The intensity, type and nature of pain, and the appearance of other symptoms depend on the location of the hernia and its size.
In many patients, intervertebral disc herniation is combined with one or more pathologies:
- narrowing of the intervertebral space;
- localized osteophytes;
- vertebral displacement
Symptoms may progress slowly over weeks or months or occur suddenly; they may disappear and reappear spontaneously at intervals or be permanent and long-lasting.
In the most negative manifestation of an acute hernia, the pain can be perceived as severe, almost unbearable. The victim occupies a special position and is almost unable to move. At the site of extrusion, the muscles are very tense, and from there the pain spreads to neighboring areas of the body and limbs.
Symptoms of pressure on nerve roots
Pressure on the nerve roots always causes severe pain, which can spread to the limbs. Along with attacks of severe pain, feelings of tingling and numbness may also appear. Depending on the stage and severity of the symptoms of a disc herniation, a decrease in muscle strength or even paralysis of individual muscles may also occur.
Symptoms of pressure on the spinal cord
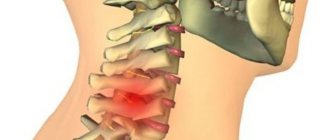
Depending on the location of the herniated disc, symptoms vary. Intervertebral hernias of the cervical spine can cause pain in the shoulder, arm, dizziness, pressure surges, and numbness in the fingers. Disc herniations in the thoracic spine can cause irregularities, cramps (spasms), pleural pain, heart pain or even paralysis of the limbs, while a large herniated disc in the lumbar spine can lead, for example, to paralysis of the bladder and legs. The condition of a patient with a large intervertebral disc herniation may be aggravated in the presence of spinal canal stenosis. Symptoms of pressure on the bundle of nerves in the lumbar and sacral regions (the so-called “cauda equina”): lack of bladder control and bowel function, sensory disturbances in the anal area and/or genitals, from the inner thighs to the feet, possibly paralysis of the legs. A herniated disc in the lower back can cause weakness in the legs and may make it difficult for the patient to lift the front of the foot.
Disc herniation l5 l5, l5 s1, l4 l5 - treatment, symptoms, diagnosis, paramedian disc herniation l4 l5
A spinal disc herniation is a bulging of the intervertebral disc beyond its physiological boundaries. It can be located in all parts of the spinal column, but the most vulnerable places are the lumbosacral and lumbar sections. The load here is the most intense, not only during physical work, but also during rest in a horizontal position of the body.
The sections of the spine are usually designated by Latin letters, L - lumbar, S - sacral, the numbers indicate a specific vertebra of a certain section. In the lumbar region there are five of them, in the sacral region five vertebrae are fused to each other, so a hernia occurs only at the level of the first vertebra of the sacral region.
Intervertebral disc herniation L5 S1 (L5 S1)
Intervertebral disc herniation L5 S1 is one of the most dangerous. In addition to physiological stress, compression of this area is often caused by improper redistribution of physical activity during sports.
Posterior disc herniation l5 s1 includes the concepts: median and paramedian. Their clinical picture is very similar. The difference is that paramedian disc herniation l5 s1 is the movement of the hernial protrusion relative to the center in the direction of the spinal canal. Median disc herniation l5 s1 is characterized by a location closer to the center.
Sequestered disc herniation l5 s1 is the most dangerous form of the disease, in which part of the intervertebral disc falls into the spinal canal. In addition to the fact that the proteins of the fallen sequester cause a strong local reaction, compression of part of the spinal cord is possible, which is extremely dangerous for the patient’s life.
The formation of a dorsal disc herniation l5 s1 most often occurs over a long period of time, under the “cover” of osteochondrosis. The patient is often treated for a long time for other diseases of the spine (scoliosis, osteochondrosis), but the formation of a hernial protrusion is possible.
The direction of the hernia towards the spinal canal is typical, so complex treatment of the pathology is necessary, not only to eliminate symptoms, but also to avoid dangerous complications.
Symptoms
With an existing hernia l5 s1, the symptoms predominate depending on the direction of the hernial protrusion, the stage of formation, the size of the hernia, and the presence of complications.
Common complaints that occur with all types of hernias of this section:
- pain in the lumbar region;
- pain radiating to the leg;
- decreased sensitivity;
- numbness of the limb.
The pain may travel down the inner thigh or be localized to the knee or ankle. In more complex cases, disturbances in the functioning of the internal organs of the pelvis occur.
Treatment
For a herniated disc l5 s1, conservative treatment is preferable in the first place, and if it fails or there are complications, the doctor recommends one of the surgical options for eliminating the pathology.
hernia treatment with traction
Treatment, both conservative and surgical, is selected for the patient, taking into account:
- type of hernia;
- intensity and duration of pain;
- existing complications;
- general state;
- presence of contraindications to medications.
Exercises for hernia l5 s1 are preferably done during the period of remission, and in the case of complex conservative treatment, after the inflammation of the strangulated tissues has been relieved.
They are aimed at developing and strengthening the back and abdominal muscles, as well as stretching the spinal column.
General physiotherapy, acupuncture, massage, and water procedures also give a positive effect with a properly selected set of measures.
Intervertebral disc herniation L4 L5
Often formed as a result of injuries or prolonged sedentary work. Incorrect posture, an inconveniently organized workplace, and concomitant diseases of the spinal column contribute to the disease.
Intervertebral disc herniation l4 l5 is classified similarly to herniations of other departments. The most common are median disc herniation l4 l5 and dorsal disc herniation l4 l5 (varieties of posterior disc herniation).
A hernia of the fifth lumbar vertebra provokes pain not only at the location, but also in the buttock, upper leg, and may radiate to the big toe.
Diagnosis of intervertebral disc herniation
It is impossible to determine on your own that back pain is caused by an intervertebral disc herniation. All the symptoms of a herniated disc can coincide with the symptoms of many other diseases. Therefore, if you have pain in the spine, you should make an appointment with a neurologist to get an accurate diagnosis and choose the right treatment method, taking into account contraindications.
The standard diagnosis is a detailed neurological examination. The doctor analyzes the medical history, checks reflexes, strength and sensitivity of the limbs, localization of pain, and the presence of disorders due to compression of the nerve roots. At the MART clinic, the clinical picture of intervertebral disc herniation is confirmed by objective data from an MRI examination of the spine.
Magnetic resonance imaging provides:
- general assessment of the entire spine;
- display of spinal cord tumors;
- identifying damaged disks;
- size and position of the intervertebral hernia.
In this case, the final conclusions based on the totality of examinations are made only by the attending physician.
Possible ways to treat cervical intervertebral hernia
When starting to treat this disease, specialists at Dr. Voight’s Clinic initially focus their efforts on eliminating pain and inflammatory processes. At this stage, it is important to stop the progression of the hernia. In this case, mandatory attention is also paid to other diseases of the spine, if any. Then, based on the patient’s individual testimony, he is prescribed therapeutic exercises. Exercises for it are selected taking into account the clinical picture.
Physiotherapeutic methods of treatment are widely used for intervertebral hernia:
- manual therapy;
- acupuncture and reflexology;
- different massage techniques;
- vacuum and laser therapy.
Excellent results in the treatment of cervical intervertebral hernia were achieved at Dr. Voight’s Clinic thanks to Professor A.N. Voitsitsky, who patented his own method of treating scoliosis and spinal hernias. The main idea of the method of Dr. A.N. Wojcicki is a clear division of the disease based on specific symptoms. Then, depending on the type and condition of the disease, treatment procedures are selected. The purpose of this technique is to “switch on” and strengthen in the body the processes of regeneration of damage and restoration of lost functions. The techniques of this technique are aimed at stimulating metabolism and blood circulation in the damaged parts of the spine, which allows one to avoid surgical intervention. It is important to remember that the best prevention of spinal diseases is a balanced, proper diet, moderate but regular physical activity, as well as general strengthening of the body.
In this article we tried to answer your questions:
- What is a cervical disc herniation?
- What are the symptoms of a cervical disc herniation?
- How to treat a herniated cervical spine?
- Why should a cervical disc herniation be treated at Dr. Voight’s Clinic?
Treatment of herniated disc at the MART clinic
In most cases, treatment of intervertebral hernia is carried out without surgery. Conservative treatment for lumbar disc herniation usually includes:
- Prescription of analgesics and non-steroidal anti-inflammatory drugs.
- Epidural steroids in severe cases.
- During an exacerbation, wearing a corset or belt, which will primarily limit excessive movements of the spine.
- Complex of physical therapy (physical therapy).
- Complex of physical therapy during remission.
Drug treatment
Drug therapy (pharmacotherapy) plays a significant role in relieving attacks of pain in spinal disorders, in particular such as herniated discs. Usually for moderate pain, NSAIDs such as ibuprofen, diclofenac, indomethacin, which are usually used in the form of tablets, capsules or suppositories, sometimes as intramuscular injections or intravenous infusions.
In case of acute pain, steroidal anti-inflammatory and decongestant drugs are prescribed. Corticosteroids should only be taken under medical supervision and only as prescribed by a doctor due to the nature of these medications.
For drug treatment of disc prolapse, muscle relaxants are simultaneously used, which relax the muscles, enhancing the pain-relieving effect caused by NSAIDs.
Using analgesics over a long period of time can lead to serious side effects. Therefore, the methods and dosages of medications for pain relief in the case of a herniated disc are always determined by the doctor. Only he can prescribe the correct treatment, taking into account the assessment of the individual degree of the disease
In the MART center, in addition to traditional medicinal forms of treatment, pharmacopuncture and reflexology (acupuncture, acupuncture) are also used.
Intervertebral hernia of the thoracic region
In neurology, intervertebral hernia of the thoracic region is classified into central and lateral. In the first case, the hernia manifests itself with symptoms of spinal cord compression—compressive myelopathy with the development of lower mono- or paraparesis and pelvic disorders. Due to the fact that discogenic myelopathy in the thoracic region is caused by compression of the motor pathways, paresis is central (spastic) in nature. A lateral hernia debuts with signs of irritation and compression of the corresponding spinal root - pain syndrome (sciatica) and sensory disturbances in the chest area. As part of the spinal nerves of the thoracic region, visceral branches go to many internal organs: trachea, lungs, bronchi, esophagus, liver, duodenum, gall bladder, kidneys. Therefore, a thoracic hernia may be accompanied by functional disorders of the corresponding visceral organs. The localization of these symptoms depends on the level of location of the hernia, and therefore it is customary to divide thoracic hernias into upper, middle and lower.
Upper thoracic hernia
(Th1-Th4) is manifested by pain (thoracalgia) and paresthesia in the upper chest, interscapular region. Thoracalgia in the left half can simulate clinical angina. A hernia at the Th1-Th2 level is accompanied by paresthesia and weakness in the arms, numbness of the hands. Possible disturbance of esophageal peristalsis and difficulty swallowing.
Middle thoracic hernia
(Th5-Th8) often occurs with symptoms of intercostal neuralgia - unilateral or bilateral shingles along the intercostal spaces, reminiscent of herpes zoster, but not accompanied by blistering rashes. Such pain can limit the respiratory excursion of the chest with the formation of more shallow and rapid breathing. Possible pain in the stomach area. In some cases, a thoracic hernia can cause dyspepsia, pancreatic enzyme deficiency, insulin secretion disorders, and disturbances in carbohydrate metabolism.
Hernia of the lower thoracic region
(Th9-Th12) occurs with pain localized in the kidney area, under the ribs, in the upper abdomen, sometimes simulating an “acute abdomen”. Right-sided pain in the hypochondrium can be mistaken for manifestations of liver pathology, acute cholecystitis or appendicitis, and intense pain around the chest for acute pancreatitis. A hernia at the Th11-Th12 level can provoke intestinal dyskinesia.
Physiotherapy
Depending on the indications, a set of physiotherapeutic procedures is prescribed aimed at:
- reduce pain;
- relieve inflammation;
- accelerate the resorption of edema (reduce swelling);
- relax the muscles;
- improve spinal function;
- strengthen muscle strength.
At the MART center, a wide range of physiotherapeutic procedures using laser, ultrasound, magnetic therapy, electrotherapy, vacuum therapy, and peloid therapy are used to treat intervertebral hernia.
All procedures in one form or another cause an effect on the affected areas of the spine and adjacent tissues at the cellular level, improving the nutrition of the intervertebral disc, microcirculation of blood and lymph, promoting the restoration of cartilage, and preventing degenerative changes.
In an acute condition of lumbar disc herniation, medical therapy, a system of therapeutic physical exercises and the patient’s purposeful work on himself can simultaneously bring relief.
The course of treatment usually lasts several months, as a result of which physical performance for everyday life and work is restored. The condition stabilizes, the likelihood of relapse decreases, and it becomes possible to live without pain symptoms for a long time.
As a result of a course of treatment at the MART center for intervertebral disc herniation, patients receive growing confidence in their own body, decreased anxiety, and the opportunity to return to a normal lifestyle.
The article was reviewed by Doctor of Medical Sciences, Professor Grigory Isaakovich Shvartsman, Northwestern Medical University. I.I. Mechnikov.
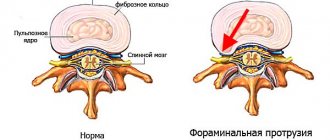
Types of intervertebral disc protrusions
Spinal disc protrusion is a protrusion of the outer contour of the disc beyond the size of the vertebrae. Unlike a hernia, the protrusion does not have a significant size (depending on the part of the spine, its size is 2-5 mm) and in the presence of protrusions, the outer fibrous ring of the disc is not damaged . Disc protrusions differ not only in their location, but also in the direction of displacement. But it is the direction of the protrusion that often plays a determining role regarding its danger.
From this point of view, there are the following types of protrusions:
Dorsal
Median
Foraminal
Paramedian
Circular protrusions
Ventral (anterior)
Let us consider the features of each type of protrusion in more detail.
Dorsal protrusion
The most common type of protrusion. Sometimes this type is also called posterior protrusion. From its name it follows that the direction of disc protrusion goes back towards the intervertebral canal. In turn, dorsal protrusion, depending on the type of disc prolapse, can be divided into 4 more subtypes.
Circular protrusion - protrusion occurs along the entire edge of the disc. In this case, a kind of expansion of the vertebra occurs due to the disc. Circular protrusion is divided into the following subtypes : foraminal , uniform or dorsal . The specific differences between these species are clearly visible in the figures.
Circular-Foraminal
Circular-Uniform
Circular-Dorsal
The foraminal protrusion expands towards the intervertebral canal. This type of protrusion is quite dangerous, since the disease can directly affect the roots.
Foraminal protrusion
Ventral protrusion. The ventral one is characterized by bulging of the discs without the possible threat of pinching the nerve roots.
Ventral protrusion
Median disc protrusion - protrusion occurs not only in the direction of the spinal canal, but in its center itself; it is the most dangerous if treated incorrectly, since there is a risk of pinching the nerve roots.
Median disc protrusion
Paramedian protrusion. The paramedian type of protrusion is in many ways similar to the median one, with the peculiarity that the paramedian one is directed slightly away from the spinal canal.
Paramedian protrusion.
Intervertebral disc protrusion: Treatment
Disc protrusions are most successfully treated with conservative methods. Each program is compiled strictly individually; the program may include:
- — Spinal traction for a short period of time. Read more about Detenzor safe traction
- — Reducing prolonged sitting, especially with protrusions of the lumbar spine
- — Physical therapy, the main goal of which is to strengthen the muscular corset of the spine
- — Physiotherapy: Shock wave therapy , Magnetotherapy , Laser therapy , Ultrasound therapy , Bubnovsky MTB simulator
- — Improving posture and correcting diet