The intervertebral discs located between the vertebral bodies are characterized by a gradual decrease in size and wear. With age, they increasingly lose their natural elasticity and their inherent firmness, so degenerative-dystrophic changes in them are almost inevitable.
The lumbosacral spine is most susceptible to stress. That is why the vertebrae and intervertebral discs that form it most often suffer from destructive changes. And the maximum static-dynamic load falls on the L5–S1 disc located on the border of the lumbar and sacral spine. Therefore, in approximately 50% of all cases of intervertebral hernia formation, it occurs.
Peculiarities
The L5–S1 intervertebral disc is located between the last lumbar vertebra and the sacrum. This is the largest disc in the spine, the diameter of which significantly exceeds the height. But due to the high load placed on him, he more often than others suffers from the development of osteochondrosis, then protrusion and, ultimately, a hernia.
But if previously such changes were mainly observed in older people, today intervertebral hernias have become much younger and are increasingly occurring even in young people. The main reason for their formation is advanced osteochondrosis. Create the prerequisites for its development:
- sedentary lifestyle, sedentary work;
- overweight;
- regular performance of heavy physical labor;
- back injuries;
- spinal deformities in any plane;
- genetic predisposition.
Thus, under the influence of these factors, degenerative-dystrophic changes begin in the tissues of the L5–S1 intervertebral disc. Initially they affect the inner part of the disc - the nucleus pulposus. Tears gradually form in its fibers, which leads to an uneven distribution of pressure on the surrounding fibrous membrane. Under the influence of the shifting nucleus pulposus and pressure from the vertebrae, it experiences serious overloads, as a result of which the fibers of the fibrous ring also begin to gradually stretch and tear in the place where their strength is minimal as a result of injury or other factors.
Thus, the symmetry of the intervertebral disc is disrupted. At a certain point there is a slight protrusion of the nucleus pulposus and the entire disc beyond the vertebral body. But since the nucleus pulposus still remains within the annulus fibrosus, in such situations L5–S1 disc protrusion is diagnosed.
The shock-absorbing properties of the disc begin to decline immediately after the first changes occur in it. Even a slight protrusion can lead to disturbances in the patient’s well-being and pain syndrome.
If no action is taken at this stage, the deformity will worsen, since the pressure of the vertebrae on the disc does not disappear, and the fibers of the fibrous membrane continue to be subject to constant pressure. As a result, it cannot withstand and ruptures, against which prolapse and herniation of the L5-S1 disc are diagnosed.
Thus, a passage is formed in the fibrous ring, through which the nucleus pulposus is able to get out, that is, into the spinal canal. This is what leads to the development of acute neurological symptoms characteristic of a hernia, since a mass of nerve endings from the cauda equina pass through the spinal canal. Therefore, the appearance of even a small foreign body in it leads to their infringement and the occurrence of corresponding disturbances in the functioning of those organs for the innervation of which they are responsible.
Therefore, with a hernia of the L5–S1 spine, severe pain is observed not only in the lower back, but also in the legs, feet, toes, sacrum, buttocks, etc. There is also a violation of their sensitivity, extinction of reflexes and other changes. Moreover, the nature of the clinical picture largely depends on the type of hernia.
Causes
The main cause of the formation of a herniated intervertebral disc (IVD) is spinal osteochondrosis.
Factors that increase the risk of developing the disease are:
- lumbalization or sacralization;
- congenital narrowness of the spinal canal;
- asymmetrical arrangement of intervertebral joints;
- referred myofascial (muscle) pain;
- referred pain in diseases of a number of internal organs (spondylogenic somatic)
- physical stress;
- exposure to vibration;
- sedentary lifestyle;
- obesity;
- smoking.
Types of intervertebral hernias
A bulging intervertebral disc can form both in the back of the spine and on the inside. Based on this, anterior and posterior (dorsal) hernias are distinguished. The former do not pose any particular danger and almost never lead to disruption of a person’s well-being. The latter protrude into the spinal canal, where the nerves pass, and can cause severe neurological complications.
There are several types of dorsal hernias:
- median;
- paramedian;
- foraminal;
- circular (diffuse).
The final stage of development of each of them is sequestration, i.e. separation of the prolapsed part of the nucleus pulposus. Sequestered hernias can move along the spinal canal and cause spinal cord stenosis, which is accompanied by severe neurological disorders. Such protrusions must be immediately treated surgically.
Also, all hernias can be divided into 3 categories depending on their size:
- small – less than 5 mm;
- medium – reach 5 – 7 mm;
- large - more than 8 mm.
Median
The protrusion is located precisely in the center of the spinal canal and can cause pain in the lower back, radiating to the back of the thighs and legs. If the formation is large, disturbances in the control of urination processes may occur, and the sensitivity of the legs may decrease, which leads to paresis or paralysis.
Paramedian
They form on the left or right side of the spinal canal, which leads to the development of unilateral symptoms, as well as burning pain in the perineum, numbness of the groin area and significant difficulty in urinating or defecating, even if there is a strong urge.
Foraminal
Localized in narrow openings formed by the vertebral bodies and their articular arches. Nerves run through them. Therefore, even the smallest hernias can provoke severe neurological disorders and severe pain.
Diffuse
In such cases, the entire posterior surface of the intervertebral disc protrudes and, as it grows, is able to fill the entire space of the spinal canal, the size of which usually does not exceed 1.5–2 cm. A hernia of this type is characterized by the presence of pain even in a state of complete rest, as well as the presence of sensation tingling in the legs and weakness, which can ultimately lead to loss of the ability to move and control over urination and bowel movements.
Symptoms
Pathological changes in the L5–S1 intervertebral disc almost immediately lead to pain and other symptoms of the disease. They significantly reduce the patient’s quality of life and require immediate treatment. This is due to the fact that at the level of the L5–S1 disc there are a large number of nerves of the cauda equina, so the slightest infringement of them provokes the development of serious disorders not only at the location of the hernia, but also in the parts of the body corresponding to the injured nerves.
They include:
- severe pain in the lower back and sacrum, radiating to the legs and tending to intensify when sitting;
- numbness of the back of the thighs, perineum and sometimes the little toes;
- loss of ability to stand on tiptoes;
- fatigue when walking;
- swelling of the lower extremities;
- weakness of the muscles of the lower extremities and a decrease in their volume;
- decreased severity of the knee and Achilles reflex;
- disturbances in control of urination and defecation;
- erectile disfunction.
At the same time, the size of the L5–S1 intervertebral hernia does not play a primary role in the severity of symptoms. There are often cases when large formations practically did not bother patients at all and were discovered by chance, or very small hernias provoked the occurrence of powerful attacks of pain.
Diagnostics
Diagnosis of the disease begins with a survey and examination of the patient by a chiropractor, neurologist or vertebrologist. A number of tests suggest the presence of an intervertebral hernia. But for its accurate diagnosis, instrumental research methods are required.
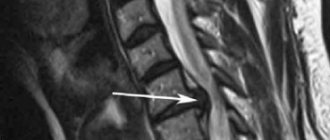
Various methods are used to detect L5–S1 hernias, but MRI is the most informative. Magnetic resonance imaging makes it possible to thoroughly study the features of pathological protrusion of the disc, its size and position. Therefore, patients are always prescribed this study first.
It can be carried out in closed and open type devices. The former are more preferable, since they create a magnetic field of 1.5–3 Tesla. This ensures that the most informative images are obtained. But due to the fact that the procedure involves immersion in a special closed tube of the device, it cannot be performed on patients with severe claustrophobia. In such situations, MRI is performed in open-type machines in which the magnetic field power does not exceed 1.2 Tesla.
The examination takes about 20 minutes, during which you must remain absolutely still. This is a guarantee of obtaining high-quality images.
To assess the condition of the vertebrae and their position, a CT scan and x-ray of the spine are additionally prescribed. Also, these diagnostic methods are used when it is necessary to examine patients who have metal structures in the body, since this is a contraindication for MRI. CT and X-ray images can be used to measure the height of intervertebral discs, osteophytes, spinal fractures, instability of spinal motion segments, osteoporosis and developmental anomalies.
If there are disorders in the leg muscles, electromyography is performed. It allows you to evaluate the quality of transmission of nerve impulses to muscle receptors and evaluate their tone. All this together makes it possible to develop optimal treatment tactics that will bring the most pronounced results in a short time.
In our clinic, you can also learn in more detail about the composition of your body and the state of the vascular system, which is involved in the blood supply to internal organs, skeletal muscles, and the brain. Our experienced doctors will explain the data obtained to you in detail. Bioimpendansometry calculates the ratio of fat, muscle, bone and skeletal mass, total fluid in the body, and basal metabolic rate. The intensity of recommended physical activity depends on the state of muscle mass. Metabolic processes, in turn, affect the body's ability to recover. Based on the indicators of active cell mass, one can judge the level of physical activity and nutritional balance. This simple and quick test helps us identify disturbances in the endocrine system and take the necessary measures. In addition, it is also very important for us to know the condition of blood vessels for the prevention of diseases such as heart attacks, hypertension, heart failure, diabetes and much more. Angioscan allows you to determine such important indicators as the biological age of blood vessels, their stiffness, stress index (which indicates heart rate), and blood oxygen saturation. Such screening will be useful for men and women over 30, athletes, those undergoing long-term and severe treatment, as well as everyone who monitors their health.
In this case, body composition analysis gives us information that adipose tissue predominates in the body, and the musculoskeletal component is in relative deficiency. These data will help the rehabilitation doctor competently draw up a physical activity plan, taking into account the individual characteristics of the patient.
Recovery prognosis
Conservative treatment brings relief in 70% of cases , but may last several years. The earlier the disease is diagnosed, the more successful it is. If you follow all the doctor’s recommendations, the disease goes into remission, but you must constantly protect the spine by all available means.
In some cases, after additional examination, surgical treatment is required . This is a way to get rid of the disease quickly and for a long time, although in rare cases relapse and even immobilization are possible.
Treatment of spinal hernia L5–S1 without surgery
Patients with a diagnosed L5–S1 intervertebral hernia are prescribed complex therapy, which is aimed at eliminating all links in the pathological chain and improving the patient’s well-being conservatively, without surgery. It is developed individually for each patient. In this case, not only the features of the protrusion are taken into account, but also existing concomitant diseases, which are often the result of degenerative processes in the spine, as well as the characteristics of his work and everyday life.
The main components of conservative therapy are:
- drug therapy;
- osteopathy;
- manual therapy;
- massage;
- physiotherapy (phonophoresis, carboxytherapy, ozone therapy);
- individual lessons with a rehabilitation specialist;
- diet.
It is important to reconsider your lifestyle and eliminate the prerequisites for the development of hernias. Office workers, drivers and representatives of other sedentary professions are advised to take a break every hour and walk, warm up and generally move more. Those who are accustomed to doing heavy physical work every day should consider changing it to another type of activity, since constant overload of the spine does not allow conservative therapy to bear fruit.
If the patient consults a doctor too late and the L5–S1 hernia has reached an impressive size, provoked severe neurological complications or entered the stage of sequestration, conservative therapy will be powerless. In such situations, the patient is referred to a neurosurgeon for surgery to remove the hernia and decompress the nerve roots.
Drug therapy
Drug treatment is aimed at eliminating pain, as well as improving nerve conduction, metabolic processes and the condition of the intervertebral disc. Therefore, patients are prescribed a whole range of medications that need to be taken in courses. Sometimes their duration is several months.
So, for a hernia of L5–S1, the following are prescribed:
- NSAIDs are drugs that have analgesic and anti-inflammatory properties and are available in the form of tablets, ointments, gels, creams and solutions for injection (the required form of administration is chosen by the doctor based on the severity of the clinical picture);
- corticosteroids are hormonal drugs that have a pronounced anti-inflammatory effect and are prescribed for severe inflammatory processes;
- muscle relaxants - medications whose main function is to eliminate muscle spasms, which is often a reflex reaction of the body to the ongoing inflammatory process;
- psychotropic drugs - used to increase the effectiveness of NSAIDs and muscle relaxants, as well as improve the psycho-emotional state of the patient;
- B vitamins - designed to improve nerve conduction and reduce the severity of neurological disorders;
- vitamin D is a remedy responsible for the condition of bone tissue, as well as for higher brain functions, such as memory, memory, attention, speech;
- chondroprotectors - contain glucosamine and chondroitin, which are building materials for cartilage tissue, so their use should lead to acceleration of the regeneration processes of intervertebral discs. We recommend Mermaids Marine Collagen to our patients. ;
- biostimulants - designed to activate metabolic processes.
The duration of use of drugs, their specific trade names and dosages are selected individually. During treatment, patients are required to have follow-up appointments, at which the effectiveness of the therapy is assessed and, if necessary, adjustments are made.
For severe, unbearable pain that cannot be eliminated with non-steroidal anti-inflammatory drugs, blockades are prescribed. They can only be performed by a highly qualified specialist, since the procedure involves injections of anesthetics into the epidural space or the site of the affected nerve branch.
Thus, unprofessional implementation of the blockade is fraught with aggravation of the situation and the development of severe, sometimes irreversible complications. Therefore, they can only be done in specialized medical institutions under complete antiseptic conditions. Four blockades are allowed per year.
Manual therapy
One of the important components of complex treatment of L5–S1 disc herniation without surgery is manual therapy. It is carried out outside periods of exacerbation and allows you to achieve a significant improvement in well-being, activation of tissue trophism and restoration of the anatomy of the spine.
Manual therapy involves the use of a number of special techniques through which muscle tension is eliminated, which already helps to reduce the severity of pain, as well as improve blood circulation in the affected area. This ensures more active saturation of tissues with nutrients, oxygen, intensification of metabolic processes and the creation of favorable conditions for the restoration of cartilage tissue.
But this alone is not enough to obtain a pronounced result. The possibilities of modern manual therapy make it possible to have a comprehensive effect on the human body by normalizing the condition of the spine. This idea underlies Gritsenko’s original method.
It has long been proven that the spine is in close relationship with all organs and structures of the human body. Therefore, the occurrence of pathological changes in it leads to disruption of the functioning of internal organs.
Since isolated formation of intervertebral herniation L5-S1 almost never occurs, other parts of the spine also suffer from degenerative changes. Manual therapy using the Gritsenko method allows you to normalize the position of each vertebra, eliminate spinal deformities, as well as compression of nerves, including those passing at the L5–S1 level, and relieve the patient from neurological symptoms.
The method involves precision, fully conscious actions, which will be different for each patient, since in each case a solution to different problems is required. As a result, after the first session, a significant improvement in the patient’s condition is noted, and the most favorable conditions are created for the restoration of intervertebral discs. The subsequent ones only further improve the patient’s well-being, and additionally eliminate the causes of a huge number of diseases of the internal organs, including diseases of the heart, respiratory system, gastrointestinal tract, kidneys, etc.
At the same time, manual therapy gives stable, long-lasting results. But you can only trust highly qualified specialists who thoroughly master the technique of performing the procedure and understand what features of the spine need to be taken into account in each specific case.
Physiotherapy
To increase the effectiveness of manual and drug therapy, patients are required to undergo courses of physiotherapeutic procedures. They are also designed to reduce the intensity of pain and produce an anti-inflammatory effect. For these purposes the following are appointed:
- electrophoresis;
- laser therapy;
- ultrasound therapy;
- UHF.
But the most widely used is traction therapy or spinal traction. The essence of the method is to use a special device, the loops of which are attached to the patient’s body. It creates a tensile load on the spine, which gradually leads to an increase in the distance between the intervertebral discs and, accordingly, a decrease in pressure on the intervertebral disc.
After the procedure, the patient should remain lying down for at least an hour and then put on an orthopedic corset. This will help maintain the achieved result and create favorable conditions for the natural regeneration of the L5–S1 disc.
Exercise therapy
For each patient who decides to treat a spinal hernia L5–S1 without surgery, a rehabilitation physician individually develops a set of exercises that will help strengthen the muscles and serve as a preventive measure for worsening the condition. The complex is selected by a specialist in exercise therapy. When compiling it, the nature of the existing disorders, the level of physical development of the patient, as well as the presence of concomitant diseases are taken into account.
The first classes must be carried out under the supervision of a doctor, and only after the technique of performing all the exercises has been fully mastered and the load has been selected ideally, are you allowed to practice therapeutic exercises at home on your own. You need to do this exercise every day. In this case, all movements are performed smoothly, without jerking. If pain occurs during any of them, you must stop immediately and consult a doctor as soon as possible.
Exercise therapy should become the norm for the patient. They can not only improve the condition of the affected intervertebral disc, but also prevent the formation of hernias and protrusions in other parts of the spine.
Diet
Diet is important to improve the quality of recovery processes and normalize weight, since extra pounds create extra stress on the intervertebral discs and contribute to their protrusion. Therefore, patients are recommended to switch to fractional meals with limited fat intake.
It is recommended to eat small portions 5-6 times a day. You can include almost any food in your diet, but special preference should be given to vegetables, fruits, lean meats and fish. It is important to achieve a balanced diet, so it is better to consult a nutritionist to prepare it.
It is recommended to refuse:
- fatty, spicy dishes;
- salty foods;
- canned food, marinades;
- confectionery products;
- fast food, snacks;
- alcohol.
You should drink at least 2.5 liters of water daily. These measures are often sufficient to smoothly reduce weight to normal values, as well as saturate the body with all the nutrients necessary for its proper functioning.
Possible complications
Ignoring the problem, reluctance to go to the doctor and self-medication for a hernia L5–S1 is fraught with the development of severe complications, including:
- hernia sequestration;
- spinal canal stenosis;
- complete paralysis of the legs;
- loss of control over urination and bowel movements;
- persistent impotence.
Therefore, at the first signs of deviations from the norm, you should contact a chiropractor, neurologist or vertebrologist. The doctor will be able to select the most effective therapy for a given patient, which will help not only eliminate the unpleasant manifestations of the disease, but also affect the condition of the disc itself.
Thus, a hernia of the L5–S1 spine can pose a serious danger, but if you seek medical help in a timely manner, it can be effectively dealt with and a high quality of life can be maintained.
0 0 votes
Article rating
Consequences
A medial hernia is especially dangerous due to the risk of damage to the spinal canal . When it is diagnosed early, conservative treatment using traditional methods is possible.
A medial hernia is dangerous because there is a risk of damage to the spinal cord
With serious protrusions of the nucleus, the ligament or even the membrane of the spinal cord may be damaged. And this is fraught with paraparesis and pelvic pathologies of varying degrees. In the worst case, even surgery does not help, and paralysis of the legs is inevitable.