The anatomical structure of the acetabulum of the pelvic bone determines the functionality of the lower extremities and femoral region. With the help of this element, a person performs about 40% of movements: flexion, extension, bending, hip abduction forward, backward, to the side. Damage to the acetabulum can lead to disability. Most often in medical practice, fractures, dislocations, thinning of cartilage tissue or impaired blood supply and metabolism occur. To identify the disease at an early stage, you need to know your own anatomy and how healthy joints function.
What is the hip joint?
It is the most powerful and largest in the human body. In addition to functions such as flexion and extension, abduction of the hips back, forward, to the sides, and rotational movements, it is also involved in bending the body.
The characteristics of this joint are unique - they provide about 40% of human movements.
It is formed by the head of the femur, as well as a depression called the acetabulum. The hip joint is deeper than the shoulder joint. Both of its elements are covered with cartilage tissue, which can absorb loads, smooth out movements when walking, running, jumping, etc.
Pathology
The hip joint, with all its advantages, also has the greatest tendency to injury, since the entire weight of the human body constantly presses on it. One of the common ones is femoroacetabular impingement syndrome, otherwise called impingement syndrome. The mechanism of formation of this disease is quite simple: when performing movements, the femoral neck comes into contact with the edge of the acetabulum. This is only possible if the cartilage of the joint is very thick or has an uneven surface.
In traumatology, there are two types of this syndrome:
- Eccentric, when the cause of contact is the incorrect configuration of the femoral head. It may have bumps, protrusions, or other defects.
- The pinser type is associated with a pathological increase in the cartilaginous covering of the cavity.
Anatomy
The acetabulum is a depression in the ilium, which is part of the pelvic bone. It performs important and complex functions in the body, such as support and movement. It has a hemispherical shape, covered on the inside with cartilage. Doctors distinguish the posterior and anterior walls of the acetabulum, as well as its arch. Considering that this part of the pelvic bone ensures human movement, it is very important to promptly detect pathology in this area and quickly carry out treatment.
The acetabulum is formed by the pubis, ischium, and ilium at their junction.
Other joint elements
The socket in question and the head of the femur form the hip joint, in which, in addition to the key structures, there are also not so strong and strong, but no less important elements:
- Synovial membrane. It provides the necessary amount of fluid to lubricate the surfaces of the joint, nourishes it and provides innervation.
- Synovial bursae are duplications of the synovial membrane that form depressions in which fluid accumulates. Their task is to reduce friction between bone elements.
- Vessels. The corresponding artery provides nutrition to the head of the femur. It takes care of all the nutrition of the joint and in the event of a fracture, the chance that the blood supply will return to normal is extremely small. In addition, large arterial trunks lie in the joint area, which makes injuries in this area especially dangerous.
- Nerve endings. In this case, these are branches of the sciatic, obturator and femoral nerves. That is why, when a joint is damaged, there will be no pain directly at the site of the pathological process, but it will radiate to the sacrum, groin or leg.
Fracture
Most often, such a violation of bone integrity occurs as a result of an accident. This injury can also occur after a fall from a great height.
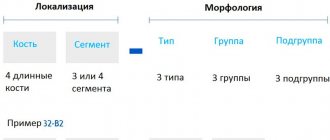
Acetabular fractures can be divided into 2 types:
- Simple damage. These are fractures of the anterior column, posterior and middle walls, and transverse injuries.
- Complex damage. This is when the fracture line passes through several parts of the bone at once. This includes injuries to the anterior wall, transverse wall, both columns, etc.
Symptoms of a fracture may include:
- Pain in the groin and hip area.
— It is difficult for the patient to lean on the injured leg.
- A clear manifestation of shortening of the limb, which is bent at the hip and knee joints. The leg is externally rotated.
Symptoms
A fracture of the posterior sections of the cavity is accompanied by significant pain. At the same time, movements are sharply limited. Cracks in bone tissue are accompanied by aching pain.
Many people mistake these signs for arthritis. If you have any difficulties with movement, you should contact qualified specialists. This will prevent the appearance of injury.
It is worth noting the following signs of the disease:
- Pain in the hip and groin area.
- Forced placement of limbs.
- Limitation of mobility.
- Difficulty leaning on the injured limb.
- The appearance of crunching and clicking sounds.
- Swelling and redness of the affected area.
With a combination of violations of the integrity of the anterior and posterior surfaces, the appearance of a shock state is observed. Accurate diagnosis will allow timely treatment and reduce the risk of consequences.
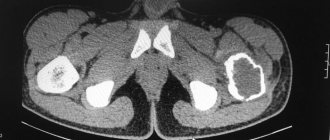
The doctor may order an x-ray to evaluate the degree of ossification. To make a diagnosis, a CT scan of the pelvic area is also performed. The technique helps determine the degree of fracture. In some cases, the fracture is accompanied by a violation of the sciatic nerve. In addition to the fields of traumatology and orthopedics, neurology also deals with the problem.
Fracture treatment
— If a violation of the integrity of the bone occurs without displacement, then the patient is given a standard splint, as well as a special adhesive plaster traction for the lower leg for a period of 1 month. A course of physical therapy and electrophoresis must be prescribed.
— If the acetabulum of the pelvic bone is broken in the upper and posterior edges, resulting in a dislocation of the hip, then treatment is carried out by skeletal traction. The specialist passes the needle through the epicondyles of the femur. Thanks to this manipulation, the joint capsule is stretched, and the fragments of the acetabulum are pressed, that is, compared. The duration of traction is usually 1.5 months.
“If the fragment is large and cannot be matched, then surgery is necessary. It should be carried out in the first two weeks after injury, not later. To fix the fragments of the cavity, surgeons use plates and lag screws.
After treatment of a fracture, the rehabilitation period is very important.
Rehabilitation
To speed up the recovery of injured segments of the cavity during the rehabilitation period, patients are prescribed physiotherapy, exercise therapy, and massage.
The last of these manipulations is aimed at eliminating violations of the tone of the muscles of the buttocks and the front surface of the thighs, improving trophism. The procedures are carried out by a clinic specialist manually or using cryopackages.
The list of the most popular methods of physiotherapy for fractures, allowing to eliminate inflammation and activate the activity of damaged systems:
- treatment with magnets;
- UHF;
- electrical stimulation.
Physical education classes are supervised by an instructor. The load increases gradually. A standard exercise therapy course includes:
- flexion-extension of the feet;
- swing your legs;
- circular movements of the limbs;
- walking (with and without support, forward with your back, sideways).
Light running is prescribed after 7-8 months. after receiving damage.
Therapy for a fracture of the posterior edge of the socket
This pathological transformation occurs during an accident or fall from a height. Mostly young people are susceptible to this trauma. A fracture is accompanied by displacement of fragments, bone dislocations, destruction of articular surfaces and cartilage. The edge of the acetabulum of the anterior section is observed in isolated cases. In most cases, posterior column fractures are found.
In a hospital setting, a specialist examines the victim using plain radiography of the pelvis. In an emergency, under epidural anesthesia or intravenous anesthesia, the doctor reduces the dislocation. After this, a final diagnosis of joint damage is carried out, including radiography in the iliac, survey, oblique projection, as well as computed tomography. Such research methods help the specialist to obtain a complete picture of damage to such a recess as the acetabulum.
In this case, only surgical intervention will help to put a person on his feet. The doctor makes an incision along the line where the fragment is localized. Next, the doctor fixes it with a screw or acceptable compression. Checks the stability of the fragment's fixation and then sutures the wound.
Damage diagnostics
To make an accurate conclusion, the doctor, in addition to examining and interviewing the patient, conducts a number of additional studies. The complex of the latter makes it possible to clarify the preliminary diagnosis.
Instrumental, laboratory
Hemisphere injuries are identified by involving:
- X-rays of the pelvis. Pictures are taken in oblique, direct projections. Analysis of the results of the review technique allows us to assess the severity of the injuries received by the patient.
- CT scan of the injured area. The use of computed tomography helps visualize the fracture and clarify the diagnosis made by the specialist initially.
- MRI. The research method increases the information content of the conclusion and provides grounds for prescribing surgical intervention.
The study of biological fluids (blood, urine) of the victim helps to identify possible damage to internal organs. If unsatisfactory test results are obtained, ultrasound is used.
Differential
In order to differentiate traumatic deformities of the cavity from other pathologies, CT is mainly used.
A rectal (vaginal) examination of the patient allows us to determine the presence (absence) of bone fragments.
If tears of the acetabular labrum are suspected, arthroscopy of the hip joint is performed.
The fact of damage to nerve fibers is determined when the patient is examined by a neurologist (neurosurgeon).
Recovery
When the acetabulum of the pelvic bone has been reanimated after a violation of its integrity, it is very important to follow the following rules of rehabilitation:
- Do special breathing exercises every day.
— Learn to walk correctly on crutches and step on your feet.
— Perform a special set of exercises under the supervision of an orthopedist: flexion and extension of the toes, rotation of the feet, raising and lowering the pelvis with support on the bent healthy lower limb and two arms.
Osteoarthritis of the hip joint
A sign of this disease is sclerosis of the acetabulum, which is observed only on x-rays. This term is often found in descriptions of images taken by radiologists.
This problem develops due to inflammatory changes in the bones with overgrowth of connective tissue.
Acetabular sclerosis is a condition in which external symptoms of the disease – arthrosis – are not observed. This problem is common among older people. The main causes of sclerosis of the cavity are:
- Thinning of cartilage.
— Impaired blood supply to the legs due to ailments associated with metabolism.
— Hereditary predisposition to arthrosis, osteochondrosis.
- Dislocations when walking.
- Sedentary lifestyle.
— Congenital abnormalities of joint development.
— Injuries during sports activities with damage to the ligamentous apparatus.
- Fractures inside the joints.
- Obesity.
General information
An acetabulum fracture is a complex injury, accounting for 15-16% of the total number of pelvic bone fractures. The acetabulum is involved in the formation of the hip joint, so damage to this area often causes the development of severe post-traumatic coxarthrosis. A prerequisite for a successful outcome is the accurate restoration of the anatomical configuration of the acetabulum and reliable fixation of fragments. Treatment is carried out by traumatologists.
Acetabular fracture
Treatment of arthrosis of the hip joint, sclerosis
Therapy includes:
- Massage.
— Exercises (spreading bent legs while lying on your back).
— Physiotherapy (ozokerite, magnetic therapy).
— Taking special baths with radon and hydrogen sulfide.
— Treatment of the problem with non-steroidal anti-inflammatory drugs “Diclofenac”, “Nimesulide”, etc.
Lifting heavy objects should also be limited and sitting for long periods of time is prohibited. Jumping and running are also prohibited.
Otto's disease
This disease is otherwise called “acetabular dysplasia.” And this pathology received the name Otto’s disease after the name of the author who first described it back in 1824. This is a congenital disease that is observed exclusively in women. The problem manifests itself in limited movements in the hip joints (abduction, adduction, rotation, shortening of the lower extremities). At the same time, representatives of the fair sex do not feel any pain.
To confirm the diagnosis of socket dysplasia, it is necessary to conduct an examination:
— X-ray of the hip joint in the required projections.
- MRI.
- Ultrasound.
Ilioinguinal approach
Surgical treatment of fractures of such a depression as the acetabulum is a rather difficult task. The fact is that it is very difficult for a specialist to reach the site of damage.
— Front access.
- Ilioinguinal tract.
— Rear access.
It is used to open the anterior and inner surface of the acetabulum. It can also be used for immediate fixation of socket fractures and ruptures of the sacroiliac joint. However, this method of access does not allow the specialist to control the posterior column and wall of the cavity.
Pathological processes occurring in the hip joint consist, on the one hand, in changes in the properties of cartilage, and on the other, in mechanical disorders. Let's consider diseases associated with the pelvic bone.
Fracture
Often injuries to the pelvic bones are observed in road accidents or falls. Fractures are divided into simple and complex. After a fracture, the victim experiences severe pain and cannot move the injured leg. Shortening and pathological rotation of the lower limb are also noted.
The diagnosis is made on the basis of x-rays and computed tomography. The photo clearly shows the location and nature of the fracture and the presence of fragments.
Attention! An acetabular fracture requires immediate hospitalization. First aid is to ensure a horizontal position and rest for the victim, give pain relief, and wait for the ambulance to arrive.
To treat such conditions, skeletal traction and surgery are necessary. Injuries to the acetabulum can lead to partial or complete loss of mobility, permanent lameness, shortening of the limb, and the development of coxarthrosis.
Hip dislocation
With excessive load on the joint, uncomfortable positioning of the legs when running, jumping and other movements, conditions such as subluxation and dislocation of the hip are observed. In this case, the head of the femur is displaced, which leads to jamming of the entire joint and the impossibility of making movements in it.
Protrusion
Protrusion of the acetabulum is the pushing of its bottom by the head of the femur into the pelvic cavity. Protrusion can occur as a result of rickets, coxarthrosis, and osteoporosis of the elderly. As a result of bone friction, cartilage tissue is destroyed and arthrosis is formed.
In adolescents, pressing is treated with physiotherapy, traction and therapeutic exercises; in adults, operations are performed - arthroplasty, resection of the head or neck of the femur, osteotomy, endoprosthetics.
Impingement syndrome
Femoral-acetabular impingement syndrome (impingement syndrome) is one of the anomalies of the hip joint. When it occurs, a collision occurs between part of the femur and the edge of the acetabulum during movement.
If a tubercle appears on the neck of the femur, or if the edge of the acetabulum and its lip are uneven and thickened, then these tubercles or thickenings will collide during movements in the joint. In this case, a vicious circle will arise: the impacting formations will become inflamed during movement, swell, become even larger in size and collide even more strongly. Treatment is carried out surgically.
Coxarthrosis
Coxarthrosis is a degenerative-dystrophic disease. Primary coxarthrosis appears due to overload of the hip joints, and it especially often affects overweight people. The secondary form often develops against the background of hip dysplasia and frequent hip dislocations.
These conditions lead to the destruction of cartilage tissue. Friction of bone on bone causes aseptic (non-infectious) inflammation. First, pain appears in the hip joint when walking, then crunching, lameness and limitation of movements. If conservative therapy is ineffective, endoprosthetics surgery is performed.
Hip replacement
Fracture with complications
Displacement of the acetabulum can occur when a large object falls onto the pelvis, is compressed in the frontal plane, or, for example, in a car accident.
With such complicated fractures, the contours of the hip joint are disrupted. In posterior dislocations, the greater trochanter moves forward. If the dislocation is central, then the trochanter sinks deeper. To understand that the fracture is displaced, it is necessary to take an x-ray in two projections, since the problem can be in both the anterior and posterior directions.
Symptoms of complications:
- Active leg movements are sharply limited.
— The affected lower limb is in a vicious position.
Treatment in this case is as follows:
— Application of a skeletal traction system. The pin is passed behind the supracondylar region of the femur with a traction of 4 kg.
— The leg is placed in a position of flexion and adduction at the hip and knee joints.
— To determine the head into the desired position, specialists perform traction along the cervical axis using a loop or skeletal traction with an initial load of 4 kg.
— After reduction, the weights are transferred to the skeletal rod, leaving the original weight along the cervical axis.
— The leg is abducted to an angle of 95 degrees within 1 week.
The duration of traction is from 8 to 10 weeks. After another 2 weeks, movements in the joint are allowed. Full weight bearing on the leg is allowed only after six months. And ability to work is restored after 7 months.
Causes
Trauma usually occurs as a result of road traffic accidents, less often as a result of falls from a height, which causes a high incidence of combined injuries. Fractures of the acetabulum are often combined with dislocation of the hip joint, fractures of the neck or head of the femur. Injuries to other areas of the pelvis (including disruption of the continuity of the pelvic ring), fractures of the limbs, fractures of the ribs, injuries to the chest, head injury, blunt trauma to the abdomen, kidney damage and rupture of the bladder are also possible.
Coxarthrosis
This is a dystrophic disease that affects elderly and middle-aged people. The disease develops gradually over several years.
Signs of coxarthrosis are:
— Pathological relationship between the head of the femur and the glenoid cavity.
— The medial quadrant of the head is located laterally.
— The roof of the acetabulum hangs tiled over the fossa, resembling a beak.
— The length of the hole and the roof is disrupted.
— The cortical layer in the roof of the depression is thickened.
Coxarthrosis is accompanied by pain and limitation of movements in the joint.
In later stages of the disease, atrophy of the thigh muscles is observed.
The causes of this disease are divided into 2 types:
- Primary coxarthrosis. It occurs for reasons unknown to medicine.
- Secondary coxarthrosis. It is discovered due to other ailments.
The latter type of disease can result from problems such as:
— Congenital dislocation of the hip.
— Hip dysplasia.
— Aseptic necrosis of the femoral head.
- Arthritis of the hip joint.
- Perthes disease.
— Previous injuries (fracture of the femoral neck, pelvis, dislocations).
The course of coxarthrosis is progressive. If you start treatment at an early stage, then you can get by with conservative therapy. At a later stage, only surgical intervention will be an effective method.
Ligamentous apparatus
The acetabulum, due to its specific shape, provides the ability to move in several planes at once. But in order to hold the head of the femur in the joint, bone formations are not enough. Therefore, ligaments exist to stabilize the joint. Anatomists distinguish five paired connective tissue cords:
- ligament of the femoral head;
- ischiofemoral ligament;
- iliofemoral;
- pubofemoral;
- circular.
As you can see, the ligaments stretch from the joint to each pelvic bone separately, in addition, a thick layer of tissue holds the bones in a circular pattern. This design allows you to minimize the risk of injury when walking or running. In addition to ligaments, muscles are needed to move a joint. The main work is performed by the anterior and posterior thigh muscles.
Treatment of coxarthrosis
Orthopedists treat this disease. The choice of treatment method depends on the stage of the disease.
1. At stages 1 and 2, the following therapy is prescribed:
— Taking anti-inflammatory drugs. True, they are not used for a long time, since they can have a negative effect on internal organs.
- Use of chondroprotectors (medicines such as Arteparon, Rumalon, Chondroitin, Structum.)
- Vasoconstrictor drugs (Trental, Cinnarizine).
- Medicines to relax muscles.
— Intra-articular injections using hormonal agents, for example, Kenalog, Hydrocortisone.
- Use of warming ointments.
— Passage of physiotherapeutic procedures (laser, phototherapy, UHF, magnetic therapy), as well as massages, special gymnastics.
2. At stage 3, the only way to get rid of coxarthrosis is surgery. The patient has the destroyed joint replaced with an endoprosthesis. The operation is performed under general anesthesia as planned. The sutures are removed on the 10th day, after which the patient is sent for outpatient treatment. Rehabilitation measures after surgery are a necessity. In almost 100% of cases, joint replacement surgery provides complete restoration of function of the injured leg. At the same time, a person can then work, move actively and even play sports. He can wear a prosthesis for up to 20 years if he follows all the doctor’s recommendations. After this long period, a repeat operation is necessary to replace the already worn-out endoprosthesis.
Acetabular labral tears
The socket of the hip joint is formed by the pelvic bone and is called the acetabulum. Along the edge of the cavity is the acetabulum , a fibrocartilaginous formation. It increases the depth of the socket by 30%, increasing the contact area of the femoral head and acetabulum and thus promoting joint stability. But the main function of the acetabular labrum is the synthesis of synovial (articular) fluid, which evenly lubricates the articular cartilage of the femoral head and nourishes it. By creating a suction effect, the acetabular lip strengthens the hip joint. In addition, the acetabular labrum contains nerves that determine the position of the femoral head in space. You can read more about the anatomy of the hip joint in the general article on the causes of pain in the hip joint.
The structure of the hip joint: in order to show the acetabular labrum, the head of the femur in the picture is “dislocated” from the joint
Transverse section of the hip joint: the acetabular labrum, bordering the acetabulum, increases the area of contact with the head of the femur
The acetabular labrum, being a soft tissue structure, can rupture. Most often, tears of the acetabular labrum occur in athletes. Ruptures can be traumatic, i.e. occurring against the background of relatively severe trauma, or dystrophic (degenerative), which occur against the background of chronic trauma. Dystrophic tears are common in ballet, as well as in sports that require strong hip flexion (football, mountaineering) or frequent hip rotation (golf, figure skating, martial arts).
A torn acetabular labrum causes mechanical obstacles to movement in the hip joint, which is manifested by pain in the groin or buttock, with an arc enveloping the hip joint from the outside. The pain is often accompanied by clicking or a sensation of obstruction in the hip joint. It is worth noting that not all pain or clicking in the hip joint is a sign of a labral tear: many other injuries and diseases can cause pain in the hip joint.
The abnormal structure of the hip joint (dysplasia, femoroacetabular impingement syndrome) predisposes to dystrophic ruptures. For example, with hip dysplasia, the acetabular labrum is hypertrophied (increased in size) and prone to tears. Femoral-acetabular impingement syndrome is characterized by persistent trauma to the acetabular labrum, which leads to its degeneration and ultimately to rupture.
Acetabular labral tears are similar to knee meniscus tears, but are much less common in comparison. The relative rarity of acetabular labrum ruptures is determined by the fact that many doctors do not even know about the existence of such a condition. However, this is not surprising, since tears of the acetabular labrum occur mainly in athletes and only a doctor who treats athletes can know about such an injury. On the other hand, it is possible that tears of the acetabular labrum are very common in ordinary people, and progress in diagnostics, in particular, the spread of magnetic resonance imaging, will make it possible to identify this problem not only in athletes.
There are two main types of labral tear: flap and marginal avulsion. In both the first and second cases, the damaged area ceases to perform its function, the dangling fragment of the acetabulum interferes with movements, is pinched in the joint, which, as we have already noted, is manifested by pain and possible clicking noises during movements. The insidiousness of ruptures of the acetabular labrum is that the dangling fragment also damages the adjacent cartilage covering the head of the femur, which leads to its chondromalacia (gradual thinning and abrasion). It is possible that chondromalacia, in turn, can cause a more serious condition - arthrosis of the hip joint (coxarthrosis), but scientists do not yet have a common point of view on this matter. Since the acetabulum borders the acetabulum along its circumference (with the exception of the area at the bottom of the acetabulum), tears can occur in different places. There are tears in the anterior, superior and posterior parts of the acetabular labrum.
The main types of acetabular labral tears. On the left - a normal acetabular labrum, in the center - a flap gap, on the right - a tear along the edge like a “watering can handle”
Detachment of the acetabular lip along the edge like a “watering can handle”
A loose fragment of the acetabular labrum damages the adjacent cartilage covering the head of the femur, leading to chondromalacia and arthrosis of the hip joint.
Diagnosis
Pain from a labral tear is usually felt in the groin or upper thigh. Often, patients, showing a sore spot, clasp the thigh with their thumb and forefinger in front and outside of the hip joint so that these two fingers form the contours of the letter C. Pain can also be felt behind the hip joint, in the gluteal region. It is possible that anterior tears tend to present with pain in front of the joint (in the groin), and posterior tears tend to present with pain behind the joint (in the gluteal region).
Pain from a labral tear is often accompanied by mechanical symptoms: clicking or a sensation of obstruction in the joint. As with other diseases of the hip joint, pain can radiate down the leg, usually along the front leg, less often along the inner surface of the thigh to the knee.
The pain can be of different nature and range from mild, dull, provoked by physical activity and passing during rest, to severe and constant, seriously limiting daily activities. Few patients have a significant limp or require crutches, but they try to avoid certain positions and movements (mainly hip flexion, abduction, and rotation) that cause pain.
Traumatic labrum rupture is primarily caused by an external force applied to a fully extended and externally rotated hip. Often the patient can point to a specific injury, such as a fall or twisted ankle, that preceded the onset of pain. The diagnosis of a labral tear often goes unrecognized, and people try to be treated for a “groin sprain” that actually turns out to be a labral tear.
Less commonly, the disease develops gradually, due to chronic trauma, which leads to degeneration of the acetabular lip and ultimately to its rupture. In this case, the patient cannot definitely indicate the time of onset of pain, cannot indicate the fact of injury.
An examination by a doctor can usually distinguish a labral tear from the internal type of snapping hip syndrome. The patient is placed on his back and his sore leg is bent, bringing the thigh into a position of flexion, adduction and internal rotation; the pain of this movement indicates a tear of the acetabular labrum.
There is also a special test that helps determine a labral tear. It was suggested by Joseph McCarthy. The patient is placed on his back with his legs bent to fix the pelvis, after which the affected leg is extended, rotating the thigh outward, and then the same movement is repeated, rotating the thigh inward. When a painful click appears, the test is considered positive and indicates a tear of the acetabular labrum. A tear in the acetabular labrum may also be indicated by pain in the groin when lifting a straight leg against the doctor’s resistance, but this is too nonspecific a sign that can also appear with other diseases of the hip joint.
To confirm or exclude a complex diagnosis of acetabular labral tear, additional research methods are required. A traditional plain radiograph of the pelvis and hip joints (to compare the hip joint of the diseased and healthy leg) and a radiograph of the affected hip joint in the position of hip flexion and abduction (in the so-called frog position) with a labral tear are normal. They may show hip dysplasia, which may contribute to a labral tear.
With old ruptures, there may be changes in the bone - subchondral cysts, which indicate chondromalacia or detachment of the acetabular lip from the articular cartilage. These cysts are most often located in the upper outer part of the acetabulum.
Femoral-acetabular impingement syndrome (impingement syndrome) is one of the anomalies of the hip joint, accompanied by dystrophy and tears of the acetabular labrum. Its most characteristic radiological sign is the so-called pistol grip sign, that is, flattening of the anterosuperior part of the femoral neck, which is why it appears abnormally convex and, together with the femoral head, resembles a pistol grip. Bone cysts may be visible in this convex part of the neck. A Mayo Clinic study found that 87% of patients with acetabular labral tears had at least one abnormality on radiographs. This study included all patients with acetabular labral tears seen in the clinic over a 6-year period and was not limited to sports-related injuries.
Computed tomography and bone scintigraphy are usually uninformative.
Perhaps the most accurate research method to detect a tear in the acetabular labrum is magnetic resonance imaging . However, unfortunately, magnetic resonance imaging also gives a high percentage of false negative results (i.e. the tomogram turns out to be normal when the labral tear is actually There is). Therefore, in any case, the importance of a doctor’s examination should not be diminished, and only those findings on magnetic resonance imaging that correlate with clinical signs are significant, i.e. those features that the doctor reveals during examination.
Magnetic resonance imaging showing a tear of the acetabular labrum in its upper part (the red arrow indicates the fragmented nature of the acetabular labrum, its irregular shape). On this tomogram, the acetabular labrum shows dark colored areas.
For differential diagnosis of pain in the hip joint, a local anesthetic (Novocaine, Libocaine, etc.) can be injected into the joint under fluoroscopy control: temporary pain relief after this procedure indicates intra-articular pathology.
An accurate diagnosis can be made through arthroscopy - an operation in which an arthroscope (video camera) is inserted into the joint cavity through an incision, or rather a puncture, about one centimeter long, which allows you to examine the joint from the inside and finally make sure of the exact diagnosis.
The main methods for diagnosing intra-articular pathology of the hip joint remain questioning and examination by a doctor - in comparison with arthroscopy (as a diagnostic standard), they allow a correct diagnosis to be made in 98% of cases. By comparison, magnetic resonance imaging produces false negatives in 42% of cases and false positives in 10% of cases. However, such high numbers of errors in magnetic resonance imaging may be due to incorrect interpretation of images by radiology doctors, who are not always familiar with acetabular labral tears. Pain relief in response to the injection of a local anesthetic into the hip joint indicates intra-articular pathology with 90% reliability, however, this test is not specific to acetabular labral tears, but covers all diseases of the hip joint, which once again emphasizes the importance of a competent examination by a doctor.
Treatment
Conservative treatment. A rupture of the acetabular labrum usually cannot be treated conservatively - it has virtually no blood supply in people over 20 years of age and therefore the ruptures do not heal on their own. Therapeutic exercise can relieve muscle spasms and correct gait, and non-steroidal anti-inflammatory drugs reduce inflammation and, to a certain extent, alleviate the symptoms of pain, but neither physical therapy nor non-steroidal anti-inflammatory drugs can eliminate the source of inflammation and completely relieve the patient of symptoms. However, the geometry of the fracture is also important. If the gap is small, then it will not cause a cascade of intra-articular disorders (choronromalacia and, then, arthrosis of the hip joint). With small ruptures, self-adaptation of the joint is possible. Sometimes athletes with constant severe pain in the hip joint due to tears of the acetabular labrum, indicating inflammation of the joint, are injected into the joint with glucocorticoids (hydrocortisone, diprospan), however, as a rule, this gives only a temporary result. If the tear of the acetabular labrum is large enough, then complete recovery is possible only through surgery - arthroscopy of the hip joint.
Surgery. Unfortunately, surgical treatment of acetabular labral tears produces less predictable results than treatment of knee meniscus tears. Hip arthroscopy allows the doctor to see the labral tear and thereby confirm the diagnosis. The goal of the operation is to remove or reattach the torn portion of the lip that is loose in the joint cavity and causing symptoms, while preserving the remaining portion of the intact lip as best as possible. During arthroscopy, you can also examine other structures that can cause pain and clicking in the joint (articular cartilage of the acetabulum and femoral head, ligament of the femoral head, and joint capsule). During the operation, the torn part of the acetabular labrum is removed, thereby eliminating the mechanical cause of the pain. In some rare cases where there is extensive marginal acetabular labral avulsion, arthroscopic suture of the avulsed acetabular labrum may be performed. This operation is performed on the same principle as the Bankart operation for habitual dislocation of the shoulder joint.
Arthroscopy of the hip joint: a video camera (arthroscope) is inserted into the joint cavity through a 1-centimeter incision, which allows you to examine the joint from the inside and see all the damage. A tear of the acetabular labrum is shown; a fragment of the labrum is pinched between the head of the femur and the acetabulum
Arthroscopic suture of the torn acetabular labrum is carried out according to the same principle as the Bankart operation for habitual dislocation of the shoulder joint
Complications
There is no reliable information in the published scientific literature regarding the consequences of acetabular labral tears, and the risk of developing severe osteoarthritis of the hip joint after them is unknown. However, a detrimental effect of a labral tear on the cartilage covering the femoral head cannot be ruled out. For this reason, surgical treatment is recommended only for athletes whose pain and decreased mobility in the hip joint are so severe that they interfere with successful sports activities. The mere presence of an acetabular labral tear on magnetic resonance imaging should not be an indication for surgery.
The complications of hip arthroscopy are the same as those of any operation performed under general anesthesia. In addition, there may be iatrogenic damage to the acetabular labrum or articular cartilage, breakage of endoscopic instruments during surgery, traction injury to the nerves of the leg (as the leg must be extended during arthroscopy), or direct damage to the sciatic nerve or lateral femoral cutaneous nerve during placement of trocars (devices in which a video camera and instruments are inserted into the joint cavity).
Forecast
The results of arthroscopic treatment of single traumatic ruptures of the acetabular labrum are very good: 80-90% of patients experience a complete recovery, after which they can return to professional sports. Even after a successful operation, clicking in the joint (especially in certain positions) may remain, which should be warned about in advance.
With dystrophic tears caused by frequent repetition of movements traumatic for the joint, the prognosis for returning to sports is quite poor, especially if chondromalacia (softening of the cartilage, its abrasion) is detected during arthroscopy.
For some time after arthroscopy (from 2 days to 2 weeks), the patient is prohibited from leaning on the operated leg. In the first 2-6 weeks after surgery, physical therapy is carried out aimed at developing the joint, and after 6-12 weeks it is usually possible to resume training.
The literature provides very little information regarding the prognosis of arthroscopic operations in patients with bone anomalies of the hip joint. In cases of severe hip dysplasia, acetabular retroversion, or femoroacetabular impingement syndrome, symptoms should be expected to persist. Surgical treatments for these anomalies have been described, including supracetabular osteotomy and femoral neck osteoplasty, which requires trochanteric osteotomy and dislocation of the femur from the hip joint during surgery. The same dislocation of the femur allows access to and repair of complex tears of the trochanteric labrum like a watering can handle.
Prevention
The best way to prevent it is to avoid movements that cause the femoral neck to strike the acetabular labrum. This, of course, is impossible in those sports that involve swinging movements of the legs or strong rotation of the hip, in particular in golf, figure skating, martial arts, dance sports and artistic or rhythmic gymnastics.
Acetabular labral tears often occur in poorly trained athletes during leg swing movements, for example, in high school dancers performing a step jump, or in athletes who press heavy loads with their legs without a full warm-up. The correct organization of the training process can prevent such gaps.
Many female athletes experience acetabular dysplasia, accompanied by increased mobility of the hip joint. This helps gymnasts and ballerinas in their activities, but it also reduces hip stability and predisposes to labral tears. Tears of the acetabular labrum are often associated with osteoarthritis of the hip joint, especially developing against the background of hip dysplasia, and femoroacetabular impingement syndrome.
Materials used when writing this article:
Byrd JW, Jones KS: Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med 2004;32(7):1668.
O'Leary JA et al: The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy 2001;17(2):181:
Siebenrock KAet al: Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop 2004;Feb(418):54.
Wenger DE et al: Acetabular labral tears rarely occur in the absence of bone abnormalities. Clin Orthop 2004;Sep(426):145.
| The author of the article is Candidate of Medical Sciences Sereda Andrey Petrovich |
Complications of an acetabulum fracture
Problems, by the way, are rare, but people should still be aware of them. Postoperative complications include:
- Sepsis.
- Suppuration of wounds.
- Thromboembolism.
- Nerve damage.
— Aseptic necrosis of the femoral head or the wall of the acetabulum.
— Paralysis of the gluteus minimus and medius muscles.
To prevent such complications from occurring, many doctors immediately offer their patients endoprosthetics.