Classification of the disease, diagnosis and main symptoms
Traumatology specialists use a classification of injuries due to chondromalacia of the femoral and tibial condyles, based on the degree of destruction of cartilaginous tissue:
- the first degree is characterized by the initial stages of softening of the cartilage layer in the presence of swelling;
- the second degree is characterized by cracking of the chondral tissue and the occurrence of delamination of the cartilaginous plane, while a small area of cartilaginous tissue is affected;
- the third degree implies a process of cracking and separation into layers of an intense nature, while the affected area increases;
- the fourth degree implies destruction down to bone formations in combination with the development of a complex cartilaginous defect.
With violations of this type, the following symptoms are observed:
- manifestation of pain in aching or acute stages;
- manifestations of crunching when performing various movements;
- formation of blockade of the articular joint;
- manifestation of joint swelling;
- impaired mobility of the joint;
- joint instability.
In modern medical practice, the main diagnostic method is arthroscopic examination, characterized by examination of the joint cavity using an endoscope. MRI and X-ray examinations are also used.
Tibial condyle fracture
First aid involves immobilizing the limb with a splint from the foot to the upper third of the thigh and urgently transporting the victim to a medical facility. Treatment of this pathology is carried out in a trauma department. Upon admission, the traumatologist performs a puncture of the knee joint and administers novocaine to anesthetize the fracture. Further tactics are determined taking into account the characteristics of the injury.
Conservative treatment
For incomplete fractures, tibial fractures, and non-displaced marginal fractures, the treatment plan involves applying a plaster cast for 6-8 weeks. Analgesics, walking on crutches, and elevated limb position during rest periods are prescribed. The patient is referred for UHF and exercise therapy. After stopping immobilization, it is recommended to continue using crutches and not lean on the limb for 3 months from the date of injury.
For displaced fractures, depending on the type of damage to the tibia, treatment includes simultaneous manual reduction followed by traction or traction without previous reduction. The presence of slight displacement allows the use of adhesive traction. In case of a fracture of one condyle or both condyles with significant displacement, a fracture of one condyle with subluxation or dislocation of the other condyle, skeletal traction is applied.
Traction is usually maintained for 6 weeks, during which time exercise therapy is performed. Then the traction is removed, and the patient is recommended to walk on crutches without supporting his leg. A distinctive feature of intra-articular fractures of the upper tibia is delayed healing, so light weight bearing on the leg is allowed only after 2 months, and full support after 4-6 months.
Surgery
Indications for surgical treatment are an unsuccessful attempt to reduce fragments, pronounced compression of fragments, entrapment of a fragment in the articular cavity, compression of blood vessels or nerves, and a displaced fracture of the intercondylar eminence of the tibia when closed reduction is unsuccessful. Operations are performed as planned a few days after admission.
Since the use of skeletal traction in a significant number of cases does not allow for accurate comparison of fragments, the list of indications for surgery is currently expanding. Specialists in the field of traumatology and orthopedics are increasingly offering patients surgical treatment not only for the injuries listed above, but also for any condylar fractures with fairly pronounced displacement of the fragments.
- For ordinary fresh injuries, an arthrotomy is performed. Fragments lying freely in the joint cavity are removed. Large fragments are reduced and fixed with a screw, and intramedullary or extraosseous osteosynthesis is performed with a nail, knitting needles, or special L- and T-shaped support plates.
- For multi-fragmented injuries of the tibia and open fractures, external osteosynthesis is performed using the Ilizarov apparatus.
- For fresh fractures with significant compression, unresolved and old fractures, as well as secondary subsidence of the condyles due to premature load on the leg, osteoplastic surgery according to Sitenko is performed.
According to the Sitenko method, the joint is opened, an osteotomy is performed, the upper fragment of the condyle is raised so that its articular surface is located at the same level and in the same plane with the surface of the second condyle, and then a wedge made of autogenous or heterogeneous bone is inserted into the resulting gap. The fragments are fastened with tightening screws and a plate. After osteosynthesis, the wound is sutured layer by layer and drained. With stable fixation, immobilization in the postoperative period is not required.
The drainage is removed for 3-4 days, then physical therapy with passive movements is started to prevent the development of post-traumatic joint contracture. Postoperative treatment includes painkillers, antibiotics, thermal procedures (ozokerite, paraffin). After the pain has reduced, they move on to active development of the joint. Light axial load on the limb with conventional osteosynthesis is allowed after 3-3.5 months, when performing bone grafting - after 3.5-4 months. Full support on the leg is possible after 4-4.5 months.
Osteochondrosis dissecans and osteochondral fractures[edit | edit code]
Osteochondrosis dissecans is a lesion of cartilage and underlying bone, leading to the formation of an osteochondral fragment (sometimes mobile) without obvious trauma. The classic location of the lesion is the outer surface of the medial condyle of the femur (51-85% of all cases). Osteochondrosis dissecans can also affect the articular surface of the medial condyle, lateral condyle and patella.
The juvenile form of the disease occurs in early adolescence, when the growth plates are still wide open, the teenage form - a little later, with greater skeletal maturity. Boys are affected almost twice as often as girls. Bilateral changes are observed in 25% of cases, but usually the lesion is not symmetrical or synchronous. The causes of osteochondrosis dissecans are still unclear. Previously, it was believed that the process was based on inflammation of the cartilage adjacent to the bone, and the disease was called osteochondritis. However, this theory was not confirmed. Currently, there are the following assumptions about the etiology of osteochondrosis dissecans.
- Chronic trauma to the outer edge of the medial condyle in contact with the intercondylar eminence of the tibia.
- Contact of the medial articular surface of the patella with the outer
edge of the medial condyle with the knee joint in full flexion. *Impaired blood supply to the subchondral bone.
- Local epiphyseal chondrodysplasia.
Cases of the disease have been reported in several family members, which may indicate a hereditary predisposition. The cause of an osteochondral fracture is acute trauma. The fracture may involve the lateral and medial condyles of the femur and the patella. Osteochondral fracture of the lateral condyle is often associated with patellar dislocation.
Rehabilitation and return to sports[edit | edit code]
It is quite difficult to predict the timing of rehabilitation. Since an osteochondral fracture occurs in an unchanged bone, the patient may well return to previous loads 3-4 months after surgery.
With osteochondrosis dissecans, the timing is not so clear - fragmentation occurs in pathologically altered tissues, which worsens the prognosis. A fragment fixed to the changed bone may not take root. A previously stable and asymptomatic fragment may suddenly detach after skeletal maturation. There is no reliable way to monitor healing. In this regard, there are no uniform recommendations regarding the timing of returning to previous loads.
Subchondral sclerosis of the hip joint
Subchondral sclerosis of the hip joint is manifested by stiffness of movement in the morning. Patients are concerned about pain in the lower back and pelvis, which worsens at night and when walking. The functioning of the intestines and genitourinary organs may be disrupted, a feeling of difficulty in breathing, chest pain and tachycardia may appear. Over time, lameness occurs; the patient cannot do without a cane, and then without a wheelchair.
If you have signs of illness, call. At the Yusupov Hospital, they treat not the manifestation, but the underlying pathology. To reduce pain, doctors prescribe analgesics, anti-inflammatory drugs and physiotherapeutic procedures. The condition of tissues is improved with the help of medications containing chondroitin and glucosamine. Joint mobility is partially restored with the help of manual therapy, exercise therapy, massage and swimming. The integrated approach used at the Yusupov Hospital will help improve the patient’s quality of life.
Treatment[edit | edit code]
Conservative treatment[edit | edit code]
Views on the treatment of osteochondrosis dissecans are as contradictory as on its etiology: in other words, there is no generally accepted treatment tactics. It is recommended to avoid significant physical activity and spare the affected leg - do not lean on it for several weeks, that is, until the symptoms disappear. Movements in the knee joint are allowed. The question of when to limit physical activity has not yet been resolved. For very active patients, the joint can be immobilized briefly with an orthopedic device or even a plaster cast.
The duration of conservative treatment is determined by the doctor, based on his preferences and experience. The literature often provides evidence that, against the background of load limitation, the defect heals spontaneously in half of the cases. In one study that followed arthroscopy for an average of 7.5 years, seven out of ten previously stable osteochondrosis lesions became unstable during the follow-up period.
The following are factors that reduce the likelihood of successful conservative treatment.
- Older age.
- Large transverse size of the lesion.
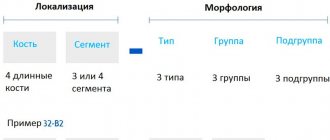
- Foci in the area of increased load (segment 2 according to Cahill in the image in a direct projection).
- Foci between 30-60° - between Blumenzaat's line and the continuation of the posterior contour of the femoral body (segment B according to Cahill on the lateral image).
Surgical treatment[edit | edit code]
Indications
- Juvenile osteochondrosis dissecans, not amenable to conservative treatment for 6-12 months.
- Separation of a previously stable fragment.
- Signs of a joint mouse.
- Estimated closure of the growth zone in the next 12 months.
- Clinical signs of nonunion confirmed by scintigraphy or MRI.
Methods
- Simple excision or removal of the separated fragment (not recommended except for very small
damage in non-load bearing areas).
- "Refreshment" and expansion of the crater.
- Microfractures.
- Fixation of the fragment with metal pins (weak), screws (countersunk microscrews from the set for fixation of facial bones, cannulated screws with a diameter of 3.5 mm or 2.4 mm, Herbert compression screws), absorbable darts, knitting needles and screws, bone pins.
- Subchondral retrograde bone grafting.
- Autotransplantation of osteochondral rods (mosaic arthroplasty).
- Osteochondral allografts.
- Implantation of a culture of own chondrocytes.
Complaints and physical signs[edit | edit code]
- No history of trauma.
- Symptoms are usually not acute and are associated with physical activity.
- Pain.
- Edema.
- Block of the knee joint.
- Signs of a joint mouse.
- Pain on palpation of the femoral condyle.
- Positive Wilson test.
Radiation diagnostics[edit | edit code]
The true severity of osteochondrosis dissecans or osteochondral fracture can be assessed radiographically. To identify lesions of typical localization, a tunnel image is best suited. Valuable additional information about the position of bone fragments and the defect is provided by radiographs in direct, lateral and axial projections.
MRI is particularly good at distinguishing between stable and unstable lesions and less so for surveillance. Unstable lesions have the following features on T2 imaging.
- Signal amplification below the osteochondrosis zone.
- Linear signal amplification directed perpendicular to the bone to the affected area.
- Articular cartilage defect > 5 mm.
- A fluid-filled cyst measuring 5 mm below the affected area.
Diagnostics
The main diagnostic measures are X-ray examination and magnetic resonance layer-by-layer scanning. An informative method is arthroscopy, which involves working in the articular cavity using a special endoscope instrument and high-precision magnification methods. Be sure to use high-quality anesthesia and appropriate preparation, which allows you to carry out the procedure effectively and even perform intra-articular administration of drugs for therapeutic purposes.