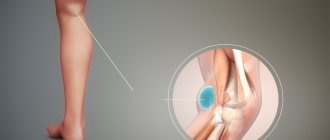
A Baker's cyst is a fluid-filled synovial cyst located in the popliteal fossa. This formation is a benign cystic tumor and originates from synovial tissue. It can also occur in the wrist, hand, and foot areas.
The cyst can put pressure on some anatomical structures, in most cases the popliteal vein is affected, which can result in thrombophlebitis.
Clinically Relevant Anatomy
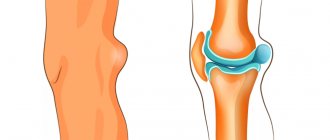
A Baker's cyst is an enlarged bursa located between the medial head of the gastrocnemius muscle and the capsular counterpart of the semimembranosus muscle, the oblique popliteal ligament.
For the formation of a cyst, two conditions must be met - anatomical connection and chronic joint effusion. Joint effusion in the knee can fill the gastrocnemius and semimembranosus bursae with synovial fluid and, if fluid drainage is obstructed by a unidirectional mechanism, the gastrocnemius and semimembranosus bursa enlarges, creating a pseudocystic cavity called a Baker's cyst.
What are the symptoms of a Baker's cyst?
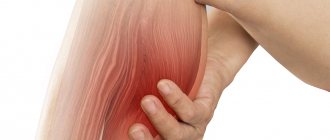
The danger of the disease lies in the fact that in the initial stages it does not manifest itself in any way. As the hernia develops, pain begins to appear. At first, the pain may only bother you during physical activity or long-term walking. A constant feeling of discomfort occurs when the bag is almost completely filled with liquid. In this case, the capsule begins to irritate the nerve structures of the knee joint, causing severe attacks of aching pain. Along with pain, the following symptoms are observed:
- inability to fully bend the knee;
- swelling of the leg;
- tingling in the affected area;
- decreased physical activity;
- numbness of soft tissues.
In advanced cases, the knee and lower leg can swell greatly, and the slightest movement brings acute pain. That is why it is very important to seek specialized help in a timely manner (even at the stage of the appearance of a small ball in the knee cavity) before obvious symptoms of joint damage appear.
Epidemiology/Etiology
A Baker's cyst or popliteal cyst forms when there is an underlying problem with the knee joint, accompanied by an inflammatory reaction, which occurs as a result of the formation of intra-articular bodies in the presence of osteoarthritis, rheumatoid arthritis, rupture of the anterior cruciate ligament or meniscus, or because As a result of knee arthroplasty, particles appear, mainly from the polyethylene liner.
- A primary cyst is a formation not associated with pathology of the knee joint.
- A secondary cyst is a stretch of the synovial bursa located between the tendons of the gastrocnemius and semimembranosus muscles. The fluid enters through the channel through which the normal bursa is connected to the joint. This is the most common occurrence.
A cyst can vary in size from very small (asymptomatic) to large, but variation in size is very common. Especially in small cysts, there may be a septum separating the semimembranosus and gastrocnemius components. It can function as a valve, allowing fluid to enter the popliteal cyst and not leave it.
There are differences between popliteal cysts in children and adults. In children, these are cystic masses filled with gelatinous material that develop in the popliteal fossa. They are usually asymptomatic and are not associated with intra-articular pathology. Spontaneous resolution often occurs, although the process may take several years. In adults, Baker's cyst often occurs in combination with other intra-articular pathologies and inflammatory conditions.
What factors contribute to the appearance of a cyst?
Before identifying the reasons for the formation of a popliteal hernia, it is necessary to understand what a cyst is. On the back of the knee joint there is a so-called bursa, which in normal condition does not manifest itself in any way. But when an inflammatory process occurs, joint fluid begins to form faster than it can be absorbed.
Due to the anatomical structure of the knee, when it bends, excess fluid begins to be forced into the posterior sections, where it accumulates in the capsule. The longer the excessive secretion of synovial fluid occurs, the larger the hernia becomes.
The main reasons contributing to the development of cysts, experts include:
- knee injuries of varying severity;
- excessive and systematic stress on the legs;
- professional sports;
- overweight;
- damage to the cartilage tissue of the joints;
- meniscus pathology;
- osteoarthritis, arthritis, chronic synovitis.
Despite the fact that damage to the knee joint can occur at any age, older people are most often at risk, since age-related changes in the body negatively affect the general condition of the musculoskeletal system.
Clinical picture
Symptoms may include:
- Vague pain in the popliteal fossa.
- Swelling and formation of additional volume in the popliteal space.
- Tension in the area of swelling, which can change depending on physical activity.
- Limitations in the range of motion of the knee joint.
Most cysts are localized on the medial side of the popliteal fossa in the gastrocnemius-semimembranosus bursa. Also, a cyst can form in the popliteal bursa and then the protrusion will be located in the lateral part of the popliteal space. In addition, sometimes the popliteal cyst extends upward or anteriorly.
Cysts can range in size from small, clinically asymptomatic and non-palpable cysts, to large, space-occupying lesions that cause visible swelling in the popliteal area. The size of the cyst and the intensity of pain can lead to limited range of motion. In rare cases, there will be signs and symptoms of a meniscus tear, which can be checked with the McMurray test.
Popliteal cysts can put pressure on other anatomical structures. Compression of the popliteal artery or vein can cause ischemia or thrombosis, respectively, whereas compression of the tibial or peroneal nerves can cause peripheral neuropathy.
Symptoms
Benign skin tumors and tumor-like proliferations of skin tissue develop in most cases painlessly in the form of single or multiple nodes or growths. More often they are localized in the upper extremities, on the torso, and face. In most cases, the neoplasms are covered with skin with a normal color, less often - pink. There are formations with different colors from yellowish-brown to black-blue. The most common symptom is an unexpectedly palpable tumor, in second place are various kinds of pain that precede the appearance of the tumor, and in third place is the appearance of a painful tumor. The nature of the pain is usually moderate and intermittent; it is not as intense as with primary bone tumors, and most often manifests itself during functional loads or palpation of the tumor. When the tumor grows into the bone, the pain becomes constant, and when localized in the area of large nerve trunks, a picture of neuritis or plexitis may develop.
Differential diagnosis
Baker's cyst can be mistaken for several other knee pathologies. The patient's medical history, as well as clinical examination and imaging, allow for the correct diagnosis of the disease.
Conditions that are accompanied by the appearance of a space-occupying formation in the popliteal fossa/tibia
| Muscle strain or tear | Palpable formation/tenderness, swelling/hyperemia, pain when contracting and/or stretching the muscle. |
| Muscle contusion or hematoma | Local muscle damage accompanied by bleeding or swelling, painful muscle contraction/stretching. If the hematoma is old, an organized compaction develops. |
| Muscle spasm or cramp | Painful, palpable cord/thickening, possible limited range of motion, pain when stretching muscles. |
| Fascial tear with muscle hernia | Palpable soft formation, acute muscle pain with increased activity, local swelling after physical activity. |
| Myositis ossificans | Palpable painful tightness in the muscles, micro-tears in the muscle fibers that cause pain and swelling when the muscles contract or stretch, impaired movement due to limited muscle function. |
| Deep vein thrombosis | Constant pain, pain with passive dorsiflexion of the foot (Homan sign), local hyperemia, local tenderness on palpation of the calf and possible swelling, increased body temperature. |
| Benign tumor | Local pain and tenderness, possible palpation sensation of softness or stiffness of tissues, there may be a disturbance in movement (depending on the location). |
| Malignant tumor | Generalized malaise, possible sudden weight loss, localized pain and/or swelling of varying sizes and consistency. |
| Hemangioma | Present for a long time, slow changes in size over time, palpation - swelling, may be painful, may/may not limit movement. |
| Baker's cyst | Palpation reveals swelling with possible pain in the area of the popliteal fossa and the posterior inner part of the calf. |
| Rupture or enlargement of Baker's cyst (pseudothrombophlebitis) | Can simulate deep vein thrombosis, swelling in the lower leg, acute pain that intensifies with compression. |
A popliteal cyst may also be confused with a lipoma, which will present less pressure resistance compared to a Baker's cyst or aneurysm differentiated by ultrasound.
Differential diagnosis of compactions in the calf muscle
| Possible diagnosis | Supporting Evidence | Negative evidence |
| Old muscle strain or injury with scar tissue | Palpation - compaction | No history of muscle tear or injury, no pain when running |
| Fascial tear with muscle hernia | Pain when walking over a distance of more than 0.5 km, tenderness on palpation | No connection with injury, latent onset of the disease, no pain when running or performing basic exercises |
| Local muscle spasm | Pain when walking more than 0.5 km, noticeable soreness | No pain when passively stretching the calf, no pain when resisting muscle contraction, no limitation of motion in the foot or knee |
| Deep vein thrombosis | Palpable tenderness, pain when sitting cross-legged, family history of increased coagulation factor XII, oral contraceptive use | No history of deep vein thrombosis and recent immobilization, no edema, no elevated body temperature, negative Homan test, presence of pulsation at the site of injury |
| Benign tumor | Palpable induration, palpable pain, latent onset of the disease | Intermittent pain |
| Malignant tumor | Palpable induration, palpable pain, latent onset of the disease | No weight loss, no night pain or feeling unwell, intermittent pain, good general health |
| Hemangioma | Hidden onset, unknown cause, hormonal changes (oral contraceptives) present for a long time, slow change in size over time, palpable swelling, may be painful, not always accompanied by restriction of movement |
Accurate differentiation of a patient's symptoms can be achieved using ultrasound.
If a popliteal cyst becomes infected, it often results in a painful lump forming behind the knee. In such cases, it may be difficult to make a diagnosis, and an infected cyst may be mistaken for a neoplasm. The cyst may rupture (open up), causing severe pain in the calf, decreased ankle motion, and causing symptoms similar to deep vein thrombosis (seen on ultrasound or venogram).
You may be interested in the article: Prepatellar bursitis: causes, symptoms, treatment.
It is important to diagnose a ruptured Baker's cyst as early as possible to determine the best treatment and avoid complications such as compartment syndrome, and to differentiate it from the following conditions:
- thrombophlebitis;
- popliteal aneurysm;
- inflammatory arthritis;
- calf muscle strain;
- soft tissue swelling or muscle rupture.
It should be considered that swelling along the anterior surface of the proximal tibia in a patient with a previous history of ipsilateral total knee arthroplasty may be a consequence of a Baker's cyst.
Diagnostics
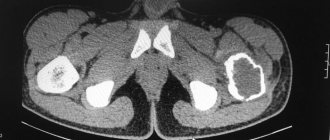
Evaluation of knees suspected of having popliteal cysts may include standard radiographs, arthrography, ultrasound, and MRI. Early in the diagnosis, it may be helpful to obtain plain radiographs to identify other conditions associated with popliteal cysts, such as osteoarthritis, inflammatory arthritis, and articular bodies (arthremphys). Additionally, loose articular bodies may be visible in a Baker's cyst on plain radiographs.
You can read about pain in the anterior knee joint here.
Direct arthrography was initially used to identify popliteal cysts. Direct arthrography involved intra-articular injection of gas or iodinated contrast medium followed by mobilization of the joint to enhance contrast in the cyst. Spot radiographs or fluoroscopy were then used to determine the presence of contrast in the cysts. Disadvantages of this method include the use of ionizing radiation and the use of invasive methods to administer contrast.
The advantages of ultrasound are its low cost, non-invasive use and absence of radiation. The main disadvantage is that it depends on the user (training of the researcher). Ultrasound is able to detect Baker's cysts in almost 100% of cases, but does not differentiate them from other pathological conditions such as meniscal cysts or myxoid tumors; it also does not detect other knee pathologies that are often associated with these cysts.
Magnetic resonance imaging remains the gold standard for diagnosing Baker's cysts and differentiating them from other conditions. It evaluates soft tissue abnormalities and has the added benefit of being accurate in diagnosing associated joint disorders, allowing the full spectrum of associated disorders to be assessed.
By
Treatment
Sometimes no treatment or simple supportive measures lead to spontaneous resolution or reduction of symptoms. If this does not happen, it may be worth using invasive and surgical instruments.
The asymptomatic condition often improves and over time, Baker's cyst disappears on its own. If the cyst is symptomatic, rest may ease the pain. You can also take non-steroidal anti-inflammatory drugs (NSAIDs) and ice to reduce pain.
If pain persists, steroids with an anesthetic solution may be recommended, which may relieve the pain but will not prevent the cyst from recurring. This is only a temporary solution. In the presence of a popliteal cyst of inflammatory origin, this is sufficient to treat the underlying disease. When the underlying disease is not treated, Baker's cyst may recur. Arthroscopic examination and treatment of all pathological conditions should be carried out before considering dissection of the popliteal cyst.
The cyst may be removed surgically if it becomes very large or causes symptoms such as discomfort, stiffness, or painful swelling. There are three surgical approaches to treat the cyst: the standard posterior approach, the posteromedial approach, and the medial intra-articular approach. The first two methods are cyst removal methods. The latter method involves creating an opening in the cyst, which is later closed.
Physical therapy
Using ice for 15 minutes every 4 to 7 hours will reduce inflammation. Treatment is based on the principles of RICE (rest, ice, compression and elevation), followed by some muscle training exercises.
A rehabilitation program can improve knee control through a series of therapeutic exercises. This will increase the mobility of the joint and also increase flexibility. A physical therapist can develop a program to improve mobility and stretch the hamstrings, which may also include exercises to strengthen the quadriceps. This will result in less pain in about 6-8 weeks.
There is an experiment comparing ultrasound-guided corticosteroid injections with horizontal therapy (hardware physiotherapy). The 60 people were divided into three groups, injections only (Group A), horizontal therapy only (Group B) and (Group C) in which patients received both injections and horizontal therapy. Horizontal therapy was performed using a custom commercial device, and the investigators followed the manufacturer's instructions. In patients in groups A and C, pain decreased after a month. Group C had the lowest VAS scores and also the best WOMAC scores. In groups B and C, stiffness and disability scores were also improved to the greatest extent.
Treatment of soft tissue cysts
If the size of the cyst is small, there is no infection or cosmetic problems, a wait-and-see approach with a repeated examination by the surgeon is possible. In all other cases, surgical treatment is indicated - removal of the soft tissue cyst. Surgery at the Stolitsa network of clinics is performed on an outpatient basis under local anesthesia. The cyst is removed along with the capsule, and when suppuration occurs, the wound is thoroughly cleansed of pus and atheromatous masses. Further tactics depend on the specific clinical picture and extent of the process (wound drainage, cosmetic sutures, skin grafting). Full recovery usually occurs within one to two weeks. Provides excellent cosmetic results. If any tumor-like formations appear in soft tissues, immediately consult a doctor at the Stolitsa network of clinics in order, firstly, to make sure that it is of good quality, and, secondly, to get rid of it in a timely manner without causing complications, for example, possible suppuration.