Reasons for development
It is still unclear why soft tissue sarcomas occur, but certain risk factors have been identified.
Genetic predisposition
- nevoid basal cell syndrome (Gorlin syndrome);
- neurofibromatosis (von Recklinghausen disease);
- tuberous sclerosis (Bourneville disease);
- Gardner's syndrome;
- Werner's syndrome.
Carcinogens
The risk of developing angiosarcomas increases significantly with previous exposure to phenoxy herbicides (2,4-dichlorophenoxyacetic acid, 2,4,5-trichlorophenoxyacetic acid) and dioxins.
Immunosuppression
The most striking example is Kaposi's sarcoma in people with AIDS, autoimmune hemolytic anemia, and organ transplant recipients.
Most patients come with a complaint of tumor growth after an injury or bruise. There is no connection between trauma and the development of soft tissue sarcomas.
Causes
To date, medicine cannot accurately indicate the causes that contribute to the development of shoulder cancer. However, there are a number of negative factors that increase the risk of this pathology.
First of all, this means working in hazardous industries, constant contact with harmful substances and chemicals.
An important role is played by the quality of food consumed, namely the presence of carcinogens in them. Alcohol abuse also has a detrimental effect.
As with any other type of tumor, the appearance and course of the disease depends on the general health of the person, the level of the immune system and the presence of chronic diseases.
Malignant neoplasms of the shoulder, as well as cancer of the elbow joint, often occur in people with increased trauma.
Doctors pay special attention to children and adolescents due to the existing likelihood of developing pathology associated with increased growth of organs and tissues.
The risk of shoulder joint cancer increases in people whose direct relatives have suffered from cancer of various types and complexity.
Classification
Classification by tissue from which tumor formation occurs:
- Fatty – liposarcoma;
- Muscular:
- striated muscle tissue - rhabdomyosarcoma,
- unstriated muscle tissue – leiomyosarcoma;
- Vessels:
- circulatory – hemangiosarcoma,
- lymphatic – linfangiosarcoma;
- Connective – fibrosarcoma;
- Synovial membrane – synovial sarcoma;
- Nervous – neurogenic sarcoma;
- Skin – fibrosarcoma.
How to avoid getting skin cancer? What to avoid?
Sunlight. The most proven cause of both types of skin cancer, as well as melanoma, is exposure to sunlight. If you like to travel to hot countries, have fair hair and skin, or your work involves prolonged exposure to the sun, you should seriously consider UV protection.
Precancerous skin diseases are the next factor that may precede the development of the squamous cell form: actinic (solar) keratoses and cheilitis, leukoplakia, human papillomavirus infection of the mucous membranes and genitals. This type of tumor can also develop against the background of scar changes after burns or radiation therapy.
Contact with carcinogens
Various chemicals can lead to the development of skin cancer: arsenic and petroleum products.
Weakened immune system. People taking immunosuppressive drugs after an organ transplant or people living with HIV have an increased risk of developing squamous cell skin cancer.
Symptoms
Clinical manifestations and severity of symptoms depend on the primary location and size of the tumor.
Most often, soft tissue sarcomas of the head and neck are asymptomatic.
May be observed:
- pain;
- paresthesia is a disturbance of sensitivity along the course of peripheral nerves, which can manifest itself as burning, numbness, tingling;
- nerve palsies;
- trismus – spasm of the masticatory muscles, which is characterized by limitation of movements in the temporomandibular joint;
- ulceration of the mucous membrane;
- dysphonia is a phenomenon characterized by impaired vocal function;
- dysphagia – difficulty swallowing.
When soft tissue sarcomas are located near the nose, nasal congestion may occur that does not go away over a long period.
Stages of the disease
In order to prescribe an adequate course of treatment for shoulder cancer, experts distinguish several stages of its development.
At the first stage, the neoplasm is located at the site of its initial growth, without affecting neighboring tissues. The size of the tumor does not exceed 7 cm in diameter.
At the second stage, laboratory analysis confirms the risk of possible metastasis.
When the disease reaches the third stage, pathological cells affect neighboring anatomical structures and are detected in the lymph nodes.
The fourth stage poses the greatest danger to the health and life of the patient. Metastases are found in distant internal organs and tissues of the body.
Examples of soft tissue sarcomas of the head and neck
Kaposi's sarcoma
Osteogenic sarcoma of the alveolar process of the maxilla
Osteogenic sarcoma of the mandible
Pleomorphic sarcoma of the soft tissues of the neck on the right
Diagnostics
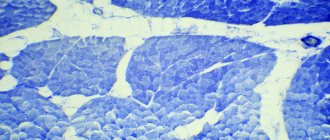
The diagnosis is made based on histological examination of tumor tissue.
There are two methods for obtaining material for research:
- core needle biopsy;
- open biopsy.
The biopsy should be performed in the location that during the operation will be included in the area of excision of the tumor formation.
Diagnostic algorithm:
- Examination: A lumpy, rounded yellow or gray nodule may be observed. It can have different densities and consistencies. Soft nodes - with liposarcomas, dense - with fibrosarcomas, jelly-like formations - with myxomas;
- Complete blood count with calculation of leukocyte formula and platelet count;
- Biochemical blood test with determination of liver and kidney function indicators (including electrolytes);
- Coagulogram;
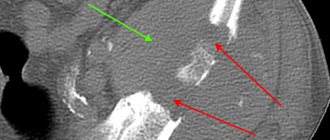
- MRI of the head and neck area;
- CT scan of the lungs;
- Ultrasonography;
- Radioisotope study of skeletal bones (for myxoid liposarcomas);
- CT scan of the brain (for alveolar soft tissue sarcoma and hemangiopericytoma).
Important: for the purpose of initial examination and clarification of the stage, routine PET scanning is not recommended.
Rehabilitation after mastectomy
Anti-Cancer Society
of the mammary gland
Breast loss is not only a cosmetic and physical disadvantage, but also directly changes the psychological status and social adaptability of women. For some women, the problem is “solved” with external prostheses.
Reconstructive and restorative operations are performed at the request of the woman in the absence of distant metastases and tumor recurrence. Read more in the section on reconstructive surgery after mastectomy.
Postmastectomy syndrome
Postmastectomy syndrome is a clinical syndrome that is a set of manifestations on the side of surgical treatment in the form of a postmastectomy defect (including cosmetic), cicatricial changes in the axillary region causing adductor contracture of the shoulder, brachioplexitis and/or neuropathy, edema of the upper limb ( postmastectomy edema, lymphedema), and in some women also in the form of psycho-emotional abnormalities in the form of restlessness, anxiety, mental exhaustion, and severe depression (in 25% of women), which leads to a significant deterioration in the quality of life.
The occurrence of early disorders accompanies the surgical stage of breast cancer treatment. The development of late complications is associated with radiation therapy and occurs from several months to 2-3 years after it. The result of radiation exposure is not only direct damage to the tumor elements of the mammary gland, but also to unchanged tissue structures of the axillary-subclavian region (fibrosis of soft tissues, development of gross scar changes). The progressive development of these processes, as well as the loss of many manual skills and the low therapeutic effectiveness of generally accepted rehabilitation therapy in patients, cause the development of scalenus syndrome, in which the nerves and vessels that supply not only the arm, but also the shoulder and the brain are compressed. When examined a year or more after radical treatment for breast cancer, scalenus syndrome is detected in 99.4% of patients.
Thus, as a result of surgical and radiation treatment of breast cancer, patients develop a whole complex of various disorders (specified in the definition), which is called postmastectomy syndrome. This is not only (1) edema of the upper limb; earlier, instead of the term “postmastectomy syndrome,” the term “postmastectomy edema” was used), but also (2) postoperative and post-radiation fibrosis of soft tissues, (3) plexopathy or damage to peripheral nerves, etc., and sometimes and cerebrovascular accidents. As a result, patients become severely disabled. But the most common pathological process in patients who have undergone radical treatment for breast cancer is lymphostasis of the soft tissues of the upper limb (postmastectomy edema), which in itself can cause damage to the m. supraspinatus (diagnosed on the basis of ultrasound data), chronic bursitis, contracture or limitation of the range of motion of the shoulder joint, plexitis and neuropathies, cellulite, scalenus syndrome and the development of lymphangiosarcoma (Stewart-Treves syndrome) against the background of long-term lymphostasis of the upper limb.
Classification of postmastectomy edema. The most comprehensive and optimal classification of postmastectomy edema is the classification proposed by T.A. Pantyushenko and M. Beltran (1990):
I degree (stage of preclinical manifestations of postmastectomy edema): the volume of the arm on the affected side increases to 150 ml compared to the opposite upper limb. No noticeable changes in the length of the shoulder circumference could be detected.
II degree (beginning of clinical manifestations of postmastectomy edema): the volume of the arm exceeds the opposite limb by 150-300 ml, the circumference of the shoulder is 1-2 cm; unstable swelling of the entire arm or its individual segments is visually noted. Eden appears in the evening and disappears in the morning. Patients feel heaviness in the arm and sometimes experience pain. The skin gradually loses the color inherent in a healthy limb and takes on rougher folds.
III degree (moderate postmastectomy edema): an increase in the volume of the arm by 300-500 ml or an increase in the circumference of the shoulder length by 2-4 cm. The swelling of the arm becomes permanent and does not disappear on its own by the morning. The skin becomes bluish, pale, and difficult to fold.
IV degree (severe postmastectomy edema): the volume of the arm is exceeded by 500-700 ml or the circumference of the shoulder by 4-6 cm. Permanent swelling of the arm occurs with the transition to fibroedema. The limb becomes deformed and partially loses its function.
V degree (aggravated postmastectomy edema): an increase in the volume of the arm by 700 ml or more or the circumference of the shoulder by more than 6 cm. The limb completely loses its function. Pronounced trophic disturbances appear. Patients are forced to keep their arm suspended.
Treatment. All treatment methods for postmastectomy edema can be divided into 3 groups:
- physical and physiotherapeutic (pneumatic compression with sequential compression of the upper limb from distal to proximal; mechanical lymphatic and manual lymphatic drainage, pneumatic massage; physical exercises complementing massage, etc.);
- medicinal (benzopyrones, primarily coumarin and its combination with troxerutin, as well as diosmin, daflon, paroven, venastat, etc.);
- surgical (removal of fibrous tissues followed by autodermoplasty, etc.).
Prevention of postmastectomy syndrome (National Lymphedema Network):
- Never ignore the appearance of even minor swelling in the arm, hand, fingers, or chest (consult your doctor immediately).
- For injection or blood collection, the hand on the side of the operation should not be used.
- Measure blood pressure only on the uninjured arm.
- The necessary hygiene must be observed, after bathing, use moisturizing lotions, dry your hand gently but thoroughly. Make sure all folds and skin between your toes are dry.
- Avoid repeated vigorous, resistive movements of the injured arm (brushing, pushing, pulling, etc.). (6) Avoid lifting heavy objects with the injured hand. Never carry heavy bags over your shoulder or in your hand on the side of surgery.
- Avoid wearing tight jewelry or elastic bands on the affected arm or fingers.
- Avoid strong temperature fluctuations when swimming and washing dishes; visiting a sauna or taking hot baths is also not recommended (at least keep your hand outside the bath). Always protect your hand from the sun.
- Try to avoid any kind of injury to the injured hand (blows, cuts, sun or other burns, sports injuries, insect bites, scratches). Watch for signs of infection.
- Wear gloves when doing housework, gardening, or other work that may cause even minimal damage.
- Avoid cutting cuticles when doing manicures.
- Discuss a set of exercises with your doctor. Do not overload the injured arm; if it starts to hurt, you need to lie down and raise your arm up. Recommended exercises: walking, swimming, light aerobics, cycling. Do not lift more than 6 - 7 kg.
- When traveling by air, you should wear a compression sleeve of the appropriate size. While in the air, increase your fluid intake.
- Women with large breasts should wear lightweight dentures. The bra should be chosen correctly: not too tight and not contain “wires”.
- Use an electric razor to remove hair in the armpit area.
- People with lymphedema should wear a well-fitting compression sleeve at all times while they are awake. If the sleeve is too loose, it is most likely that the volume of the arm has decreased or the sleeve is worn out.
- Attention: if a rash, itching, redness of the skin, pain, or fever appears, consult a doctor immediately. Inflammation (infection) of the injured arm may be the onset or worsening of lymphedema.
- Try to maintain your normal weight. A low-salt (reduced sodium), high-fiber diet should be well balanced. Do not smoke or drink alcoholic beverages. The diet should contain easily digestible protein (fish, chicken, tofu).
Treatment
The treatment of a patient with sarcomas of the soft tissues of the head and neck requires an integrated approach with the involvement of a number of specialists: a morphologist, a surgeon, a radiation diagnostician, a chemotherapist, and a radiologist.
Surgery
Surgery is the main treatment method for patients with this pathology.
Soft tissue sarcomas grow within the capsule, which subsequently pushes away nearby tissue. This shell is called a pseudocapsule. Surgery involves removing the pseudocapsule en bloc with negative resection margins without damaging it, since violating the integrity of this formation increases the risk of tumor recurrence.
Postoperatively, radiation therapy may be administered to provide local control.
Additional treatments include chemotherapy and radiation therapy.
Radiation therapy
Preoperative radiation therapy provides significant advantages - the operating conditions are improved and the size of the tumor formation is reduced.
The negative aspect of this treatment is the high incidence of postoperative complications of an infectious nature.
Chemoradiation therapy
Treatment that combines chemotherapy with radiation therapy is called chemoradiotherapy.
Chemotherapy can improve the effectiveness of radiation therapy, so they are sometimes used together. This is a combination of systemic and local therapy.
Basal cell skin cancer
Basalioma is the most common, but at the same time the safest type of skin cancer. Death from basal cell carcinoma is possible only in very advanced cases or with aggressive forms (basosquamous) tumor. The favorable course of basal cell carcinoma is due to the fact that it almost never metastasizes (only 0.5% of cases).
Symptoms and signs
Most often, basal cell carcinoma occurs on the skin of the nose, a little less often on the face and much less often on other parts of the body.
The peak incidence occurs over the age of 40 years. The youngest patient diagnosed with basal cell carcinoma by histology was 39 years old.
What basal cell skin cancer looks like depends on the form:
- Nodular form (synonymous with nodular). The tumor is presented in the form of a nodule. It can be distinguished from other skin formations by an increased number of vessels on the surface, a waxy sheen and small gray-blue inclusions. All these signs are visible in the photo.
Nodular form of basalioma
In addition, on the surface of nodular basalioma there may be another characteristic sign - ulceration.
Nodular basal cell carcinoma with ulceration
- The superficial form of basal cell carcinoma in most cases is presented as an area of redness on the skin. Elements of peeling and the waxy sheen already mentioned above are also possible.
Superficial form of basalioma
- Scleroderma-like form of basalioma is very rare and often presents difficulties in diagnosis. It is characterized by a lighter and harder seal compared to the surrounding skin.
Scleroderma-like form of basalioma
- The pigmented form of basal cell carcinoma makes up a very small part of the total number of these tumors. It is distinguished by a large amount of pigment. In this regard, basal cell carcinoma is often mistaken for melanoma when examined without a dermatoscope.
Pigmented form of basalioma
- The ulcerative form of basalioma can reach very large sizes and in advanced cases is practically untreatable.
Ulcerative form of basalioma
Photos in the initial stage
Unfortunately, basal cell skin cancer is extremely difficult to diagnose in the early stages, i.e. when it is minimal in size. Here are some photos:
Basalioma of the skin of the nose, nodular form, size 5 mm
Basalioma, nodular form, 3 mm in diameter
Nodular basalioma of the temporal region, diameter 2 mm
Diagnosing basal cell carcinoma in the early stages, when the tumor is small, can present significant difficulties. Only a combination of a comprehensive examination of the entire skin, a thorough determination of the history of the existence of the formation and dermatoscopy will help in establishing the diagnosis of basal cell carcinoma at an early stage.
Basaliomas with high and low risk of recurrence (NCCN, 2018)
Area H: Facial mask (including eyelids, eyebrows, skin around eyes, nose, lips [skin and red border of lips], chin, lower jaw, skin/grooves in front and behind the auricle, temples, ears), genitals, palms and feet .
Area M: cheeks, forehead, scalp, neck and legs
Region L: trunk and limbs (excluding shins, palms, feet, nails and ankles)
Notes
- Localization, regardless of size, may be a sign of high risk
- Histological forms of low risk: nodular (nodular), superficial, keratotic, piloid, with differentiation towards skin appendages, Pincus fibroepithelioma
- Area H means high risk regardless of size
- Morphea-like, basosquamous (metatypical), sclerosing, mixed infiltrative, micronodular in any part of the tumor
To assign a tumor the status of “high risk of recurrence”, only one of the factors from the right or left column is sufficient.
Treatment of basal cell carcinoma
The main goal of treatment for basal cell carcinoma is complete removal of the tumor while maximally preserving the cosmetic properties and functions of those parts of the body where this tumor has developed.
As a rule, the best results are achieved by surgical methods. However, the desire to maintain functionality and cosmetic properties may lead to the choice of radiation therapy as the primary treatment modality.
Depending on the degree of risk of relapse (see above), the approach to treating basal cell carcinoma may vary.
In patients with superficial basal cell carcinoma and a low risk of recurrence, when surgery or radiation therapy is contraindicated or inappropriate, the following treatments may be used:
- 5-fluorouracil ointment;
- Imiquimod ointment (Aldara, Keravort);
- photodynamic therapy;
- cryodestruction.
Mohs micrographic surgery may be recommended for patients at high risk of recurrence.
Chemotherapy for basal cell carcinoma includes drugs that are inhibitors of the hedgehog signaling pathway – vismodegib (Erivedge) and sonidegib (Odomzo). These drugs can help in cases where surgical methods, like radiation therapy, are not applicable or contraindicated.
What you need to know about basal cell carcinoma?
- In the vast majority of cases, basal cell carcinoma does not pose a threat to life.
- If a histological examination of a distant formation results in basal cell carcinoma, there is nothing to worry about. It is important to make sure that the formation is completely - be sure to consult with an oncologist.
- If, after removal of a basal cell carcinoma, the histological examination contains the phrase “tumor cells in the resection margin” or something similar, further treatment in order to completely remove the tumor.
- strongly do not recommend removing basal cell carcinoma without histological examination, since even a very typical-looking formation may not be what it seems at first glance.
- Basalioma needs to be treated . Observation is a bad option for a diagnosis like this. Treatment of advanced forms (see photo of ulcerative form) is extremely difficult and expensive.
- If you have already had a basal cell carcinoma removed, you should regularly have your entire skin examined by an oncologist in order to possibly identify another such tumor.
- The likelihood of metastasis in the metatypical (basosquamous) histological type is higher than in other types.
Treatment for a common process
Chemotherapy is the mainstay of treatment for advanced disease because the drugs injected enter the bloodstream and reach cancer cells throughout the body.
The most common chemotherapy drugs used for soft tissue sarcomas are doxorubicin, trabectedin, gemcitabine, docetaxel, and paclitaxel. These drugs may be prescribed alone or in combination.
Chemotherapy in patients with progressive disease should be based on doxorubicin or epirubicin, both drugs belong to the anthracyclines. In patients with angiosarcoma, paclitaxel or docetaxel may be offered instead of doxorubicin.
Adding another drug(s) to doxorubicin or epirubicin may enhance the effect of systemic chemotherapy in some patients. This choice primarily depends on the histological type of cancer.
If the first chemotherapy does not give the expected result, then another chemotherapy may be offered. The choice of one or more drugs will depend on previously used drugs, as well as on the histological type of the tumor. Drugs that may be considered include ifosfamide, trabectedin, gemcitabine, docetaxel, and paclitaxel.
Targeted therapy
This treatment works by binding to a specific protein or structure involved in tumor growth and progression. Side effects differ from traditional chemotherapy and depend on the mechanism of action of the drug. Targeted drugs approved for use in soft tissue sarcomas in Russia are:
- pazopanib – for soft tissue sarcomas other than liposarcomas;
- imatinib – for dermatofibrosarcoma, when systemic therapy is required.
Radiation therapy
Radiation therapy may be used to relieve symptoms or prevent complications, such as bone metastases.
Surgery
Surgical treatment of metastases may be considered depending on their location and medical history. For example, when lung metastases appear long after initial treatment and when, in the opinion of the surgeon, they can be completely removed.
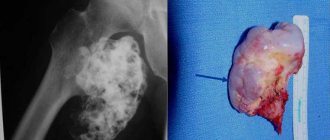
Symptoms of bone cancer
The clinical picture of bone cancer consists of the following symptoms:
- Pain at the site of the tumor (the patient constantly experiences pain, which intensifies with movement and physical activity, as well as at night when the muscles are relaxed; in children this is sometimes mistaken for “growing pains”);
- Swelling around the area affected by the tumor (such swelling becomes noticeable only in the later stages, when the tumor has reached a large size; in other cases, the swelling cannot always be felt);
- Difficulty in movement (when the tumor is located around or near a joint, it affects its function, while limiting the movement of the limb as a whole; if the leg is affected, the person begins to limp, experiencing tingling in the limb or numbness);
- Pathological bone fractures (quite often cancer is discovered after a bone fracture due to an accident or fall);
- Deformation of the body or limb;
- Fatigue, lethargy, sweating, high temperature, weight loss (these are the so-called symptoms that are characteristic of cancer in general).
Similar symptoms occur in many other diseases, but if pain in the limbs lasts more than two weeks, it is recommended to immediately consult a doctor for qualified help and undergo examination.
Forecast
The prognosis for soft tissue sarcomas of the head and neck largely depends on the size of the tumor, primary location, etiology, and the presence of local or distant secondary foci of malignancy. With early diagnostic measures and adequate timely therapy, the prognosis is favorable.
Bibliography:
- NCCN Guidelines for Patients: Soft Tissue Sarcoma, 2021.
- Shah. Head and Neck Surgery and Oncology 5 ed., 2021.
- Soft tissue sarcomas: a guide for patients – Information based on ESMO Clinical Practice Guidelines – v.2016.1
- Fedenko A. A., Bokhyan A. Yu., Gorbunova V. A., Makhson A. N., Teplyakov V. V. Practical recommendations for drug treatment of soft tissue sarcomas. Malignant tumors: Practical recommendations RUSSCO #3s2, 2021 (volume 9). pp. 272–282.
Possible complications and prognosis
The most common complication of a cancerous tumor of the shoulder is infectious infection of the tissue, which subsequently led to amputation of the arm.
In addition, a malignant neoplasm at stages 3–4 gives metastases to regional lymph nodes and distant anatomical structures. The result of this pathological process is the establishment of disability or death.
The prognosis of the treatment process is individual and is largely related to the patient’s general health, age, level of immunity, stage of cancer development and the presence of metastases.
The most successful treatment for the patient is considered to be the beginning of treatment for the pathology in the first stages of its development. In this case, the probability of getting rid of cancer is at least 80%.
When a secondary neoplasm is detected, the chances of recovery are significantly reduced. According to statistics, in this case, life expectancy is no more than 1 - 1.5 years.