Vocal cord granuloma is a benign formation that occurs as a result of injury or irritation of the vocal cords. The cause of granuloma may be trauma to the mucous membrane of the larynx caused by intubation. Postintubation granulomas of the larynx occur only in women, because their larynx is smaller and more sensitive to injury. The formation is quite rare - it occurs with a frequency of 1 granuloma per 800-1000 intubation anesthesia. The period of formation of such granulomas after intubation is from two to seven months. Spontaneous granulomas of the vocal cords are more common. The cause of irritation of the larynx is often laryngopharyngeal reflux (reflux of the contents of the pharynx into the larynx). This leads to the formation of vocal cord granulomas.
Typically, manifestations of this disease of the vocal cords are the sensation of a foreign body in the larynx, hoarseness of the voice and its intermittency. The first indicated symptom is the most characteristic and disturbing to the patient, which leads to the desire to cough up a foreign body, causing a cough, which itself is also the cause of irritation of the larynx and vocal cords. As a result, a granuloma is formed.
Unlike many other formations of the vocal cords, granuloma is most often found above the vocal process, along the posterior surface of the cords. Polyps are not found in this location.
Typically, the manifestations of a granuloma depend on its size. It can even prevent the glottis from closing, resulting in less hoarseness and the person being unable to speak loudly. This leads to a kind of vicious circle: the person tries to speak louder. Straining the vocal cords, which in turn causes irritation and trauma. This, in turn, again leads to the development of granuloma. If the granuloma is attached to the vocal cords by a stalk, it may become dislodged, causing the voice to become choppy when speaking.
Granuloma is one of the formations of the vocal cords that can cause pain. Usually, pain occurs when coughing, swallowing or expectoration due to direct irritation of the granuloma. Sometimes, this pain may radiate to the ear on the affected side.
Typically, a granuloma is a small pale or pinkish formation located above the vocal process. It resembles a raised area above the surrounding mucous membrane. Sometimes granulomas can reach large sizes, spherical formations. It can be either on a wide base or on a thin leg. Sometimes, under the influence of the edge of the opposite vocal cord, it can be split.
Granulomas tend to grow as long as they are irritated. Sometimes a vocal cord granuloma can grow so large that it lacks blood flow and dies. However, this does not mean that a new granuloma will not arise at this location, since the reason for its formation (irritation) does not disappear along with the granuloma.
It should be noted that simple surgical removal of the granuloma does not solve the problem, since if the irritating factor is left in place, the granuloma will certainly appear again. In fact, eliminating the irritating factor makes it not even necessary to remove the granuloma, since after eliminating the irritating factor it gradually resolves on its own.
Treatment of vocal cord disease
If the patient has laryngopharyngeal reflux (that is, the reflux of acidic gastric contents into the larynx), this problem should first be eliminated. To do this, you need to adjust your diet. In addition, antacid medications help reduce acidity. You often have to take large doses of these drugs over several months.
In the treatment of vocal cord granuloma, voice therapy also plays a role, which is aimed at reducing irritation of the vocal cords.
Surgical treatment of granulomas is usually considered the last method, which is resorted to in case of ineffectiveness of conservative measures, since with proper compliance with all these measures, granulomas usually go away on their own. Most often, surgery is indicated for large granulomas in order to increase the effectiveness of conservative treatment. Let us recall that simple removal of the granuloma usually leads to the reappearance of the granuloma.
What diseases does a phoniatrist treat?
A phoniatrist must have basic knowledge of the diagnosis and treatment of organs involved in voice formation.
He specializes in pathological changes in the vocal apparatus and voice restoration. The phoniatrist treats the following conditions:
- vocal fold cyst, acute or chronic laryngitis in the acute stage, papillomatosis or paralysis of the larynx, nodules, polyps, paresis.
- functional dysphonia (spastic, hypotonic, hypertonic, etc.);
- neoplasms in the larynx, in the folds;
- deals with voice restoration after surgical treatment of laryngeal diseases.
Vocal fold nodules
Vocal fold nodules (cords) are benign growths that form as a result of constant overload of the vocal folds. Nodules are most often found in singers and people whose work involves excessive stress on the vocal folds. It has been noted that most often vocal fold nodules appear in women aged 20–50 years. Overload of the vocal folds leads to the formation of small seals on them. Over time, these seals harden and become callus-like. As the vocal folds continue to be stressed, these nodules increase in size. Usually the nodules on the vocal folds are located symmetrically. Nodules are not tumor or pre-tumor diseases. As already stated, the main cause of vocal fold nodules is the overload placed on the vocal folds. In addition, long-term smoking, decreased thyroid function (hypothyroidism), and gastroesophageal reflux disease can lead to the formation of such nodules and polyps. The most typical manifestation of vocal fold nodules is painless hoarseness. This phenomenon is caused by unevenness in the closure and vibration of the vocal folds. Typically, some tension on the vocal folds leads to worsening hoarseness. After a short rest, the hoarseness goes away. In appearance, during laryngoscopy, vocal fold nodules are small, symmetrically located growths of tissue along the edges of the vocal folds. The color of the nodules is the same as the ligaments, which distinguishes them from polyps of the vocal folds, which are usually red. In addition, the nodules never experience intensive growth, although some swelling of the ligaments may be observed after overstraining the ligaments. It should be noted that unilateral formations on the vocal folds are not nodules. The nodules are usually arranged symmetrically in pairs, and are always the same size. Paired vocal fold formations that are not symmetrically arranged should be carefully examined. Most often these can be cysts or polyps of the vocal folds.
- Diagnosis of vocal fold nodules
- Diagnosis of vocal fold nodules is usually done using laryngoscopy.
- Treatment of vocal fold nodules
Usually, in case of hoarseness, laryngologists always advise maintaining a voice mode - that is, not speaking loudly, but, if possible, limiting vocal communication. This may improve the condition of the voice somewhat, and also lead to some shrinkage of the nodules, but they do not disappear completely. "Vocal rest" may help reduce swelling of the vocal cords. Following a voice regimen can return the voice to its previous level, however, if the voice is overloaded, hoarseness may recur again until its cause is eliminated. The use of anti-inflammatory drugs and steroid hormones can reduce swelling and inflammation of the vocal cords, but again, this treatment cannot eliminate the cause itself.
Voice therapy is the mainstay of treatment for vocal fold nodules. The goal of this therapy is to teach the patient to control their voice to avoid problems in the future. However, it is important to understand that voice therapy alone does not eliminate nodules. It only helps to soften them and make them more mobile, resulting in an improved voice.
Endolaryngeal microsurgery methods are used to remove vocal fold nodules. In this case, endoscopic instruments are used to visualize the lumen of the larynx and pathological foci on the monitor screen. Removal of nodules is possible either using a laser or cryosurgical methods.
Diagnosis of voice disorders
The most accurate diagnosis for voice disorders can be made by a doctor based on medical history, examination and some other types of research.
Diagnosis may require indirect laryngoscopy using a mirror and a forehead lamp. If this procedure does not give the desired result, it can be performed using a flexible fiberoptic laryngoscope. This procedure is performed under local anesthesia. In case of acute inflammation of the larynx, the patient can see redness of the larynx without the presence of discharge. Using this study, benign and malignant tumors of the larynx can also be detected.
If the laryngeal nerve is injured, the patient may experience vocal cord paralysis on one side. If this pathology is detected, the doctor must conduct an additional examination to identify the factors that provoked this condition.
When examining the neck, the doctor must rule out the presence of a goiter. If the supraclavicular lymph nodes are detected to be enlarged, the doctor may suspect the patient has tumors in the esophagus.
During an examination of the chest organs, the specialist must exclude the patient from collapsing lung lobes and inflammation of the pleura, which often accompanies lung cancer.
In some cases, it may be necessary to conduct laboratory and instrumental studies, which include:
- ESR - performed for inflammation of the larynx, neoplasms;
- RGC - for malignant lung tumors;
- tensilone test - for patients with autoimmune neuromuscular diseases;
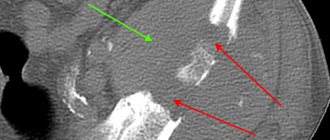
- computed tomography of the cervical spine - prescribed for patients with laryngeal or thyroid cancer to determine its stage;
- computed tomography of the chest - performed for tumors in the lungs, an increase in the diameter of the thoracic aorta;
- endoscopy - prescribed for suspected esophageal cancer;
- aortography of the aortic arch;
- OAC - prescribed to patients with inflammation of the larynx;
- biopsy - for thyroid tumors.
Some patients are recommended to be additionally examined by a phoniatrist and a neurologist.
Vocal cord polyps
Vocal cord polyps are small, benign growths usually located in the middle of the vocal cords. Some researchers believe that the cause of polyps is small, limited hemorrhages in the vocal cords when they are torn, which occurs during overexertion. The most typical manifestation of vocal cord polyps is painless hoarseness. This phenomenon is caused by uneven closure and vibration of the vocal cords due to the presence of a formation on their surface. If the polyp has a thin stalk that attaches it to the vocal cord, it may move when the vocal cords contract, causing the voice to become choppy. In some cases, these voice changes may be accompanied by a sensation of a foreign body in the larynx and a desire to get rid of it. Typically, polyps are formations of red or reddish color, with clear edges, delimited from surrounding tissues. The polyp can have a thick base or a thin stalk. The surface of the polyp can be smooth and even, or have a lobular structure. The sizes of polyps can vary. Polyps can be single or located in pairs on each vocal cord opposite each other. They are almost always located in the middle of the vocal cord. Usually the growth of polyps does not occur in a short time, although sometimes there are exceptions. Such exceptions occur with repeated injuries. In any case, a formation that grows quite quickly (over a few weeks) is not typical for a polyp and should be carefully examined after a biopsy.
Since vocal cord polyps most often appear due to vocal trauma, voice therapy is highly recommended to reduce their manifestations. If the polyp has recently appeared, voice therapy can minimize its manifestations.
- Diagnosis of vocal cord polyps
- Diagnosis of vocal cord nodules is usually done using laryngoscopy.
- Treatment of vocal cord polyps
Usually, in case of hoarseness, laryngologists always advise maintaining a voice mode - that is, not speaking loudly, but, if possible, limiting vocal communication. This may slightly improve the condition of the voice, and also lead to a slight reduction in the size of the polyps. "Vocal rest" may help reduce swelling of the vocal cords. Following a voice regimen can return the voice to its previous level, but if it is overloaded, hoarseness may reappear until its cause is eliminated. The use of anti-inflammatory drugs and steroid hormones can reduce swelling and inflammation of the vocal cords, but again, this treatment cannot eliminate the cause itself. Voice therapy is also used to treat vocal cord polyps. The goal of this therapy is to teach the patient to control their voice to avoid problems in the future. However, it is important to understand that voice therapy alone does not eliminate polyps. It only helps to soften them and make them more mobile, resulting in an improved voice. Endolaryngeal microsurgery methods are used to remove vocal cord polyps. In this case, endoscopic instruments are used to visualize the lumen of the larynx and pathological foci on the monitor screen. Removal of polyps is possible either using a laser or cryosurgical methods.
Signs of ligament pathology
Physiologically, there are no nerve endings in the vocal folds, so pathological changes do not cause pain.
But there are a number of symptoms and manifestations that require seeking medical help. It is necessary to pay attention to the following manifestations:
- “loss” of voice after an infectious disease (if more than a week has passed after recovery);
- loss of voice after injury, overexertion, as a result of stress;
- hoarseness, change in smoothness or loss of expressiveness of the voice, hoarseness;
- feeling of a lump in the throat, the need to clear your throat before speaking;
- shortness of breath, feeling of shortness of breath during a conversation;
- pain when swallowing;
- feeling tired after using your voice for a long time;
- prolonged mutation in adolescents.
Spastic voice disorders in diseases of the vocal cords
Spasmodic voice disorders (spasmodic dysphonia) are expressed in involuntary movements of the vocal cords. Typically, spasmodic dysphonia occurs in adults aged 30–40 years. The most common adduction type of spasmodic dysphonia is characterized by the fact that the vocal folds close together when pronouncing a sound. With the abduction type, the vocal cords, on the contrary, open. Spastic voice disorders are not hereditary. Causes of spasmodic dysphonia: • psychological trauma, • stress overload, • overstrain of the vocal cords. With the adduction type of spasmodic dysphonia, a strained, tense, unnatural voice is noted. This occurs as a result of the vocal cords closing too close. With the abduction type of spastic dysphonia, the ligaments move away from each other, as a result of which the voice becomes silent and airy. In both cases, the manifestations of this pathology can change every day. People with spasmodic dysophnia report difficulty communicating with strangers or speaking in public. Communication on the phone is especially difficult. Like many types of dystonia, manifestations of spasmodic dysphonia are mostly associated with a certain type of activity. Other functions of the larynx, such as breathing, are not impaired. Sometimes the voice may be normal when singing or laughing, but during normal conversation its pathology appears. This property of this disease, combined with changes in the characteristics of the voice during emotional stress, sometimes leads to a misconception about the mental causes of its occurrence. However, spasmodic dysphonia is not a psychiatric or psychological disorder. Since spasmodic dysphonia is a disorder of the motor function of the vocal cords, examination of the larynx in this pathology is necessary during a conversation. Usually this disorder of the vocal cords manifests itself in the form of their short spastic movements, which are sometimes even difficult to detect. This is especially true when examining the larynx and vocal cords during rigid endoscopy, during which the patient is forced to stick out his tongue. Therefore, it is advisable to use a flexible fiberscopic technique to diagnose spasmodic dysphonia. Treatment for spasmodic dysphonia Unfortunately, there is no cure for spasmodic dysphonia. Treatment, however, can reduce the manifestations of this pathology. It should be noted that if this disease is not treated, its course does not worsen. The most popular treatment for spasmodic dysphonia is injection of botulinum toxin into the muscles of the vocal cords. Botulinum toxin is a waste product of Clostridium botulinum. As you know, botulism is a serious infectious disease that manifests itself with neurological disorders. Botulinum toxin affects nerve fibers, causing them to stop transmitting nerve impulses. This leads to paralysis of the muscles they innervate. This property of botulinum toxin has found wide application in medicine and cosmetology, in particular, in the form of Botox injections - a special form of botulinum toxin used in plastic and aesthetic surgery to eliminate wrinkles on the face. The same principle of action of botulinum toxin is based on its use in the treatment of spasmodic dysphonia. The toxin relaxes the muscles that cause excessive contraction of the vocal cords. Neither medication nor psychotherapy or voice therapy alone can control the symptoms of spasmodic dysphonia. Botulinum toxin has been used in medicine since 1984. The basis of its use, as already mentioned, is muscle relaxation. In the case of adduction spasmodic dysphonia, these are the muscles that close the vocal cords. In the case of abduction spasmodic dysphonia, these are the muscles that push the vocal cords apart. The injection into the vocal muscles is carried out through the skin in the neck area. The procedure is usually performed on an outpatient basis and after the procedure the patient can safely go home. In the case of adductive spasmodic dysphonia, after an injection into the muscles, the voice may be aspirated and whispering for some time; sometimes, when taking liquid, the patient may choke or cough. If this side effect is too pronounced or lasts more than 7–10 days, then the injected toxin is corrected. In the case of abduction spasmodic dysphonia, excessive relaxation of the muscles that open the vocal cords may cause difficulty breathing. It is worth noting that in the case of this type of spasmodic dysphonia, it is somewhat more difficult to avoid complications. If treatment of spasmodic dysphonia with botulinum toxin injections is ineffective, surgical intervention is used on the nerves that approach the larynx (their dissection or destruction). This method has good results, however, in the case of severe spasmodic dysphonia associated with brain pathology, the disease may recur after several months or years.
Classification of voice disorders
In medicine, voice disorders are divided according to the degree of manifestation of the disorder into:
- Dysphonia is a disorder in which the strength of the voice decreases, its color and pitch change. With dysphonia, the voice becomes hoarse, lowers, and becomes hoarse;
- aphonia is a disorder during which the voice disappears completely. With aphonia, a person can only whisper.
According to the mechanism of development, these disorders are divided into:
- organic;
- functional.
Based on the location of lesions of the vocal apparatus, voice disorders are:
- central - voice disorder resulting from pathological processes occurring in the middle of the vocal apparatus;
- peripheral - pathological changes occur in the peripheral part of the vocal apparatus.
Examination and diagnosis by a phoniatrist
The examination of the patient begins with an assessment of his condition, evaluation of complaints and voice characteristics.
The doctor must collect a history of the disease, allergic status, concomitant diseases, what medications the patient is taking, hormonal levels, and previous surgeries. Diagnostic methods:
- indirect laryngoscopy – examination of the larynx using mirrors;
- videofibrolaryngoscopy – examination of the larynx with a flexible endoscope through the nose, allows examination at any age (from 0 to 99+), in patients with a pronounced gag reflex;
- video stroboscopy - examination with a device that allows you to obtain a multiply enlarged image of the larynx, examine hard-to-reach areas, evaluate the oscillatory movements of the vocal folds and make a video recording
The specialist can use additional instrumental diagnostic methods - X-ray, ultrasound, CT, MRI. To clarify the diagnosis, the specialist prescribes laboratory diagnostic methods - a swab from the throat, larynx for microflora and sensitivity to antibacterial drugs, a blood test.
After a complete examination, the doctor prescribes a therapeutic course. Therapy can be conservative or surgical. Conservative therapy includes medication, physiotherapy, and phonopedia. Surgery is prescribed for tumors in the larynx or vocal folds.
How to save your voice?
The human voice is a delicate instrument that requires delicate handling.
Smoking, alcohol, telephone conversations, working in dusty rooms, loud speech - this is a list of factors that negatively affect the vocal apparatus. Prevention measures:
- observe the vocal load regime. In case of overexertion, you need rest, complete silence (6-12 hours are necessary for recovery);
- do not lie down immediately after eating to prevent reflux of the food bolus and entry through the esophagus into the larynx;
- balanced diet. Elimination of carbonated drinks, spicy, too hot foods;
- giving up alcohol and smoking;
- rest, stress reduction;
- breathe through your nose. This protects the respiratory tract from dust, viruses, and infections;
- control the level of humidity in the room;
- drink enough water per day.
Representatives of voice-speech professions are recommended to consult a phoniatrist at least once every six months.
Lost voice: diagnostics
Diagnostic methods:
- Patient interview.
- Examination of the patient, oropharyngoscopy, laryngoscopy, rhinoscopy, videolaryngoscopy (examination of the larynx with an endoscope at high magnification), videostroboscopy. Using video stroboscopic equipment, the specialist receives an enlarged image of the larynx. This method makes it possible to examine a hard-to-reach area to diagnose pathological changes at an early stage.
- Instrumental studies (ultrasound, MRI, CT).
- Laboratory diagnostics.
If the problem arose due to concomitant diseases, the phoniatrist may recommend consultation with a related (subspecialty) specialist.