Types of most likely complications
Tonsillitis develops due to the penetration of bacteria and viruses into the oropharynx, which cause pain and symptoms of intoxication. Timely intake of antibacterial agents and compliance with all doctor’s recommendations allows you to destroy the causative agent of the disease in the primary focus of microbial development. If this does not happen, there is a high probability that bacteria will spread throughout the body through the blood or lymph flow, which leads to inflammation of the internal organs.
All possible complications of any type of tonsillitis are divided into local and systemic (general). Local ones are easier to tolerate, although they lengthen the recovery time and significantly weaken the immune system. General complications are less common, but they are much more dangerous for the patient.
Chronic tonsillitis
A lot is known about tonsillitis - inflammation of the tonsils - so much so that the information is available to almost anyone. In the context of a condition that is described as a “sore throat” and characterizes the dysfunction of an organ, which is usually called in the French manner, le glande (“acorn”), the choice of a treatment plan is often considered. The success of the latter does not always lie in surgical removal or persistent conservative treatment.
Let's try to understand what follows the appearance of the diagnosis of tonsillitis and what forms the disease takes. To do this, we need a “patient model”: a description of a group of potential owners of unhealthy “tonsils”. By the way, healthy palatine tonsils often have the shape of an “acorn” (le glande), and with tonsillitis, the latter acquire a spherical shape.
- Tonsillitis is more common and, accordingly, the number of cases of its surgical treatment is increasing among children 4-12 years old and adults 20-30 years old. These periods correspond to the restructuring of the lymphoid tissue of the pharynx, maturation and implementation of barrier properties in accordance with the characteristics of the microflora inhabiting it.
- Our patient is often sick - these are viral infections, somatic diseases associated with immune disorders, and various congenital syndromes.
- Enlargement of the palatine tonsils and, often, the nasopharyngeal or adenoid tonsil does not allow free breathing: both the lymphoid tissue itself and swelling of the nasal mucosa are an obstacle. Nasal obstruction syndrome develops.
- Breathing disorders are especially pronounced during sleep, when there is no possibility of using additional muscular effort, the patient breathes only due to the work of the diaphragm. Snoring appears, and less often, episodes of short pauses in breathing during sleep. As Yevgeny Vaganovich Petrosyan said, “when I sleep, I don’t control myself.”
- Microbial communities in the form of colonies covered with a “shell” of complex carbohydrates (“films”) are expressed on the root of the tongue, the posterior wall of the pharynx and in the recesses (crypts) of the tonsils. Excess microflora creates conditions for unpleasant odor from the mouth (halitosis).
- Sometimes inflammation in the tonsils causes problems with the functioning of the throat muscles and makes swallowing difficult (dysphagia).
The choice of the “optimal” method of treating tonsillitis led in the 40-50s of the 20th century to their widespread removal in almost all patients, starting from the period of physiological enlargement in childhood. The price for this was a sharp deterioration in the body's anti-infective defenses. Already in the early 50s, the authors refuted their point of view, calling the method of treating tonsillitis without specifying the indications “orgy.” About 50 years have passed, and the criteria (also known as indications for surgery) for tonsillectomy have become generally accepted (Paradise, 1984):
- Number of relapses of tonsillitis: more than 7 in the previous year, or more than 5 in each of the 2 previous years, or more than 3 in each of the previous 3 years (from the patient’s perspective).
- Sore throat and one of the signs: body temperature more than 38.3, cervical lymphadenitis (node more than 2 cm), exudate in the tonsils, culture of group A beta-hemolytic streptococcus (GABHS).
- Previous treatment: Antibiotics against GABHS in every episode.
- Condition: each episode of tonsillitis is documented by a doctor, or the doctor observed 2 episodes in the patient.
Tonsillitis has acquired the status of an infectious disease with systemic complications, which often have a more negative impact. One of the most severe diseases aggravating the course of tonsillitis is kidney damage.
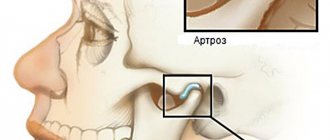
Sound phenomena produced by the patient during sleep: loud labored breathing, extraneous noises - vibrations of the soft tissues of the pharynx, or short episodes of lack of breathing. However, in addition to the reaction of those around you, you should pay attention to the structural features of the patient’s face (see figure). A small lower jaw (micrognathia) and a small narrow laryngopharynx are anatomical prerequisites for poor breathing, even with a slight increase in lymphoid tissue. And, on the contrary, a deep bass voice is a sign of a large-volume laryngopharynx - even a significant increase in the palatine tonsils will not immediately affect breathing characteristics.
Intoxication, prolonged episodes of a slight increase in body temperature (to subfebrile values) over several weeks are a formidable sign of a harmless enlargement of the tonsils. In such patients, the risk of diseases not apparently related to tonsillitis increases. And one more quote from the repertoire of Faina Georgievna Ranevskaya. “Medicine is making amazing progress. Previously, at the reception they told me to “take off your clothes.” Now, just “open your mouth.” That's all." Most likely, F.G. Ranevskaya unconsciously emphasizes the attention of therapists to the condition of the palatine tonsils. And it's not a joke.
Even charismatic doctors, supporters of “evidence-based medicine” (EBM), allow themselves to ask the question of the appropriateness of choosing a treatment method. In the following, we briefly summarize EBM's position on tonsillectomy (TTE).
In the “infectious model” of the disease:
- Recurrent acute tonsillitis is considered an indication for TE, but indications for “essential TE” vary - see Paradise criteria. “Chronic tonsillitis” is not a strictly determined concept, because The time factor in adults is difficult to take into account, but in children the period of onset of tonsillitis is more understandable.
- Peritonsillar abscess (it is better to use the differentiated concept of “peritonsillitis”, but it is not in ICD-10 - Yu.N.). Fine needle aspiration of the abscess contents may be sufficient. If there is effective anesthesia during the operation, in addition to puncture of the abscess, one-stage removal of the tonsils (abscess tonsillectomy) can be performed. The risk of postoperative bleeding is equal to traditional TE. Traditional TE in the treatment of peritonsillar abscess in the “era of antibiotics” is not strictly necessary.
- Infectious mononucleosis. TE is justified in cases of airway obstruction or tonsil bleeding. TE may shorten the duration of the disease, but compromises the immune system.
- Angina of Simanovsky-Plaut-Vincent. There is no data on TE, as well as on frequent sore throats of this kind.
- Sinusitis. There is no rigorous level A evidence.
- Bronchitis or cough. Not shown - strictly level A.
- Chronic otitis media with exudate. Some reviews contain the statement that in case of CSO, adenotomy is indicated, TE is not necessary.
Somatic local and systemic diseases:
- IgA nephropathy. TE has a positive effect (see picture above)
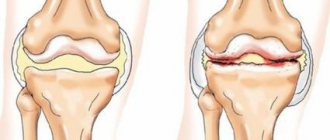
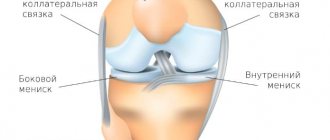
- Arthropathy (joint pain). The positive effect in children; in adults, the effect of TE has not been proven.
- Dermatoses. At the case-effect level: psoriasis, palmoplantar pustulosis.
- Intestinal diseases. TE has no effect in nonspecific ulcerative colitis or celiac disease. TE may be considered a risk factor for chronic intestinal diseases.
- Heart diseases. No Category A data.
- Vague fevers. There is no data in children, unlike adults, when after TE the risk of fever of “unexplained origin” decreases.
- Atopy
- Bronchial asthma. In children, TE does not affect the course of asthma or allergic rhinitis. There are no category A data for adults.
- Atopic diseases have never been a contraindication to TE. In adults, no connection was found.
"Unclassified indications":
- Malocclusion, cleft palate. There are no correlations. Indications for TE are determined individually.
- Halitosis. In some cases, TE reduces halitosis. There is no category A evidence.
- Hemorrhagic tonsillitis. Rarely seen in adults.
- In case of tumors, there is no need to discuss the advisability of TE. TE is considered as a biopsy option.
- Growth disorders – micrognathia (see picture above). Considered in the context of airway obstruction.
- Enuresis (bedwetting). The opinion about improving the quality of night sleep in enuresis after TE (considered last in the review by the authors) can be considered a “subtle German joke” based on isolated publications.
Individual states:
- Down syndrome. Macroglossia in hyperplasia of the palatine tonsils – in the context of respiratory disorders.
- Spindle cell anemia. Recurrent episodes of tonsillitis may be followed by hemolytic fever or another aplastic crisis. TE improves the condition of these patients.
- Cerebral paralysis. Limited indications for TE.
Thus, the indications for removal of the palatine tonsils are formulated quite clearly. An alternative is the method of “minimally invasive surgical treatment” of tonsillitis: in the presence of inflammatory cysts (the majority of them), limited in the volume of scar-inflammatory changes, less radical effects can be used. Vaporization (evaporation) using high-frequency electrocoagulators or lasers, argon plasma coagulation, etc. have become the most popular options for surgical treatment of patients with chronic tonsillitis.
Author of the article:
otorhinolaryngologist surgeon, professor, doctor of medical sciences Nazarochkin Yuri Valerianovich
Local complications
The development of local complications of tonsillitis, covering the ENT organs and respiratory system, is indicated by the addition of new symptoms, deterioration of health against the background of the beginning of recovery.
The most likely consequences of a sore throat are:
- Peritonsillar abscess
. This is the formation of an abscess in the tissue of the pharynx. It is manifested by the appearance of increasing pain on one side of the throat, a secondary increase in temperature, tension in the neck muscles, and difficulty swallowing. The patient cannot turn his neck normally and open his mouth completely. - Otitis
is an inflammation of the middle ear. It occurs both in parallel with a sore throat and a few days after the completion of the acute stage of tonsillitis. - Swelling of the larynx
. Occurs due to inflammation of the vocal cords. It manifests itself as hoarseness, difficulty swallowing and deterioration in breathing. - Inflammation of the lymph nodes
. The submandibular ones are most often affected, less often the clavicular and supraclavicular, cervical ones. - If left untreated, tonsillitis can also cause bronchitis, pneumonia, and tracheitis.
Classification
Acute tonsillitis (tonsillitis) or primary inflammation can occur in catarrhal, lacunar, follicular, and less often necrotic form. Secondary acute inflammation of the palatine tonsils most often occurs against the background of existing inflammatory or infectious diseases - scarlet fever, diphtheria, typhoid fever, mononucleosis, as well as leukemia,
Chronic tonsillitis is a long-term inflammatory process in the tonsils, with rare or constant relapses of the disease. Exacerbations can be caused by viruses or bacteria, or against the background of acute respiratory viral infections, dental diseases, or a general decrease in immunity.
Systemic complications
When a sore throat develops, an adult should always remember that failure to comply with treatment can lead to damage to:
- Hearts
. Sore throat often causes myocarditis and rheumatic damage to the heart muscle. Symptoms of complications may appear after 2-3 weeks. The main signs are arrhythmia, the appearance of increasing shortness of breath, swelling of the limbs, weakness, heart pain, and increased sweating. - Kidney
. The most likely complications of tonsillitis from the kidneys are pyelonephritis and glomerulonephritis. Renal pathologies are indicated by pain in the lumbar region, increased urination, swelling of the face and legs, lethargy, and irritability. - Sustavov
. After a sore throat, the possible development of rheumatoid arthritis. Symptoms are swelling and pain in the joints, redness of the skin where the limbs are flexed.
The most serious complications of tonsillitis are sepsis and toxic shock. They develop when bacteria spread throughout almost the entire body. The diseases are manifested by severe symptoms of intoxication, shortness of breath, difficulty breathing, and severe weakness. Treatment is carried out in intensive care conditions.
Prevention of complications after tonsillitis
To prevent the development of life-threatening complications, the patient should:
- Start drug therapy as early as possible from the onset of the disease.
- Use medications prescribed by your doctor for treatment. Antibiotics are prescribed to each patient individually, taking into account the sensitivity of pathogenic microorganisms to antibacterial agents.
- During the period of rising temperature, strictly adhere to bed rest.
- Drink as much as possible. Drinking large amounts of water and unsweetened compotes accelerates the removal of microbes and their toxins from the body.
If you have complications after a sore throat, you can contact our clinic for treatment. Qualified doctors will not only conduct a thorough diagnosis and identify the slightest undesirable changes, but will also correctly select medications taking into account the type of pathogenic microbes, the patient’s age and concomitant diseases.
After the main therapy, the clinic’s doctors also give their patients a list of recommendations, compliance with which will minimize the negative impact of tonsillitis on the body.
Diagnostics
Diagnosis of tonsillitis in children, as well as tonsillitis in adults, is carried out using the following methods:
- examination by an ENT doctor, collecting an anamnesis of the disease;
- throat swab for flora with determination of sensitivity to antibiotics and bacteriophages;
- general blood test, general urinalysis;
- blood test for antistreptolysin-O, rheumatoid factor, C-reactive protein;
- ECG;
- According to indications, ultrasound of the kidneys, Echo-CG, consultation with a cardiologist, urologist.