Osteomyelitis of the jaw is a dangerous inflammatory disease that is caused by infection. A purulent-necrotic process develops on the tooth bone - most often on the lower jaw. Next, the inflammation affects the bone tissue of the head and spreads to soft tissues - gums, salivary glands, skin, chewing and facial muscles. In severe cases, pus forms and necrosis of bone tissue occurs.
If the process turns into purulent inflammation of the soft tissues of the face, the patient suffers not only from local inflammation of the bone, but also from general intoxication.
Inflammatory processes in the mouth do not always develop into osteomyelitis. This disease most often affects people with weakened immune systems.
General information
Osteomyelitis of the mandible is more common, more severe and has more complications. With chronic osteomyelitis of the lower jaw, the bone is affected deeper, which can lead to jaw fractures. Inflammation affects a dangerous area - the jaw processes. Acute osteomyelitis of the lower jaw easily turns into subacute and then chronic.
Osteomyelitis of the upper jaw develops more rapidly and can lead to inflammation of the maxillary sinuses. However, since the bone tissue here is less dense, abscesses and phlegmons develop less often with osteomyelitis of the upper jaw, and the disease itself is easier.
The entry point for infection is a diseased tooth, and the causative agents of inflammation are Staphylococcus aureus and Staphylococcus alba, pneumococci, Escherichia coli and typhoid bacilli. This microflora is usually located in areas of chronic infection of the tissues surrounding the tooth.
Inflammation in osteomyelitis does not occur suddenly; initially, a chronic infection develops in the gum for a long time - for example, in periodontitis or periodontitis. Then, if the outflow of waste products from the infection is disrupted, the microflora from the lesion spreads to the surrounding tissue.
Osteomyelitis of other parts of the skeletal system is caused by only one type of pathogen - staphylococcus (streptococcus), which penetrates the tissue through the bloodstream. Since osteomyelitis of the jaw can be caused by different pathogens, the course of the disease has much more distinctive features than with ordinary osteomyelitis.
Osteomyelitis in dentistry
Osteomyelitis of the jaw bones accounts for approximately a third of all identified cases of this disease. This statistical feature is not accidental and is determined by the presence of teeth, which are often a source of infection of bone tissue. In addition, there are a number of features in the jaw that predispose to the development of such a disease:
- a very abundant network of arterial and venous vessels in the maxillofacial region;
- active growth of the jaw and rapid changes in its structure during the period of replacement of milk teeth with permanent ones;
- the presence of relatively wide Haversian canals;
- very thin and delicate bone trabeculae;
- high sensitivity of myeloid bone marrow to infection.
All this leads to the fact that the penetration of almost any microorganism deep into the bone tissue provokes the development of osteomyelitis.
Classification
Osteomyelitis of the jaws (photo) is classified according to several parameters.
Osteomyelitis may be caused by:
- Infectious
a) Single-gene. It is a consequence of dental disease - caries, stomatitis. The most common type of pathology accounts for 75% of all cases of osteomyelitis.
c) Non-odontogenic (hematogenous). The pathogen enters the bloodstream from other foci of infection. May be a consequence of chronic tonsillitis, diphtheria, scarlet fever.
- Non-infectious (traumatic). The result of mechanical damage to the jaw or a wound through which infection enters. Osteomyelitis can occur under the influence of a growing malignant tumor or become a complication after dental surgery. For example, if the nerve tissue is not carefully removed from the tooth socket.
According to the course of the disease, osteomyelitis of the jaw occurs:
- Spicy. It lasts 7–14 days, then passes into the subacute stage - when a fistula forms at the site of inflammation and exudate flows out from the site of inflammation.
- Chronic. Lasts from a week to several months. It ends with the rejection of dead bone areas through the fistulous tract. Treatment at this stage is mandatory.
- Subacute. The transitional form between acute and chronic disease lasts 4–8 days. The painful signs subside, but the infection is actively spreading.
According to the location of the pathology:
- Osteomyelitis of the upper jaw.
- Osteomyelitis of the lower jaw.
By coverage:
- Limited. The inflammation covers the alveolar process or the area of 2–4 teeth of the jaw.
- Diffuse. The pathology covers most or all of the jaw.
According to clinical and radiological forms, chronic odontogenic osteomyelitis is:
- productive. During the healing process, it does not form sequesters (dead bone areas);
- destructive. Upon recovery, it forms sequesters.
- destructive-productive.
Preventive actions
Prevention is important not only to prevent the development of purulent inflammation, but also to minimize the likelihood of complications. With the help of preventive measures, you can also speed up rehabilitation if it was not possible to prevent the disease:
- Timely elimination of carious formations, even if there are no clinical symptoms.
- Sanitation of various foci of infection.
- Physical activity, a balanced and nutritious diet, which contribute to the effective functioning of the immune system.
- Compliance with the doctor’s recommendations after injury, during recovery after surgery or tooth extraction.
In conclusion, I would like to emphasize that although modern medicine has made great progress, osteomyelitis of the jaw bone still remains a serious problem. Thanks to the timely detection of symptoms of pathology and proper treatment, it is possible to significantly increase the likelihood that the patient will be able to fully recover and the quality of his future life will not be affected.
Causes of osteomyelitis of the jaw
Odontogenic osteomyelitis is caused by advanced diseases of the oral cavity. The infection penetrates into the bone tissue through the affected pulp or tooth root. Among the most common gates of infection are:
- caries;
- pulpitis;
- periodontitis;
- pericoronitis;
- alveolitis;
- granuloma or dental cyst.
With hematogenous osteomyelitis, infection through the bloodstream can come from abscesses on the neck or face (boils, carbuncles) or result from:
- purulent otitis;
- tonsillitis;
- umbilical cord infections in infants;
- inflammatory foci in diphtheria and scarlet fever.
With traumatic osteomyelitis, the infection from the external environment enters the open wound, then into the bone tissue. This may happen:
- with a gunshot wound;
- jaw fracture;
- damage to the nasal mucosa.
If a person has good immunity, his body successfully resists the invasion of pathogenic bacteria and in 60% of cases can prevent the development of the disease. If the patient suffers from chronic ailments - diseases of the blood, liver, kidneys, endocrine system, arthritis and polyarthritis, he will most likely develop osteomyelitis of the jaw.
What causes the disease
The main culprit of the disease is pathogenic microorganisms. These are mainly streptococci and anaerobic bacteria that are present in the human oral cavity. They are the ones who trigger the infectious process that affects the jaw. But how do pathogenic bacteria get into bone tissue? There are several ways:
- An advanced carious process that has destroyed the hard tissues of the tooth and reached the pulp.
- Tooth injury – crack, filling defect, fracture. But not every mechanical damage will become a source of infection. The damage must be serious and deep. This also includes a broken jaw. But in this case, the inflammation is usually caused by a staphylococcal infection.
- Chronic infectious focus in another organ. Harmful bacteria can make their way to the jaw through the lymph nodes or blood vessels from a nearby organ (ear, throat, nose).
Most often, the disease is diagnosed in the lower jaw, since the teeth of the lower row are more susceptible to caries and various traumatic effects.
The risk of developing osteomyelitis increases in the presence of an immunodeficiency state, as well as diseases of the circulatory system. This is due to the fact that a person with such pathologies has poor wound healing, and the body is not able to resist infections.
Other factors provoking the disease include:
- smoking;
- alcohol abuse;
- diabetes;
- fasting or poor nutrition;
- syphilis;
- chemotherapy courses.
If the acute development of the disease is not completely cured, then chronic osteomyelitis of the jaw develops. It is more difficult to respond to conservative therapy and also more often leads to complications.
Symptoms of osteomyelitis of the jaw
At the initial stage, osteomyelitis of the jaw has no characteristic signs. The person feels unwell, as with most inflammatory diseases. Unaware of the real cause of poor health, the patient may assume another disease and self-medicate. Not only will this not help, but it will also delay the moment of recovery. Therefore, if you feel unwell, it is important to consult a doctor.
External symptoms of maxillary osteomyelitis:
- General weakness, sweating, headache. The person is depressed, he sleeps poorly, refuses to eat.
- Depending on the type of infection and the patient’s immunity, the body temperature rises to 38 or higher or remains normal. If there is no temperature, then the body is not fighting the infection.
- In the acute form of odontogenic osteomyelitis, the tooth affected by the infection hurts. The pain intensifies with pressure and is not relieved by taking painkillers. The tissue around the tooth is swollen and has a reddish tint. Not only the diseased tooth moves, but also those nearby.
- Sometimes an abscess develops on the periosteum of the tooth root. Inflammation affects neighboring teeth, and acute pain shoots into the ear, temple and eye area.
- With osteomyelitis of the lower jaw, the lower lip, mouth and chin become numb. When inflammation invades the jaw tissue, pain spreads throughout the face and neck. The submandibular and cervical lymph nodes become enlarged and painful.
- A periodontal pocket filled with pus forms in the space between the tooth and gum.
Symptoms of acute osteomyelitis of the jaw:
- it hurts to chew;
- at the site where the infection develops, the skin turns pale and becomes covered with plaque;
- the sclera of the eyes turn yellow;
- blood pressure surges;
- with osteomyelitis of the lower jaw, part of the lower lip becomes numb and stops moving, this is due to the fact that the source of inflammation compresses the alveolar nerve.
In subacute osteomyelitis, the inflammatory process continues and sequestration is formed. The teeth in the affected jaw retain and even increase mobility.
With chronic osteomyelitis, the patient feels satisfactory. During remission, the pain subsides. However, the following warning signs remain:
- lack of appetite;
- poor sleep;
- soreness of the facial skin;
- lymph nodes are enlarged;
- fistulas in the mouth do not heal, pus is regularly discharged from them;
- the mucous membranes of the mouth are swollen;
- The teeth on the affected jaw are mobile, and their mobility increases over time.
During an exacerbation, the patient again feels pain spread throughout the jaw and cannot always accurately indicate the location of its localization.
Infants and young children can also develop osteomyelitis of the jaw (usually the upper jaw). The disease develops against the background of sepsis or becomes a complication of ARVI. The symptoms of osteomyelitis in children are pronounced; the disease progresses rapidly and can lead to severe complications, including pneumonia and meningitis. Therefore, it is important to consult a doctor as soon as possible and begin treatment if your baby has the following symptoms:
- high temperature that cannot be reduced with antipyretic drugs;
- cheeks, eyes, lips swell, facial asymmetry appears, it is difficult for the child to open his eyes, and the swelling of the nose makes it difficult to breathe. If you do not see a doctor, the swelling spreads to the neck;
- lymph nodes enlarge;
- purulent foci are noticeable on the gums, and over time infiltrates and fistulas open;
- pain in the eye area.
Treatment with folk remedies at home
It is important to remember that osteomyelitis is a severe purulent disease and it is impossible to cure it at home only with folk remedies or homeopathic preparations!
It is better to use traditional medicine recipes in the recovery stage, when acute inflammatory phenomena have gone away. For example, mumiyo is a powerful natural stimulant. This remedy promotes rapid healing of wounds and restoration of damaged tissue. For osteomyelitis, prepare a solution from 2 g of mumiyo and a glass of warm boiled water. Take this medicine one tablespoon in the morning and evening.
In order for the fistula tracts to heal faster, you can rinse your mouth with a solution of propolis tincture. To do this, place a small piece of propolis in a dark thick glass bottle and pour 200 ml of good vodka. The bottle is tightly closed and left in the refrigerator for 2 weeks. To prepare the solution, 7-10 drops of tincture are dissolved in a glass of boiled water and used to rinse the mouth 2-3 times a day.
Even ordinary table salt can treat osteomyelitis. To do this, dissolve a teaspoon of salt in a glass of water and rinse your mouth after each meal.
Treatment of osteomyelitis with herbs is justified. Many medicinal plants are natural antiseptics, immunostimulants, they promote wound healing and the prevention of complications. At home, you can prepare herbal decoctions (chamomile, calendula, string, nettle) and rinse your mouth with them until all fistulas heal.
Comfrey ointments are widely used for the treatment of osteomyelitis. To prepare such a product, take 160 grams of fresh lard per 40 grams of dry crushed plant roots. Mix everything and boil in a water bath for 2 hours. The mixture is infused for a day and filtered to remove any solid residues. The resulting ointment is applied to the skin over the affected area until complete recovery.
The following micropreparations can be used from homeopathic remedies for the treatment of osteomyelitis:
- Acidum fluoricum,
- Mercurius solubilis,
- Stillingia,
- Aronea diadem,
- Aurum muriaticum,
- Strontium carbonicum.
In any case, the correct treatment for such a disease should be selected by a homeopathic physician, taking into account the individual characteristics of the patient.
Separately in non-traditional methods of treatment is the drug ASD or Dorogov’s antiseptic stimulant. This product is a product obtained from animal raw materials by thermal decomposition. It has antiseptic, immunomodulatory and stimulating properties, which have been proven in animals in which experimental osteomyelitis was induced. To treat osteomyelitis, its second fraction or ASD 2 is used. The drug is used orally, for which 15 drops of it are dissolved in 100 ml of chilled boiled water and drunk either 30-40 minutes before meals, or no earlier than 2 hours after meals. Course treatment: 5 days with three-day breaks until final recovery.
Diagnostics
Osteomyelitis cannot go away on its own; without medical help, the patient’s condition will worsen.
Periodontitis, cysts and tumors of the jaw, as well as lesions of oral tissue due to syphilis, tuberculosis, and fungal skin infections have similar symptoms. Therefore, self-diagnosis is highly not recommended.
When visiting the clinic you must:
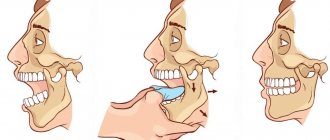
- Undergo an initial examination of the jaw by a dentist. With osteomyelitis, tapping and palpating the affected areas will be painful.
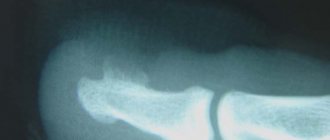
- Take an x-ray. In the acute form, it is not very informative, but in subacute and chronic pathology, areas of change in bone density and areas of dead bone tissue will be noticeable.
- Take a general urine and blood test, a biochemical blood test, and bacteriological culture to identify the type of pathogenic microorganisms.
- Get a CT scan.
Treatment of osteomyelitis of the jaw
Treatment of osteomyelitis of the jaw is complex and consists of surgery, drug treatment and restorative therapy, which promotes tissue regeneration.
During surgery:
- the surgeon removes the affected tooth;
- treats fistulas and boils in the oral cavity;
- drains pus;
- removes dead (sequestered) areas of bone;
- fills hollow areas with bone materials;
- strengthens mobile teeth with splints.
At the same time, drug treatment is carried out:
- antibiotics;
- immunostimulants;
- vitamin complexes.
To consolidate the result, you must undergo a course of physical procedures:
- UHF;
- magnetic therapy;
- ultrasound therapy.
During the treatment process, the patient is prescribed plenty of fluids and a gentle diet of light, crushed and nutritious foods. It is necessary to carefully monitor oral hygiene.
Desensitization therapy
The treatment complex is supplemented with antihistamines:
- diphenhydramine;
- chloropyramine;
- fenkarol;
- diazolin.
Medicines help eliminate intoxication, activate the anti-inflammatory functions of antibiotics, minimize the permeability of the vascular wall, and fight swelling. To increase the effect, drugs containing calcium and glucose are prescribed in combination.
This treatment protocol is used for patients with diabetes, since this approach minimizes the negative impact of concomitant disorders in the foci of infection and facilitates the recovery process.
General restorative therapy
As part of a general strengthening course, the patient is prescribed vitamin complexes (groups B, C), adaptogenic drugs, and stimulants.
In severe forms of the disease, extracorporeal detoxification is performed. For this purpose, hemosorption, plasmapherosis or lymphosorption are prescribed. Courses of autohemotherapy (administration of one’s own venous blood intramuscularly) have a positive effect.
Physiotherapy
Such treatment is allowed only after acute inflammatory symptoms have reduced, so manipulations are prescribed a few days after the start of therapy. The methods may be as follows:
- hardware treatment with UV rays;
- electrophoresis using anti-inflammatory and antibacterial drugs;
- massage;
- oxygenation;
- laser irradiation of the site of the extracted tooth.
Regardless of the course of the disease, the treatment protocol is determined only by the doctor, taking into account the physiological characteristics of the body.
Forecast and prevention of osteomyelitis of the jaw
If the patient sought medical help on time, followed the doctor’s recommendations and received the correct treatment in full, osteomyelitis will be successfully cured. Incorrect treatment in combination with a weakened immune system can lead to the following complications:
- sepsis;
- acute purulent inflammation;
- general intoxication;
- the formation of multiple abscesses;
- meningitis;
- inflammation of the facial nerves;
- bone deformities;
- purulent sinusitis and destruction of the walls of the maxillary sinuses;
- infection of the orbit and formation of phlegmon;
- jaw fractures.
To prevent osteomyelitis of the jaw, it is important to:
- Have dental checkups every year.
- Properly brush your teeth, maintain oral hygiene, and use interdental floss and rinses.
- Treat teeth and gums in a timely manner.
- Protect your jaw from injury.
- Strengthen immunity.
- Do not start treatment for infectious diseases, including tonsillitis and ARVI.
Prognosis and possible complications
With timely consultation with a doctor, accurate diagnosis and properly selected therapy, the prognosis is favorable.
Otherwise, the pathological process can spread along the descending and ascending paths. This threatens the development of the following complications:
- Meningitis
- Brain abscess.
- Phlegmon of the orbit.
- Sinusitis.
- Thrombophlebitis of the facial vein.
- Sepsis.
- Lung abscess.
- Mediastinitis.
These conditions have an acute onset and require immediate medical attention. Delay often ends in death for the patient.
The chronic form with sluggish inflammation negatively affects the condition of the soft tissues and bones of the jaw, and is accompanied by:
- fractures,
- deformation of the temporomandibular joint;
- formation of intra-articular adhesions;
- the formation of scar contractures of the masticatory muscles.
These pathologies significantly limit the mobility of the jaw or lead to its complete immobility.