A benign bone tumor is called osteoblastoma. More often it occurs at an early and young age, in boys, teenagers and men under 30 years of age. Women suffer from this tumor disease less often.
Our expert in this field:
Akhov Andemir Olegovich
Traumatologist-orthopedist, oncologist. Member of the Russian Society of Clinical Oncology RUSSCO
Call the doctor Reviews about the doctor
After 30 years, the likelihood of developing osteoblastoma decreases, but its danger increases. Now it can be an aggressive tumor, growing rapidly, with a serious risk of malignancy - degeneration into osteogenic sarcoma.
The causes of osteoblastoma are unclear. A significant role can be played by a genetic (hereditary) factor, frequent trauma, inflammatory diseases of bone and connective tissue.
Osteoblastoma cannot be cured. It can either be removed or left alone and observed.
Make an appointment with a doctor now
Message sent!
expect a call, we will contact you shortly
What it is
Osteoblastoma is a group of benign neoplasms localized on the bone. The pathology is not common and occurs in rare cases.
Osteoblastomas are benign tumors that affect the bone. The manifestation of symptoms depends on the location of the neoplasm.
For diagnosis, extended radiography, computed tomography and magnetic resonance imaging are used. Treatment is only surgery.
Diagnosed at the age of under 30, under the influence of unfavorable factors it retains a tendency to degenerate. Osteoblastoma is common among males.
Women suffer less frequently, but the course of the disease is complicated. Pregnancy and hormonal imbalance increase the likelihood of tumor malignancy.
Kinds
There are two main types of the disease.
Bizarre
The tumor is characterized by a large number of multinucleated cells. Not dangerous to humans, prognosis is favorable. The formation is identified by x-ray.
Aggressive
Occurs within 2 years after removal of the formation and degenerates into a malignant tumor. A distinctive feature of the tumor is clear contours. Education is common among the male half.
Comprehensive diagnostic measures and the patient’s medical history will help determine the type of tumor process. If there is information about a previously removed osteoblastoma, the doctor makes a diagnosis of an aggressive form of formation.
In two thirds of cases, the disease is diagnosed in men. Age of onset: 20-30 years. Malignant osteoblastomas are characterized by aggressive growth with more frequent cases of relapse.
Oncologist, mammologist, chemotherapy
Butsyk Natalya Gennadievna
32 years of experience
Provoking factors
The development of a benign neoplasm is due to a number of provoking factors. The underlying causes of the tumor:
- mechanical damage;
- genetic predisposition;
- systematic impact on a specific area;
- congenital pathologies;
- inflammatory processes;
- infectious diseases;
- lack of timely treatment for inflammatory processes in the oral cavity;
- rheumatism;
- advanced form of syphilis;
- disorder .
People with weakened protective functions of the body are at risk. Constant colds and inflammatory diseases increase the likelihood of a benign neoplasm. Receiving the same injury is dangerous due to the development of a tumor-like process.
Osteoblastoma manifests itself at a young age and, without treatment, grows rapidly.
Aggressive osteoblastoma of the mandible: diagnostic difficulties
Osteoblastoma is a benign tumor that accounts for less than 1% of all bone tumors and most often affects the spine and sacrum of patients at a young age. Less than 10% of all osteoblastomas are located on the skull, and approximately half of them involve the mandible, especially its posterior segments. The very first detailed description of a case of osteoblastoma of the jaw bones was carried out by Borello and Sedano in 1967.
Since the discovery of the tumor by Jaffe and Mayer in 1932, the nomenclature of osteoblastoma has changed dramatically. Names proposed include osteoblastic osteoid-forming tumor, giant osteogenic fibroma, and giant osteoid osteoma. In 1956, this neoplasm was clearly distinguished from osteoid osteoma and identified by Jaffe and Lichtenstein as a separate nosological form: benign osteoblastoma. This name has been approved by the World Health Organization and the Institute of Pathology.
This bone tumor occurs at a young age (on average 20 years) in men and women in a ratio of 2:1. Clinically, the disease is characterized by severe pain lasting from several weeks to a year or more. Radiologically, the tumor may begin to appear as a radiolucent area with poorly or well-defined edges and varying degrees of mineralization. Although the use of radiological examination is very important, the final diagnosis is made only after a histopathological report.
This article describes a case of aggressive osteoblastoma in the posterior segment of the mandible in a 26-year-old woman.
Description of a clinical case.
A 26-year-old woman came to the clinic with complaints of a slowly growing painful swelling in the right posterior part of the lower jaw, which had been developing over the past 3 years. The pain is moderate and intermittent. An external examination revealed a swelling with a smooth surface measuring 3 x 3 cm, affecting the right part of the body of the lower jaw approximately from the symphysis of the chin to the second lower molar on the right side and causing pronounced facial asymmetry. Intraoral examination is unremarkable, the mucous membrane over the swelling is not changed. No lymphadenopathy was detected by palpation.
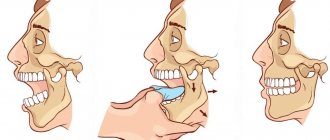
An orthopantomogram reveals a large radiolucent zone affecting the second lower molar on the right side. The formation contains calcified masses approaching the distal root of the second molar, as well as several radiopaque areas located against the background of the clearing zone. This formation was well defined and caused bulging and thinning of the bone tissue of the lower edge of the lower jaw. (Photo 1).
Photo 1: Orthopantomogram. Large single-cavity radiolucent lesion involving the right mandibular second molar, with areas of mineralization
Differential diagnosis included cementoblastoma, osteoid osteoma, ossifying fibroma, and focal cemento-osseous dysplasia.
Subsequently, the tumor was scraped out. The removed tissue, as well as the second molar, was sent for histopathological examination (Figure 2).
Photo 2: Photograph of tissue sample: material obtained after curettage and lower second molar
Light microscopy of the hematoxylin-eosin-stained specimen revealed an irregular bone structure with many cells and loose fibrovascular connective tissue stroma. A large number of areas of osteoid and cementoid formations were also found. The bone was composed of large osteocytes surrounded by a clear rim of osteoblasts (Figure 3a and b). Along the edge of the neoplasm, mature trabeculae are visible, clearly delimited from the rest of the tissue by a demarcation line. The specimen contained giant cells with several nuclei. No atypical mitotic activity was detected.
Figure 3a: Photomicrograph of specimen showing irregular bone, rims of osteoblasts and fibrovascular connective tissue stroma (hematoxylin-eosin, x100)
Figure 3b: Photomicrograph of a specimen showing large osteocytes, modified osteoblast-like cells, surrounded by osteoid substance. (hematoxylin-eosin, x400)
Histopathological examination allowed a diagnosis of aggressive osteoblastoma.
Discussion.
Osteoblastoma is a fairly rare bone tumor for which damage to the jaw bones is not typical. However, cases of its occurrence in the posterior part of the lower jaw have been described. Differential diagnosis is often particularly difficult due to the unclear radiological and clinical appearance, as well as the histological features of this tumor, which sometimes resemble osteosarcoma.
Typical osteoblastomas are biologically benign and limited in growth, typically no more than 4 cm in diameter. But there is also a small group of borderline, more aggressive osteoblastomas. Such tumors cannot be classified as “typical” and are therefore classified as a separate class of lesions with the names: osteoblastoma-like osteosarcoma, malignant osteoblastoma, or aggressive osteoblastoma.
Aggressive osteoblastomas occur at a later age than tumors with a benign course. Clinically, these neoplasms exhibit more aggressive behavior. They can grow into neighboring tissues, and after treatment they recur in 10-21% of cases, but never metastasize. The histological picture is more reminiscent of osteosarcoma than a benign neoplasm. Some authors have stated that the disease called aggressive osteoblastoma is actually a high-grade osteosarcoma that resembles the course of osteoblastoma. Diagnosis is based on the histological features and clinical picture of the lesion.
Differential diagnosis is carried out with a wide variety of diseases, such as cementoblastoma, osteoid osteoma, fibrous dysplasia, ossifying fibroma, focal cemento-osseous dysplasia, as well as borderline malignant forms of the above pathologies and slowly progressing osteosarcoma.
Benign cementoblastoma is included in the differential diagnosis due to similar radiographic findings with osteoblastoma. The main distinctive features of cementoblastoma are revealed by careful examination of the surface of the tooth root on an x-ray, and it is also believed that the affected area by cementoblastoma looks more uniform in shadow. In this clinical case, the tumor masses did not affect the tooth, despite its very close location to it. Microscopically, these two diseases look the same, so the final diagnosis of cementoblastoma cannot be made until the fact of tooth damage is confirmed.
Another difficulty is confusing osteoblastoma with osteoid osteoma. Clinically, benign osteoblastoma does not usually cause the pain that is characteristic of osteoid osteoma. Also, osteoblastoma is a fairly large neoplasm, usually about 1 cm in diameter, and does not cause sclerosis of bone tissue, which is again characteristic of osteoid osteoma. Microscopically, the bone trabeculae of osteoblastoma are slightly wider than those of osteoid osteoma and also have a more regular orientation. Osteoblastoma has a huge number of osteoblasts, while osteoid osteoma has few giant cells and poor vascularity.
Histopathologically, ossifying fibroma and fibrous dysplasia of bone may resemble osteoblastoma, but they are typically less mineralized and mildly calcified in contrast to the large mineralized fragments of osteoblastoma. In addition, fibrous dysplasia does not appear as demarcated radiographically as osteoblastoma and may also be multifocal, which is uncommon in osteoblastoma.
Focal cemento-osseous dysplasia is a fibro-osseous lesion that may appear very similar to osteoblastoma on radiographs. However, the former is typically asymptomatic and does not damage the cortex. Most of these formations are less than 1.5 cm in diameter. Although, upon microscopic examination, both pathologies damage bone tissue in a similar way. In focal cemento-osseous dysplasia, a small number of large and actively proliferating osteoblasts are determined.
Histological examination is of paramount importance in making a final diagnosis and excluding osteosarcoma, especially the osteoblastic variant. The difficulty in distinguishing arises from the presence in osteoblastoma of modified osteoblast-like cells, similar to atypical osteosarcoma cells. In such cases, diagnosis is based on accurate interpretation of histological and radiological studies, the findings of which exclude aggressive characteristics of osteosarcoma. Bertoni and other scientists believe that the main microscopic feature that distinguishes osteosarcoma from osteoblastoma is the small number of mature trabeculae at the edge of osteosarcoma and the high penetration of this tumor into surrounding tissues.
Due to the benign nature of osteoblastoma, the main treatment is conservative excision, since recurrence is rare (13.6%) and is usually associated with a complicated course. It should also be noted that there is no uniform description of the biological behavior of this tumor. Looking at the various study reports, it becomes clear that the course of this disease varies greatly depending on the specific clinical case.
Conclusion.
The importance of the clinician understanding the tumor process and its individual course should be especially emphasized. To make a final diagnosis, it is necessary to take into account clinical and radiological data in strict conjunction with the results of histological examination. At the same time, the entire pathology must be qualitatively classified and segmented to facilitate diagnosis and prescribe appropriate, strictly specific treatment.
Authors: Harshaminder Kaur, Sonika Verma, Manveen K. Jawanda, Atul Sharma Department of Oral and Maxillofacial Pathology, College of Dental Research, Mullana, Haryana, India
Symptoms
Clinical manifestations of the disease depend on the location of the tumor. Generalized symptoms include dull pain and the appearance of a lump. It can be independently identified through a thorough examination.
Spinal osteoblastoma
Damage to the spinal column is recorded in 50% of all cases.
There are no clinical manifestations. As the formation grows, the first symptoms are observed. The patient complains of dull pain in the spine, motor activity is reduced.
The presence of a foreign body is felt. The clinical picture is due to the growth of the tumor and the formation of a dense node.
Osteoblastoma of the jaw
Pathological growth is discovered accidentally during a routine X-ray of the oral cavity. The tumor is localized in the lower part of the jaw and covers the bone structures. Pain occurs when pressure is applied to the formation. The nature of the pain is similar to inflammatory damage to the trigeminal nerve.
Osteoblastoma of the skull
Identified by magnetic resonance imaging. Systematic nosebleeds indicate tumor growth. As the formation increases, epileptic seizures are observed.
Why can our articles be trusted?
We make health information clear, accessible and relevant.
- All articles are checked by practicing doctors.
- We take scientific literature and the latest research as a basis.
- We publish detailed articles that answer all questions.
This is due to compression of parts of the brain. The patient complains of decreased vision and hearing. The tumor process negatively affects the emotional state of the patient.
General clinical picture
The patient complains of prolonged pain (depending on the location of the formation). The symptom intensifies at night, which negatively affects a person’s rest.
The general condition is depressed, there is constant fatigue and weakness. Muscle weakness is possible, the person is not able to cope with his usual activities.
Indications for surgery
Osteoblastoma is removed in case of its rapid, aggressive growth, risk of malignancy, compression of neighboring organs, vascular or nervous structures due to the large size of the tumor, bone deformation, severe symptoms.
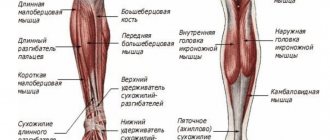
A benign tumor can occur on any bone, in any place, but in 50% of cases this place is the spine. By compressing the spinal nerve root, osteoblastoma causes pain, ranging from moderate, aching, constant to acute. Other symptoms of a spinal tumor are associated with radicular syndrome - muscle weakness in the arm or leg, sensory disturbances, numbness, paresis.
A tumor of the facial bone often leads to a pronounced aesthetic defect. If it compresses a blood vessel, blood circulation is disrupted, and if it presses on a nerve, neuralgia occurs (in particular, trigeminal neuralgia with unbearable pain).
One example of facial osteoblastoma is a tumor of the lower jaw, which can cause tooth loss, inflammation, skin ulcers, purulent fistulas, and facial asymmetry.
If the tumor has affected the skull bone, it manifests itself as headache, memory loss, vision impairment, epileptic seizures, nosebleeds, and hormonal imbalance. Osteoblastoma in the sinus impairs breathing and vision.
A tumor of the femur is manifested by lameness, nagging pain in the muscle, which intensifies when walking.
If osteoblastoma occurs in the joint area, its movements are impaired. For example, a large tumor in the shoulder joint makes it impossible to move the arm. Tumors on the bones of the fingers disrupt their function and are accompanied by local inflammation, pain, burning, weakness and muscle atrophy.
These and other pronounced symptoms of osteoblastoma are indications for surgery.
Our doctors will help you
Message sent!
expect a call, we will contact you shortly
Diagnostics
Enhanced radiography will help determine the presence of a pathological process. The procedure is carried out depending on the location of the tumor. The image characterizes the formation: size, structure, location.
To determine the type of tumor process, a biopsy is indicated. The procedure involves taking tissue from the affected area. In laboratory conditions using reagents, specialists determine the type of formation (benign or malignant).
For small formations, radiography is uninformative. To obtain information about the type of growth, the patient undergoes an advanced computed tomography or magnetic resonance imaging scan.
Treatment
Therapeutic tactics depend on the type of formation and its location. Therapy consists of surgical excision of the tumor. Medication treatment is not carried out due to lack of effectiveness.
Self-medication is dangerous with complications!
Attention
Despite the fact that our articles are based on trusted sources and have been tested by practicing doctors, the same symptoms can be signs of different diseases, and the disease may not proceed according to the textbook.
Pros of seeing a doctor:
- Only a specialist will prescribe suitable medications.
- Recovery will be easier and faster.
- The doctor will monitor the course of the disease and help avoid complications.
find a doctor
Do not try to treat yourself - consult a specialist.
Indications for surgical intervention:
- disruption of vital functions of the body due to the rapid growth of the tumor;
- discomfort (if localized in the oral cavity, the tumor affects the quality of life);
- mutation process accompanied by deformation of bone structures;
- rapid growth in education;
- high probability of malignancy.
Intensive spread of the tumor is dangerous due to its degeneration. In case of a malignant course, the probability of damage to neighboring organs and systems remains.
Surgery is performed in two ways: traditional and using a laser. In the first case, the formation is excised along with healthy tissue, which minimizes the likelihood of relapse. The operation is performed under general anesthesia.
Removal of formations using laser therapy - a modern bloodless technique. The tumor is burned out with high precision, without causing discomfort or bleeding. It is performed under local anesthesia and is used for small formations.
After removal of the formation, the patient must undergo preventive examinations. This action is aimed at timely detection of deviations and prevention of relapse.
Forecast
Detection of pathology at an early stage of development increases the likelihood of a favorable prognosis. When a relapse occurs, a positive outcome is recorded in 20% of cases.
An unfavorable prognosis is typical for formations in the oral cavity and inside the skull. The risk of death remains. In the absence of therapy in the early stages of development, the likelihood of osteosarcoma (bone cancer) developing is 25%.
The favorable prognosis depends on the patient himself. The sooner a person seeks help, the sooner he will receive help.
Prices
| Disease | Approximate price, $ |
| Prices for thyroid cancer screening | 3 850 — 5 740 |
| Prices for examination and treatment for testicular cancer | 3 730 — 39 940 |
| Prices for examinations for stomach cancer | 5 730 |
| Prices for diagnosing esophageal cancer | 14 380 — 18 120 |
| Prices for diagnosis and treatment of ovarian cancer | 5 270 — 5 570 |
| Prices for diagnosing gastrointestinal cancer | 4 700 — 6 200 |
| Prices for breast cancer diagnostics | 650 — 5 820 |
| Prices for diagnosis and treatment of myeloblastic leukemia | 9 600 — 173 000 |
| Prices for treatment of Vater's nipple cancer | 81 600 — 84 620 |
| Prices for treatment of colorectal cancer | 66 990 — 75 790 |
| Prices for treatment of pancreatic cancer | 53 890 — 72 590 |
| Prices for treatment of esophageal cancer | 61 010 — 81 010 |
| Prices for liver cancer treatment | 55 960 — 114 060 |
| Prices for treatment of gallbladder cancer | 7 920 — 26 820 |
| Prices for treatment of stomach cancer | 58 820 |
| Prices for diagnosis and treatment of myelodysplastic syndrome | 9 250 — 29 450 |
| Prices for leukemia treatment | 271 400 — 324 000 |
| Prices for thymoma treatment | 34 530 |
| Prices for lung cancer treatment | 35 600 — 39 700 |
| Prices for melanoma treatment | 32 620 — 57 620 |
| Prices for treatment of basal cell carcinoma | 7 700 — 8 800 |
| Prices for the treatment of malignant skin tumors | 4 420 — 5 420 |
| Prices for treatment of eye melanoma | 8 000 |
| Prices for craniotomy | 43 490 — 44 090 |
| Prices for thyroid cancer treatment | 64 020 — 72 770 |
| Prices for treatment of bone and soft tissue cancer | 61 340 — 72 590 |
| Prices for treatment of laryngeal cancer | 6 170 — 77 000 |
| Testicular cancer treatment prices | 15 410 |
| Bladder cancer treatment prices | 21 280 — 59 930 |
| Prices for cervical cancer treatment | 12 650 — 26 610 |
| Prices for treatment of uterine cancer | 27 550 — 29 110 |
| Prices for treatment of ovarian cancer | 32 140 — 34 340 |
| Prices for treatment of colon cancer | 45 330 |
| Prices for lymphoma treatment | 11 650 — 135 860 |
| Prices for kidney cancer treatment | 28 720 — 32 720 |
| Prices for breast reconstruction after cancer treatment | 41 130 — 59 740 |
| Prices for breast cancer treatment | 26 860 — 28 900 |
| Prices for prostate cancer treatment | 23 490 — 66 010 |
Prevention
There are no specific preventive measures. A systematic examination of the body will help prevent the development of a tumor. Doctors recommend carefully monitoring your health and not ignoring negative symptoms.
A complete examination of the body minimizes the risk of serious illness. If the skin is systematically damaged and a lump appears, it is advisable to consult a doctor. Timely therapy will help avoid serious complications and the spread of the malignant process.
Osteoblastoma is a benign neoplasm with a tendency to malignancy. It is characterized by a dull pain localized in the area of compaction. Diagnosed using radiography or computed tomography.
Timely therapy minimizes risks and tumor degeneration. The formation is removed through surgery or laser therapy. The method of exposure is determined by the doctor based on the general condition of the patient and the type of tumor process.
Minimally invasive surgeries
If the osteoblastoma is small, it can be removed endoscopically. In this case, no incision is made, but surgical instruments and an endoscope are inserted through small punctures. This allows you to reduce tissue trauma and speed up rehabilitation after surgery.
Tumor removal is performed under visual control using a miniature endoscope video camera and ultrasound guidance. High precision is required from the surgeon. This presupposes extensive experience in performing such operations and appropriate qualifications, which the specialists of the international clinic Medica24 certainly possess.
Small osteoblastoma (up to 5 cm) can be removed using a laser. This method eliminates bleeding and damage to adjacent tissues. A laser light guide is inserted through a puncture of the skin and brought to the tumor under CT control.
Another option is radiofrequency ablation. In this case, an electrode is inserted into the tumor body, to which an electric current of a certain frequency is applied. This causes rapid heating of the osteoblastoma and its destruction. High precision of guidance is ensured by computed tomography.
The material was prepared by oncologist, traumatologist-orthopedist of the international clinic Medica24 Andemir Olegovich Akhov.