Polyosteoarthrosis of the hands is a frequently detected disease in older people and in representatives of certain professions whose work involves exposure to negative factors on the fingers. More often than others, seamstresses, cutters, cooks, hairdressers, laundresses, and finishers suffer. Anyone who is forced to use fine motor skills of their hands for a long time or keep them in a cold, aggressive environment suffers to one degree or another from the destruction of cartilage tissue inside the joints.
The human hand is a unique articulation of bones, around which there is a huge number of muscles, ligaments and tendons. The hand is capable of performing hundreds of different movements. This is a unique instrument with which a person serves himself, draws, plays musical instruments, sews, produces various objects, etc. Fine motor skills in childhood are directly related to the functioning of the central nervous system. It is a widely known fact that in infancy, a child’s mental abilities can be significantly improved by engaging in activities that develop fine motor skills.
Unfortunately, this principle also works in old age, when polyosteoarthrosis of the joints of the hands develops - the less ability to perform minor operations, the faster the brain’s performance decreases. A person begins to suffer from memory lapses, the quality of his thinking process deteriorates, his logic is distorted, suspiciousness, irritability and other characteristic signs of hydrocyanic dementia appear. Therefore, it is very important to maintain your fine motor skills until old age and protect the joints of your hands from negative effects and destruction. And at the first symptoms of trouble, you should seek medical help.
In Moscow, you can make an initial free appointment with an orthopedist at our manual therapy clinic. Experienced doctors work here. They will be able to make an accurate diagnosis. If polyosteoarthrosis of the hands is detected at an early stage, the doctor will suggest an individual course of rehabilitation therapy. During the treatment, the pathological process will be stopped and you will regain the ability to perform all the usual movements with your hands.
Polyosteoarthrosis of the joints of the hands is a pathology of cartilage tissue. It develops very slowly. At the initial stage, it manifests itself as periodic pain in the interphalangeal joints. Then stiffness in movement may begin to appear. In advanced cases, the amplitude of mobility decreases sharply. When moving, clicks, crunching and other extraneous sounds appear. The joints become deformed and lose all their functionality.
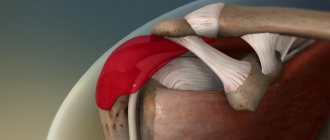
Joints are movable joints of bones that provide the ability to perform various movements. In the hands, the individual phalanges of the fingers are connected to each other using joints. This provides maximum grasping ability and gives the ability to perform even the smallest operations.
The bones of the palm are also connected to each other by joints with a lesser degree of mobility. They are less likely to undergo deformation and destruction due to their physiology. Another joint that is often destroyed is the wrist. It bears a lot of load as it connects the forearm to the hand. It is complex in structure and is responsible for performing movements simultaneously in several planes. This contributes to the rapid destruction of cartilaginous synovial tissue.
Why is polyosteoarthritis dangerous?
Multiple joint lesions indicate serious disorders in the body. As a rule, the disease develops against the background of other pathological conditions, and does not become a consequence of an accidental injury, therefore the prognosis is always less favorable than with localized osteoarthritis of the elbow, knee or hip joint.
Among the most common complications is limited mobility of the limbs and spinal column. If the disease is not treated at all, the joints wear out to such an extent that every movement brings incredible pain. And since the lesions are multiple, disability is one step away.
The reasons for the development of polyosteoarthrosis are:
- hereditary changes in cartilage tissue, which loses elasticity, strength and ceases to withstand dynamic loads;
- weakness of the ligamentous-muscular system;
- diabetes;
- metabolic disorder;
- diseases of the thyroid, parathyroid and other endocrine glands.
Provoking factors are old age (polyosteoarthrosis develops, usually after 50 years), excessive stress on the joints, especially with a sedentary lifestyle. Bad habits and excess body weight also place a person at risk. Injuries can also accelerate the deformation of cartilage, but in this case they are not the main, but rather a provoking factor.
Polyosteoarthrosis of the fingers is passed on from generation to generation in some families.
Symptoms
- Initially, thickenings appear on the dorsal and lateral surfaces of the finger joints. The first fingers to be affected are the middle and index fingers. They are bent. This occurs due to bone growth in the joint area. Both hands are affected symmetrically at once.
- Then clicking occurs in the joints.
- Slight difficulty moving.
- Pain appears along the edge of the hand when moving the thumb, and attacks of aching pain occur (usually at night).
- The skin over the affected joints becomes red.
With further progression of the disease, coordination of movements is impaired, especially when squeezing the hand. At first it is difficult to thread a needle, and later the process of writing on paper is disrupted. With light loads on the hand, the pain increases.
Typical signs of multiple osteoarthritis
Regardless of the location of the affected joint, the disease makes itself felt with the following symptoms:
- stiffness in movements;
- difficulty moving after sleep (passes within half an hour);
- pain in the affected joints - first after physical activity, and then at rest;
- changing the shape of the joints.
In rare cases, the patient does not even think about treating osteoarthritis, since the symptoms are very smooth or completely absent. However, over time, the disease, alas, progresses.
Is any joint disease arthrosis? Is it possible to cure osteoarthritis quickly? Are chondroprotectors effective in the treatment of polyosteoarthrosis? Am I cured of arthrosis if the pain goes away? A famous rheumatologist answers these and other questions:
How to distinguish arthrosis from rheumatoid arthritis
Since polyosteoarthrosis of the joints of the hands can be confused with rheumatoid arthritis, let's look at the symptoms of both diseases. The information below is provided for informational purposes only. Only a doctor can make a diagnosis based on anamnestic data, the clinical picture of the disease, and the results of laboratory tests.
Table 1. Main differences between arthrosis and rheumatoid arthritis:
| Signs | Deforming osteoarthritis | Rheumatoid arthritis |
| Pain | They intensify during physical activity, but disappear at night. Arthrosis is also characterized by “starting” pain that occurs at the beginning of movement. | Painful sensations appear at night or early in the morning and disappear after a few hours. Unlike arthrosis, with arthritis pain after exercise decreases |
| Stiffness | The patient notes minor difficulties in flexion/extension of the fingers. In the morning, stiffness lasts no more than 15-20 minutes | Pronounced stiffness in the fingers, like “tight gloves.” Usually appears in the morning and persists for several hours |
| Presence of nodules | Bouchard's and Heberden's nodes, which are bone growths on the interphalangeal joints. They are always motionless | Rheumatoid nodules are located subcutaneously in the joint area. They are mobile. Nodules can also appear on the back of the hands, ears, knees, elbows |
| Crunch | Occurs with active finger movements | The appearance of a crunching sound is not typical for arthritis |
| Temperature increase | No | Body temperature can rise to 37-37.5 degrees |
| Changes in analyzes | Sometimes doctors detect nonspecific signs of inflammation in a general blood test | Characterized by increased levels of RF, C-reactive protein, antibodies to MCV and ACCP. In patients with rheumatoid arthritis, the HLAB27 antigen is also detected |
| X-ray signs | In the initial stages, changes in the joints are almost invisible. Later on the pictures you can see a narrowing of the joint spaces and signs of bone damage. Many patients are diagnosed with osteoporosis, which is manifested by a decrease in bone density | Characteristic lesions of the joints, the severity of which depends on the severity of the disease. X-rays show periarticular osteoporosis |
Polyosteoarthrosis of the joints of the foot and hand is treated with the same means as arthrosis of any other localization. To combat the disease, chondroprotectors, anti-inflammatory drugs of the steroid and non-steroidal groups, physical therapy, and physiotherapy are used.
Types of polyosteoarthrosis
Depending on the visual condition of the joints, the disease can take the following forms:
- knotless;
- nodular (with thickenings on small joints - Bouchard's or Heberden's nodes).
Depending on the nature of the course, the disease is classified as follows:
- low-symptomatic form - typical for young patients, rarely accompanied by severe pain, instead of which there are cramps in the calves and nodules on the upper phalanges of the fingers;
- manifest form.
In its manifest form, the disease progresses slowly or quickly. In the first case, a person may not pay attention to the symptoms for more than five years, after which moderate pain appears - due to the weather, when moving, “starting pain”. Rapidly progressive multiple osteoarthritis is typical for young people. Rapid damage to several joint groups occurs with limitation of movement, muscle atrophy and neurological complications.
In old age, multiple osteoarthritis does not progress as quickly as in young people.
Stages of disease development
Polyosteoarthrosis of the joints of the hands has 3 stages:
- First stage. At the initial stage, a person does not notice the signs of the disease, since they rarely appear. Thus, a person sometimes feels slight pain, occasionally a crunching sound is heard when moving, and during prolonged physical activity the affected area of the hand swells.
- Second stage. At this stage, polyosteoarthrosis appears much more often, and the symptoms become more pronounced. Pain is felt much more often, even if a person does not engage in physical activity. In addition, a crunching sound is heard with almost every movement, and the joint very often swells and swells. Also at this stage, the mobility of the limb is slightly limited, and the person cannot be physically active for a long time.
- Third stage. The third stage of polyosteoarthrosis greatly complicates a person’s life. Since the signs of the disease appear constantly, the pain becomes unbearable. Hand mobility is severely limited. In addition, seals appear on the hand, or the affected area becomes severely deformed.
The stages of the disease differ not only in symptoms, but also in treatment methods. Therapy is more effective at stages 1 and 2, but people rarely seek medical help on time.
Manifestations of polyosteoarthrosis
Classic treatment of arthrosis is not always suitable for this diagnosis, since the disease has specific manifestations:
- with generalized arthrosis, three or more joints are affected, most often symmetrical (knee, hip, interphalangeal), Heberden's nodes are noticeable;
- with lesions of the intervertebral joints, pain occurs in different parts of the spine, but secondary symptoms are also possible - dizziness, blurred vision, migraine, indicating compression of the branches of the vertebral artery;
- if polyosteoarthrosis is accompanied by spondylosis of the lumbar and cervical regions with the growth of osteophytes and degenerative changes in cartilage tissue, there is numbness of the limbs, “intermittent” claudication, tinnitus and other unpleasant symptoms;
- sometimes multiple osteoarthritis develops along with periarthritis or tenosynovitis - tissue inflammation, swelling of tendons and capsules.
All this rich symptomatology complicates not only the diagnosis of the disease, but also its treatment.
Polyosteoarthrosis can be accompanied by the most unexpected symptoms
Key Treatment Approaches
It is impossible to diagnose the disease by clinical examination alone. Laboratory tests and x-rays of the affected joints are needed. The therapy is aimed at reducing the intensity of degenerative processes in cartilage tissue, restoring the functioning of affected joints, and relieving pain and inflammation.
Drug treatment includes:
- chondroprotectors – for the restoration of cartilage tissue;
- anti-inflammatory drugs - non-steroidal and intracapsular corticosteroids;
- drugs to improve blood circulation.
If the focus of the disease is identified, it is possible to restore the synovial fluid with intra-articular injections of Noltrex, a synthetic drug with a prolonged action. The product is a liquid endoprosthesis that is well tolerated by the body and does not cause rejection, allergic reactions or infections. After two to three injections at weekly intervals, the damaged joint acquires normal biomechanics, which lasts for a year or longer.
Intra-articular injections quickly restore the biomechanics of an individual joint
Treatment of polyosteoarthrosis of the joints of the hands
Effective conservative treatment of polyosteoarthrosis of the hand joints is possible only at the first and second stages of the disease. If the cartilage tissue is preserved, then it is possible to restore it. At the third stage, treatment of polyosteoarthrosis of the hands is only symptomatic. Its goal is to alleviate the suffering of the patient while awaiting arthroplasty surgery.
In our manual therapy clinic, treatment of polyosteoarthrosis of the joints of the hands is carried out using the following techniques:
- osteopathy – restores microcirculation of blood and lymphatic fluid in the area of tissue damage, improves their trophism, restores physiological structure;
- massage – improves the elasticity of muscles and other soft tissues, relieves their spasm, which creates conditions for normal blood circulation;
- reflexology – starts the process of regeneration of damaged tissues by using the hidden reserves of the human body;
- therapeutic exercises improve the process of diffuse nutrition and restore cartilage tissue;
- physiotherapy improves metabolism at the cellular level.
Electromyostimulation can also be used to restore muscle fiber function, laser treatment of joints, and much more.
If you need effective and safe treatment for polyosteoarthrosis of small joints of the hands, then you can contact an orthopedist for free at our manual therapy clinic in Moscow. The doctor will tell you about all the possibilities and prospects for using manual therapy techniques in your individual case.
The following are used as agents that alleviate the course of polyosteoarthrosis:
- physiotherapeutic procedures - to relieve swelling, stimulate blood circulation and metabolism, accelerate regeneration;
- manual therapy - to reduce pain;
- acupuncture – to restore mobility;
- other rehabilitation measures (physical therapy, massage, orthopedic treatment, etc.).
Part of the treatment is a proper diet and giving up bad habits.
With a timely approach, even such a complex disease as polyosteoarthritis can be kept under control. The disease begins with pain in the spine and hands, and is manifested by deformation of one of the large joints - the knee or hip. Therefore, you should not ignore any pain symptoms or attribute them day after day to physical fatigue. It is impossible to completely cure arthrosis, and when it comes to multiple lesions, the future is at stake. Be vigilant and attentive, first of all, to yourself - then the disease will not have a chance!
Therapy
To confirm the diagnosis, the doctor prescribes certain tests and studies. Any specialist knows that the disease is classified according to ICD-10 and has code M15. The main diagnostic procedure is an x-ray of the affected area. The severity of the manifestations in the image can confirm one of three degrees of severity of the pathology.
Competent treatment involves the cessation or maximum inhibition of destructive changes in the affected joints. In addition, therapy should eliminate or minimize the causes of the pathology. It also involves restoring the functioning of joints and reducing the severity of pain.
Treatment includes several main points.
Drug therapy. Includes the use of chondroprotectors, drugs to stimulate blood circulation, as well as anti-inflammatory drugs. Chondroprotectors are a basic component; without them, treatment is ineffective. Drugs that reduce the severity of inflammation can be non-steroidal and hormonal. Blood circulation stimulants include Tretal and Chimes. Anti-inflammatory drugs are often used topically, in the form of gels and ointments.
Physiotherapeutic treatment. Physiotherapy procedures are necessary to relieve inflammation and swelling; they also stimulate metabolic processes and blood supply to the affected area, which helps restore the structure of cartilage tissue. These include phonophoresis, magnetic therapy, electrophoresis, electromyostimulation, and laser therapy.
Non-traditional methods - manual techniques, acupuncture.
Rehabilitation, both medical and social. Medical rehabilitation can be both surgical and conservative in nature.
Physiotherapy. Includes physical exercises recommended by a physical therapy doctor. Gymnastics should be given at least thirty minutes a day.
Massage.
Treatment with folk remedies. It involves the use of recipes based on natural ingredients. These include onions, garlic, aloe, beeswax, and sedge. Decoctions of herbs - dandelion, burdock, nettle, chamomile, sunflower - also help well. Therapy with folk remedies should be agreed with a doctor.
In rare cases, prosthetics are indicated.