In medical practice, the term “polyosteoarthrosis” is rarely used; often in official medical terminology the more familiar formulation is used – “polyarthrosis”.
Regardless of which term is used, the essence of the pathological condition does not change. The diagnosis refers to a chronic form of degenerative-dystrophic damage to the articular system, where several areas of the human musculoskeletal system act as foci.
Lack of timely diagnosis, as well as refusal of treatment or neglect of the components of complex treatment can cause intensive progression of the pathological condition and a significant deterioration in the patient’s health, including disability.
What is polyosteoarthrosis?
Polyosteoarthrosis (polyarthrosis)
is a chronic disease of the joints of the musculoskeletal system of the human body, leading to deformation of bone tissue or disruption, gradual loss of joint mobility.
The pathological condition under consideration is a representative of the varieties of pathologies of the “osteochondrosis” group, but at the same time it has a striking distinctive feature - the number of focal lesions (more than three). However, despite this, the causes, symptoms and treatment of diseases of the general group are almost the same.
During the development of the disease, destruction of articular and adjacent bone tissues is observed. Activation of the compensatory function of the body causes the accumulation of calcium salts in elastic tissues, which significantly reduces their elasticity and mobility, thus forming new bone formations.
What is the true danger for a patient with such a diagnosis?
Diagnosed polyarthrosis signals serious disorders occurring in the human body. In most cases, the disease develops in the presence of other pathological conditions, which indicates a not very favorable prognosis, unlike other types of osteochondrosis (elbow, knee or hip joint).
The true danger of lack of control over degenerative-dystrophic processes lies in the limited mobility of the limbs and spine. If left untreated, the joint tissues wear out greatly, which causes intense pain to the person.
A large number of lesions of articular and bone lesions can lead to irreversible consequences and cause a significant deterioration in a person’s quality of life, namely, obtaining the status of “disabled” and the inability to self-care.
Disease prevention
Thus, from all of the above it follows that you should always listen to the body and not ignore the alarm signals of your joints. If you experience discomfort, you should consult a doctor to identify and subsequently treat the disease.
Self-medication in this case is a crime against one’s health, because erroneous measures will lead to the patient remaining disabled.
You must always remember that the basis for joint health is, first of all, a healthy lifestyle, proper nutrition and feasible physical activity.
© 2021, Golub Oleg Vasilievich. All rights reserved.
Causes of polyosteoarthrosis
Like other diseases, the pathological process in question has certain causes of development, which are in many ways similar to the pathology of the group of osteochondrosis.
The causes of polyosteoarthrosis include factors such as:
- genetic predisposition, hereditary factor;
- abnormalities in the formation of connective (cartilage) tissue, causing a deterioration in its structural properties;
- insufficient strength of the muscular frame;
- the presence of a disease such as diabetes;
- violation of metabolic processes;
- diseases of the endocrine system, as well as other endocrine glands.
In addition, there is a set of provoking factors, on the basis of which a risk group of people who may encounter this type of pathology is formed.
Risk group
Representatives of the risk group (category of people most likely to develop multifocal joint pathology) are:
- those in adulthood (mostly over 50 years old);
- experiencing increased stress on the joints;
- leading an insufficiently active lifestyle;
- survivors of various types of joint injuries.
There are types of the pathology in question that are inherited, for example, polyosteoarthrosis of the fingers.
Types of polyosteoarthrosis
Today, there are several types of polyosteoarthrosis of the joints. Let's try to understand their features and define the classical classification of the disease in international medicine.
Based on external signs characterizing the condition of the joints of the musculoskeletal system, there are two main forms of polyosteoarthrosis:
- knotless;
- nodular (visually noticeable thickening, the so-called “Bouchard or Heberden nodes”).
Based on the characteristics of the course of the pathological condition and the degree of its intensity, osteoarthritis is classified somewhat differently:
- low-symptomatic – characteristic mainly of young people, it is practically asymptomatic. Instead of the characteristic soreness, a cramp in the calf muscles may be observed, as well as a change in the appearance of the fingers;
- manifest – a slowly progressive form, the intensity of symptoms in which is determined by the patient’s level of health. Moderate pain may be experienced (as the weather changes, when performing various movements, etc.)
Symptoms of polyosteoarthrosis
Symptoms of polyosteoarthrosis have certain specifics. According to existing information, treatment of arthrosis is not always a suitable solution, because the pathology has very unusual manifestations.
Symptoms of polyosteoarthrosis include:
- nodularity of several predominantly symmetrical joints at once (with a generalized type of arthrosis);
- quite severe pain, causing dizziness, ophthalmological disorders, migraine and other signs of compression of large vertebral vessels (if intervertebral tissue is damaged);
- proliferation of bone tissue and harmful, pathologically dangerous changes in connective tissue, accompanied by numbness of the limbs and other signs (with spondylosis of the lumbar and cervical region);
- inflammatory process, local swelling (with periarthritis or tendovaginitis).
The expanded range of symptoms of polyosteoarthrosis somewhat complicates the diagnostic process, which certainly affects the treatment process.
Primary, generalized, nodular and other forms of polyosteoarthrosis
Primary polyosteoarthrosis is extremely rare; more often this disease becomes a consequence of other pathological and degenerative processes in the human body. So, if the disease develops against the background of diabetic angiopathy or atherosclerosis, then they speak of secondary vascular polyosteoarthrosis. For the primary form of the disease, the absence of binding factors and typical negative changes in the human body is necessary.
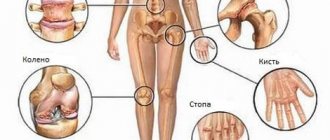
Generalized polyosteoarthrosis is a form of the disease in which total damage to all joints of the upper or lower extremities occurs. Thus, the hip, knee, ankle, metatarsal and interphalangeal joints on the left and right lower extremities are simultaneously destroyed in a generalized manner. A similar situation can be observed with the joints of the upper limbs and spinal column.
The nodular form of polyosteoarthrosis develops more often in women. Polyosteoarthritis nodosa affects the small interphalangeal joints of the fingers and toes. Bouchard's nodes appear, which are located on the lateral surfaces of the joint. They are dense, motionless, painful on palpation.
There are other forms of polyosteoarthrosis. The symptoms of this disease largely depend on the location of the destructive process and the stage at which they are located. Among the most characteristic clinical signs of the disease are:
- pain in the projection of the affected joints;
- limited mobility;
- reduction in the length of arms and legs;
- hyperemia of the skin over diseased joints;
- the appearance of extraneous sounds when moving (creaking, clicking, crunching, etc.);
- decrease in muscle strength and the appearance of increased fatigue during habitual physical activity;
- disruption of innervation when the main nerves are damaged due to the growth of deformed bone tissue.
For diagnosis, an x-ray, CT or MRI examination, a biochemical blood test using rheumatic tests, and arthroscopy are prescribed.
Diagnostic techniques
Diagnosis in the presence of appropriate symptoms is carried out in a clinic. To receive professional diagnostic and treatment assistance, it is enough to have an appointment with a therapist, who, based on the results of the initial examination, will draw certain conclusions and refer the patient to a more specialized specialist.
There are 4 most effective diagnostic methods:
- X-ray examination is the optimally accessible diagnostic method that allows you to assess the degree of change in the joint space and bone surfaces, etc. transformations, allowing you to draw a conclusion about the stage of the pathology.
- Magnetic resonance imaging (MRI) is the best solution that allows you to visualize the condition of soft tissues (muscle frame, ligaments and tendons, as well as the surface of the joint capsule).
- Laboratory blood testing - makes it possible to assess the general health of a person and test for the presence of rheumatoid markers.
- Arthroscopic examination - a therapeutic and diagnostic operation allows you to penetrate into the articular cavity in a minimally invasive way and examine in detail the surfaces of the articular tissues. If necessary, it is possible to take a tissue fragment and a small amount of synovial fluid for analysis.
Treatment of polyosteoarthrosis
The key to successful treatment of polyosteoarthrosis is compliance with the instructions of the attending physician, maintaining a healthy lifestyle and, of course, following the basics of dietary nutrition.
Even the most complex disease can be treated if medical help is sought at the right time. Polyosteoarthrosis can be successfully cured using both a complex of conservative techniques and surgical operations.
The choice of the most promising direction of treatment is determined on an individual basis, taking into account the characteristics of the course of the disease and the number of affected joints.
Let us consider the components of the treatment of polyosteoarthrosis in more detail.
Drug therapy
The basis of conservative treatment is drug therapy. The complex of drugs, as well as the dosage and duration of their use, are determined by the treating specialist on an individual basis, taking into account the intended treatment plan.
As part of drug therapy, the following groups of drugs are used:
- painkillers;
- corticosteroids;
- chondroprotectors.
It is important to pay special attention to chondroprotectors, which protect the remaining cartilage tissue from the further destructive effects of pathological processes and create optimal conditions for its restoration. Among the drugs of this kind is Artracam, which is distinguished by its effectiveness and optimally affordable cost.
Physiotherapeutic treatment
Physiotherapeutic treatment of polyosteoarthrosis belongs to the category of auxiliary therapeutic techniques, the beneficial effects of which help stimulate the renewal of bone and cartilage tissue of the human body.
In order to prevent the development of pathologically dangerous processes and restore damaged structures, methods such as:
- electrophoresis;
- exposure to magnets/laser;
- warming up (provided there is no inflammation).
As part of the implementation of a complex of physiotherapeutic procedures, patients are recommended to visit specialized sanatoriums and medical resorts that specialize in the treatment and rehabilitation of people with pathologies of the musculoskeletal system.
Therapeutic physical education (PT)
Of particular importance in the treatment, rehabilitation and prevention of pathologies of the musculoskeletal system is physical activity, in particular, exercise therapy.
A set of exercises is selected taking into account the location of pathological processes, as well as the characteristics of clinical manifestations.
It is important that the exercises must be performed under the strict guidance of a specialist, because deviation from the norm can cause overexertion and harm to health.
Surgery
In some particularly advanced cases, when conservative therapy does not produce the desired results, the patient may be indicated for surgical intervention.
The most popular and optimally effective solution is endoprosthetics - an operation that involves removing the affected joint and its full/partial replacement with an individually formed prosthesis.
After surgery, there is a long and rather difficult recovery period. If all recommendations are followed, the patient can return to a full standard of living.
Key Treatment Approaches
It is impossible to diagnose the disease by clinical examination alone. Laboratory tests and x-rays of the affected joints are needed. The therapy is aimed at reducing the intensity of degenerative processes in cartilage tissue, restoring the functioning of affected joints, and relieving pain and inflammation.
Drug treatment includes:
- chondroprotectors – for the restoration of cartilage tissue;
- anti-inflammatory drugs - non-steroidal and intracapsular corticosteroids;
- drugs to improve blood circulation.
If the focus of the disease is identified, it is possible to restore the synovial fluid with intra-articular injections of Noltrex, a synthetic drug with a prolonged action. The product is a liquid endoprosthesis that is well tolerated by the body and does not cause rejection, allergic reactions or infections. After two to three injections at weekly intervals, the damaged joint acquires normal biomechanics, which lasts for a year or longer.
Intra-articular injections quickly restore the biomechanics of an individual joint
Forecasts
Seeking qualified medical help at an early stage is the key to success and the most favorable scenario for the complete elimination of the symptoms of polyosteoarthrosis, and, sometimes, the complete recovery of the patient. If the intended treatment plan is followed, most diagnosed cases can be successfully treated.
Conservative therapy gives positive results within the first week of treatment, depending on the individual characteristics of the patient. After just 1-1.5 months, the mobility of the affected joints improves significantly.
Polyosteoarthrosis is one of the incurable diseases, which means that it is necessary to follow medical recommendations for life.
Typical signs of multiple osteoarthritis
Regardless of the location of the affected joint, the disease makes itself felt with the following symptoms:
- stiffness in movements;
- difficulty moving after sleep (passes within half an hour);
- pain in the affected joints - first after physical activity, and then at rest;
- changing the shape of the joints.
In rare cases, the patient does not even think about treating osteoarthritis, since the symptoms are very smooth or completely absent. However, over time, the disease, alas, progresses.
Is any joint disease arthrosis? Is it possible to cure osteoarthritis quickly? Are chondroprotectors effective in the treatment of polyosteoarthrosis? Am I cured of arthrosis if the pain goes away? A famous rheumatologist answers these and other questions: