The temporomandibular joint (TMJ) is a joint located in front of the ear and connects the lower jaw to the base of the skull. Its main function is to provide movement of the lower jaw.
The TMJ is one of the most important joints in our body; without it, we would not be able to talk or eat. This is why it is important to identify TMJ diseases at an early stage.
TMJ diseases are common - according to various sources, they affect from 70% to 92% of the population, people of different genders and ages. The most common TMJ disease is TMJ muscle-articular dysfunction.
The main signs of musculo-articular dysfunction of the TMJ:
- Pain syndrome . Depending on the stage of the disease, you may feel pain in the area of the masticatory muscles when eating, speaking for a long time, and in difficult cases even constant muscle pain.
- Crunching, clicking in the TMJ area. It is important to understand that normal movement in the joint should be silent, and any clicks and crunches in the joint area indicate that the cartilage tissue of the joint is injured.
- Asymmetrical, uneven opening of the mouth. Normally, when opening the mouth, the lower jaw should move evenly downward, without lateral displacement. If the lower jaw shifts to the side when opening the mouth or its S-shaped movement, you should consult a doctor.
- Limitation of mouth opening . Normally, the mouth should open 40-45 mm, this distance is approximately equal to the width of three fingers. With TMJ dysfunction, mouth opening is limited to 20 mm or less at maximum mouth opening.
- Other symptoms. Also, with TMJ dysfunction, there may be jamming of the jaw, grinding of teeth (bruxism), dizziness, and headache.
At the onset of the disease, symptoms of dysfunction may be mild, but without treatment the disease will progress.
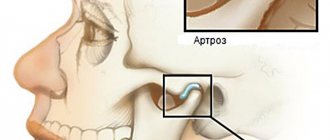
Dangerous! With long-term dysfunction, osteoarthritis of the TMJ can develop.
NeoStom – Dentistry website
In various periods of the development of dentistry, scientists in their works proposed the use of certain classifications of diseases of the temporomandibular joint. The term " arthritis"was introduced by Hippocrates. At the International Congress in London in 1913, inflammatory arthritis and degenerative arthrosis were clearly differentiated and separated from each other.For a long time, the simplest and most convenient classification was proposed by V.I. Burgonskaya and Yu.I. Vernadsky (1970). In their opinion, all diseases of the temporomandibular joint must be divided into arthritis, arthrosis and arthritic arthrosis. V.A. Khvatova in 1982 proposed using the following nosological forms of diseases of the temporomandibular joint: arthritis (acute and chronic), arthrosis (sclerosing and deforming, in the chronic stage and in the acute stage), muscle-articular dysfunctions, ankylosis, tumors. Dental and neurological symptoms, dislocations and subluxations of the lower jaw, articular disc, observed in various nosological forms, were considered as a complication of these diseases. Dysfunction is understood as a pathology of the temporomandibular joint, not diagnosed on x-rays, accompanied by impaired movements of the lower jaw, sound phenomena when opening and closing the mouth, discomfort and periodic pain in the area of the temporomandibular joint, occurring without radiological changes. In foreign, and recently in domestic literature, the term “internal derangement” has firmly taken its place, which accounts for 70 to 82% of all diseases of the temporomandibular joint. This term refers to changes developing in the joint, including displacements, defects, deformations of the articular disc, sprains and ruptures of articular ligaments, detected using modern radiation diagnostic methods. In close connection with internal disorders, secondary osteoarthritis is considered, developing without timely treatment of the latter. In essence, internal disorders are the morphological substrate of dysfunctions of the temporomandibular joint.
Numerous studies [Kostur B.K. and others (1981), Egorov P.M., Karapetyan I.S. (1982), Petrosov Yu.A. (1985), Sysolyatin P.G. and others, Minyaeva V.A. (1989), Sergeeva T.A. (1997), Vyazmin A.Ya. (1999) and others] found that in 70-89% of cases, pain in the temporomandibular joint is not associated with inflammatory processes. More often it is a common functional disorder - dysfunction and is caused by changes in soft tissue elements: the disc, the retrodiscal zone, the capsular-ligamentous apparatus, the lateral pterygoid muscles, etc. Classification by Yu.A. Petrosova (1982) most fully reflects the clinical picture of diseases of the temporomandibular joint, where, among various forms of lesions, dysfunctional syndromes are put in first place, and the clinical manifestations of which are outlined quite clearly. Yu.A. Petrosov classifies: I. Dysfunctional conditions of the temporomandibular joint: - neuromuscular dysfunctional syndrome; — occlusal-articulatory dysfunctional syndrome; - habitual dislocations in the joint (jaw, meniscus). II. Arthritis: - acute infectious (specific, nonspecific); - acute traumatic; - chronic rheumatic, rheumatoid and infectious-allergic. III. Arthrosis: - post-infectious (neoarthrosis); — post-traumatic (deforming) osteoarthritis; — myogenic osteoarthritis; - metabolic arthrosis; - ankylosis (fibrous, bone). IV. Combined forms. V. Neoplasms (benign and malignant) and dysplastic (tumor) processes. Neuromuscular dysfunctional syndrome occurs against the background of disorders of the neuromuscular complex and is usually caused by various causes or initiating factors, namely: psychogenic factor (stress, hysterical crises, grimaces), factors of mechanical overload of muscles associated with prolonged unilateral type of chewing, profession, parafunctions of masticatory muscles and etc.
Occlusal-articulation syndrome occurs with a decreasing bite, as a result of the lack of distal support of the bite, increased tooth wear, bite pathology, improper prosthetics, deformation of the occlusal surface of the dentition, etc. Disorders of the function of the neuromuscular complex very rarely develop in isolation and are more often combined with disturbances of occlusion. According to I. Sestak (1984), disorders of the hard tissues of teeth, occlusion and articulation constitute a triad of signs of dysfunction, which is observed in 96% of patients with this pathology. Since the first symptoms of the disease, such as acoustic symptoms, intermittent and moderate pain in the joint, a feeling of awkwardness and fatigue of the masticatory muscles, do not particularly bother patients, as a result, at this stage they are not provided with timely and targeted dental care, which they seek already at advanced, combined forms of damage. In the clinical picture, symptoms develop that are directly related to the temporomandibular joint, but go beyond the dental system: decreased ability to work, increased fatigue, headaches, dizziness, etc. In general, there is no single generally accepted classification of the pathology of the temporomandibular joint. The proposed ICD-10 nomenclature is rarely used both in domestic and foreign practice, it distinguishes: • Syndrome of painful dysfunction of the temporomandibular joint (Costen syndrome). • Recurrent dislocation and subluxation of the temporomandibular joint. • Pain in the temporomandibular joint, not elsewhere classified. • Osteophyte of the temporomandibular joint. • Other specified diseases of the temporomandibular joint.
• Diseases of the temporomandibular joint, unspecified.
You might be interested in:
- Biomechanics of the lower jaw
- Features of writing a medical history for TMJ diseases
- Principles of treatment of TMJ diseases
- Special methods for examining TMJ diseases
- Methods of examination and diagnosis of TMJ diseases
Related materials:
- Features of the structure of the TMJ. Etiology and pathogenesis of TMJ changes
- TMJ diseases
Treatment of TMJ diseases:
Treatment is prescribed depending on the examination results. When treating a joint, the following is used:
- drug therapy
- physiotherapy
- myogymnastics (muscle gymnastics)
- splint therapy
Splin therapy is one of the most effective methods of treating musculo-articular dysfunction of the TMJ. An individual mouthguard is made for the patient, which helps to relax the masticatory muscles, set the joint in the correct position, thereby eliminating the cause of musculo-articular dysfunction of the TMJ.
The article was prepared by Kurakova A.S., orthodontist.
Temporomandibular joint diseases
Go to:
- Maxillofacial Surgery
Facial pain is one of the most common complaints of patients turning to us for help. At the same time, we observe true facial pain in a third of patients, while secondary facial pain caused by pathology of the ENT organs, ophthalmological problems and dental disorders make up the vast majority of cases. One of the main nosological forms is temporomandibular joint dysfunction syndrome (TMJ) - one of the most difficult and controversial diagnoses in modern medicine. Up to 40% of people experience symptoms of temporomandibular joint disease, but not everyone seeks medical help.
What is temporomandibular joint dysfunction (TMJ)?
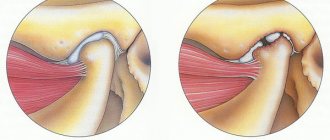
The head of the lower jaw, the articular surface of the temporal bone, the articular disc located between them, the articular capsule, as well as the ligamentous apparatus and masticatory muscles take part in the formation of our joint. The joints are located anterior to the ear canal and work synergistically.
Temporomandibular joint dysfunction means that one of the components of our joint is not functioning properly. This joint is one of the most complex in the human body, it is responsible for the movement of the lower jaw forward, backward and from side to side. Any pathological condition that does not allow this complex system of muscles, ligaments, discs and bones to work properly leads to its dysfunction.
-10% on all MRI and CT scans in the department on Narodnaya
How does the TMJ function?
The temporomandibular joint is a combination joint, representing the functional combination of two anatomically separate joints (left and right). The articulating surfaces of the head of the mandible and the articular surface of the temporal bone are supplemented by a fibrous intra-articular disc located between them, which is attached with its edges to the articular capsule and divides the articular cavity into two sections. Both temporomandibular joints function simultaneously, representing a single combined joint; thanks to the intra-articular disc, movements in three directions are possible in it.
- vertical axis: lowering and raising the lower jaw (opening and closing the mouth) - occurs in the lower part of the joint, between the cartilaginous disc and the head of the lower jaw;
- sagittal axis: displacement of the lower jaw forward and backward - occurs in the upper part of the joint, between the cartilaginous disc and the articular surface of the temporal bone;
- frontal axis: lateral movements (rotation of the lower jaw) during chewing - on one side, the head of the lower jaw together with the cartilaginous disc emerges from the articular fossa onto the tubercle, and on the opposite side, the head of the lower jaw rotates relative to the articular cavity around a vertical axis.
What are the symptoms of temporomandibular joint disorders?
Painful TMJ dysfunction or TMJ pain dysfunction syndrome has many synonyms: Costen's syndrome, myofascial pain syndrome of TMJ dysfunction, TMJ dysfunction, craniomandibular dysfunction syndrome, mandibular dysfunction, musculo-articular dysfunction of the TMJ, etc.
This symptom complex was first described by otolaryngologist J. Costen, who observed it in patients with missing teeth and in people with low occlusion. Painful joint dysfunction is characterized by the following manifestations:
- headache (fronto-temporo-parietal localization), ear pain, as well as pain and pressing sensations behind the eyes;
- “crunching” or “clicking” when opening or closing the mouth;
- pain when yawning and wide open mouth;
- spasm of the chewing muscles;
- displacement of the center line of the jaw;
- malocclusion.
The variety of clinical manifestations of temporomandibular joint dysfunction is determined by the polyetiology (multiple causes) of the pathological processes developing in it, which complicates diagnosis and treatment.
What Causes TMJ Disorders?
In general, TMJ disorders are a multifactorial process. These factors can be divided into two types: problems associated with the masticatory muscles and problems with the joint itself. Muscle problems are the most common type, especially for young people.
Muscle problems can be caused by:
- Muscle hyperactivity. This can happen if you clench your jaw frequently, especially while sleeping, which is quite common.
- Scar changes in the masticatory muscles
- Increased sensitivity to pain. This may be due to stress, or some other process that affects pain sensitivity
- Joint problems can be caused by
- Degenerative-dystrophic changes in the joint
- Inflammation in the joint (arthritis)
- TMJ injury
How are TMJ disorders diagnosed?
The diagnosis is made based on symptoms and additional examination methods.
Possible examinations:
- Blood tests that may be useful to look for signs of inflammation;
- MRI - this method is used to give a detailed morphological picture of the joint;
- Arthroscopy (using a fiber optic device) to look "inside" the joint);
- Electromyography (EMG) is an objective method for studying the neuromuscular system by recording the electrical potentials of the masticatory muscles, which allows one to assess the functional state of the dental system;
- Densitometry is a method for measuring bone mineral density, that is, the content of calcium, which is its main structural element. The information obtained is subjected to computer processing, the thickness and size of the bones, and their volumetric density are calculated. Such indicators make it possible to judge the resistance of bone tissue to mechanical stress.
What is the treatment for temporomandibular disorders?
Most problems in the mandibular joint can be eliminated using simple procedures, such as painkillers and muscle relaxants, a course of physiotherapy and exercise therapy, and advice on how to relieve the joint, procedures aimed at relaxation and anti-stress therapy. These are the so-called orthopedic methods using mouthguards and bite pads.
In case of more severe disorders in the joint or the ineffectiveness of conservative methods, they resort to injections of botulinum toxin into the masticatory muscles if they are hyperactive and intra-articular administration of steroids.
Arthroscopy is a minimally invasive surgical treatment using endoscopic equipment. A very small percentage of patients may be eligible for open joint surgery. As a rule, these are gross deformations of the joint in the form of ankylosis.
It's great to have all the doctors nearby.
Dentists for adults and children.
What are the prospects for the treatment of temporomandibular disorders?
Most TMJ disorders improve over time.
Make an appointment with a specialist by phone, online appointment or mobile application.
tourism news photo
What does a patient need to know about TMJ disorders?
Clinical experience, scientific work, algorithm for the treatment of TMJ diseases at the Department of Maxillofacial Surgery of the Moscow State Medical University
The problem of medical rehabilitation of patients with diseases of the temporomandibular joints (TMJ) has attracted the attention of dentists for several decades.
The clinical manifestations of TMJ diseases are highly variable and range from myogenic facial pain to joint noises and blocking and restriction of mandibular movements.
More and more researchers see the occurrence of disorders of the temporomandibular joints as the result of a combination of a number of unfavorable factors that can reinforce each other. The most significant of them are dentofacial anomalies and deformations of the dentition, dysfunction of the masticatory muscles and processes of internal disorders in the TMJ.
There has been an increase in the number of patients with TMJ diseases.
Currently, this pathology ranks third in the prevalence of diseases of the maxillofacial area after caries and periodontal diseases among.
The main reason for seeking professional medical help is Pain.
What symptoms should alert the patient and become a reason to seek medical help?
As an absolute indication for treatment, the triad of signs must coincide:
1. Presence of pain syndrome (Pain)
2. Limitation of mouth opening
3. Internal disorders of the TMJ, confirmed by the results of Magnetic Resonance Imaging (ICD-10C K07.6)
As signs, if one of them is present, it is necessary to consult a specialist, it is necessary to note:
A) Asymmetrical mouth opening (“mouth opens crookedly”)
B) Noises during movements of the lower jaw
B) Pain on palpation of the masticatory muscles
D) Uncomfortable closure of teeth.
Historically, ideas about the etiology and pathogenesis of Temporomandibular Disorders (TMD) have been transformed from purely dental to general medical ones, which has influenced the approach to the diagnosis and treatment of patients with these diseases.
Since 1934, when Costen described otomandibular syndrome, thought to be associated with malocclusion, occlusion has been thought to be the leading, if not the only, factor causing Temporomandibular Disorders (TMDs).
However, the results of studies conducted using multivariate analysis and logical regression models allow us to conclude that occlusal disorders occur in only 27% of patients suffering from TMD.
In other words, the influence of occlusion on the development of TMD is much less than previously thought, which requires additional research aimed at identifying other potential risk factors for TMD.
Currently, most authors support the concept of multifactorial development of TMD, based on the instability of the masticatory apparatus.
At the Department of Maxillary Surgery of the Moscow State Medical University named after A.I. Evdokimov adhere to the global concept of the development of TMJ diseases, substantiated by a significant number of randomized clinical studies conducted around the world and at their own clinical sites.
It is believed that joint lubrication plays a large role in the prevention of dysfunction. Phospholipids are attached to the articular surfaces, and hyaluronic acid, in turn, is fixed to them, protecting the joint and ensuring uniform movement.
Disruption of this mechanism can lead to pathological changes in the TMJ.
Understanding this issue is a key factor in the treatment of TMJ diseases, naturally as part of a complex algorithm that takes into account the general condition of the dentofacial apparatus and the general somatic status of the patient.
On the basis of the Department of Maxillofacial Surgery under the guidance of Doctor of Medical Sciences. Professor Alexey Yuryevich Drobyshev developed an algorithm for the diagnosis and treatment of diseases of the temporomandibular joint, which has shown high clinical effectiveness and meets international standards for providing care to patients with this group of diseases.
The method has been successfully used for more than 5 years and is included in the educational and methodological work of the department, a large number of scientific papers have been published, several Ph.D. theses have been defended using this algorithm and, of course, hundreds of grateful patients.
SO, I AM A PATIENT, WHAT SHOULD I DO?
First - Consultation at the Center for Dentistry and Maxillofacial Surgery at the Department of Maxillofacial Surgery of the Moscow State Medical University named after A.I. Evdokimova.
Any diagnosis is made on the basis of a clinical examination, without which it is IMPOSSIBLE to make a diagnosis!
At our base, we use a developed scheme for the complex diagnosis of diseases of the TMJ and the dental-jaw system, which can reveal not only the presence of pathology, but also its cause.
Second, during the consultation you will be given directions for all the necessary examination methods. It is recommended to do research as prescribed by the doctor, since the ultimate goal of any diagnosis is to fully inform you and your doctor. Not all centers perform research according to standards and therefore they will recommend the best ones to you. If you already have research (images, tests, etc.), you need to take them with you. The “gold standard” for the study of TMJ diseases is magnetic resonance imaging (MRI). The method has serious advantages: it is a magnet (no radiation exposure, can be done an unlimited number of times and regardless of health status), all structures of the joint are visualized, including soft tissue components such as the intra-articular disc, muscles and even inflammatory fluid in the joint cavity.
Often the cause of joint diseases lies in a combination of several factors, one of which may be the presence of dentofacial anomalies (bad bite). Malocclusions can be caused not only by the dentition itself, but also by the jaw bones. Comprehensive rehabilitation of patients with dentofacial anomalies is a priority direction of the department’s medical work. Particular attention is also paid to the possibility of developing common connective tissue diseases, such as Rheumatoid arthritis, ankylosing spondylitis and others. Specialized clinical and laboratory studies aimed at verification are prescribed.
Based on the results of the consultation, you will be given an advisory opinion and recommendations explained.
WHAT IS THE TREATMENT?
Relieving excess load from the joint and reducing spastic load on the masticatory muscles is an important stage of preparatory therapy.
The task of the preparatory stage of treatment is performed by a specially manufactured occlusal-stabilizing device (KAPPA).
The device is made based on the results of a special myocentric program using the Transcutaneous Electrical Myostimulation method.
The main functions of the OSA (occlusal-stabilizing apparatus, mouthguard):
- Protection of dentition and TMJ from parafunction
- Redistribution of the contact articular surfaces of the TMJ
- Muscle relaxation
- Centering the articular heads
- Reposition of articular elements (DISC REDUCTION)
- Preparation for surgical treatments
Indications for use of OSA:
- lack of occlusally stable position of the lower jaw in the habitual bite;
- dislocation of articular discs;
- muscle dysfunction;
- decrease in bite height.
Contraindications to the use of OSA:
1) lack of CT and MRI diagnostics;
2) unsatisfactory oral hygiene;
3) the presence of a purulent-inflammatory process.
During the stages of wearing the devices, specialized pharmacological therapy is carried out, and, if necessary, a course of physiotherapeutic procedures and gymnastics under the supervision of the attending physician.
The use of standard and silicone mouth guards is strongly discouraged. The use of these devices leads to an “expander effect” due to overload of the masticatory muscles and incorrect occlusal relationships. Such soft-elastic devices are dangerous and no one is responsible for their use. Occlusal devices are manufactured on the basis of comprehensive laboratory diagnostics from specialized certified materials.
In the treatment of TMJ , modern diagnostic methods are used:
Magnetic resonance imaging
Kinesiographic examination
Kinesiography is a graphic recording of the movements made by the lower jaw during chewing and performing functional tests.
Transcutaneous electromyostimulation
Therapeutic and diagnostic splint therapy
The main functions of the OSA (occlusal-stabilizing apparatus, splint):
- Protection of dentition and TMJ from parafunction
- Redistribution of the contact articular surfaces of the TMJ
- Muscle relaxation
- Centering the condyles
- Reposition of articular elements
- Preparation for surgical treatments
Indications for use of OSA:
- lack of occlusally stable position of the lower jaw in the habitual bite;
- dislocation of articular discs;
- muscle dysfunction;
- decrease in bite height.
Contraindications to the use of OSA:
1) lack of CT and MRI diagnostics;
2) unsatisfactory oral hygiene;
3) the presence of a purulent-inflammatory process.
Minimally invasive surgical techniques for the treatment of TMJ diseases are successfully used: Arthrocentesis with lavage and Arthroscopic surgery.
Clinical example of the effectiveness of Arthrocentesis with TMJ lavage:
The use of the drug PRGF (Plasma enriched with growth factors) has shown high efficiency.
here joomla 3 templates