Temporomandibular joint dysfunction is a pathological process that is caused by changes in the jaws, articular surfaces and muscle tissue. In this case, uncoordinated movement of both jaws in relation to each other is diagnosed with clear signs of a violation of static and dynamic occlusion. The pathology occurs quite often, accounting for about 75% of all patients in dental offices. Many oral diseases are a consequence of TMJ dysfunction. Also, nearby organs and tissues are involved in the destructive process, which complicates its clinical signs with additional symptoms.
Specialists usually diagnose a chronic form of pathology in the temporomandibular joint, which in some cases accompanies a person for many years and is compensated by other components of the maxillofacial apparatus. Without therapeutic measures, complete or partial ankylosis may occur; therefore, a timely visit to the dentist will prevent impaired chewing function, visual unattractiveness and many other problems, the development of which can be caused by TMJ dysfunction.
Definition of temporomandibular joint
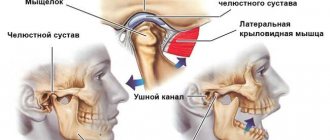
The temporomandibular joint is a fairly mobile joint that connects the lower jaw and the temporal bone, located on either side of the skull, in front of the ears.
This hinge joint provides the following functions:
- sedate jaw movements characteristic of conversation;
- maximum opening of the mouth, for example, when yawning;
- movement of the jaw during chewing.
The main assistants to the joints of the maxillofacial apparatus are the masticatory muscles, which help keep the lower jaw in the correct anatomical position, while easing the load on it.
Risk factors
Main reasons:
- Injury. The cause in this case may be a bruise, a blow, or a sudden opening of the mouth.
- Infection of ENT organs. Arthritis of the maxillary joint can be caused by streptococci, chlamydia or tuberculosis.
- Osteomyelitis.
- Untreated caries.
- Periodontal diseases.
- Otitis.
In addition, the following conditions may also affect the development of jaw arthritis:
- Gout.
- Systemic lupus erythematosus.
- Diabetes.
- Thyroid diseases.
- Rheumatoid and reactive arthritis.
Sometimes inflammation can be caused by general hypothermia of the body.
Causes of dysfunction of the temporomandibular joint
Modern dentistry has facts that have not been fully studied about the causes of pathologies of the temporomandibular joint. However, based on the available data, experts suggest that the main problem lies in the destructive processes of the muscles and altered components of the joint itself.
Orthodontists identify the following pathologies and situations as the main causes and provoking factors for impaired mobility of the joint connecting the lower jaw (mandible) and the temporal bone:
- trauma to the lower jaw, which can provoke a violation of static and dynamic occlusion;
- damage to the facial muscles, which is accompanied by an increase in the load on the joint;
- pinching of the facial nerve causes excessive muscle tension, which, in turn, disrupts the functioning of the joint and mandible as a whole;
- involuntary contraction of the chewing muscles, which is usually accompanied by damage to the dentition, periodontal disease and inflammation of the TMJ;
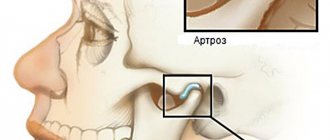
- damage to the temporomandibular joint due to the progression of osteoarthritis or rheumatoid arthritis;
- inadequate prosthetics;
- congenital anomalies of the structure of the lower jaw;
- malocclusion, which in 95% is caused by destructive manifestations;
- pathologically low alveolar processes;
- inflammatory processes of the articular surface of infectious etiology;
- incorrect position of the disc at the junction of the head of the joint and the corresponding notch;
- prolonged tension of the facial muscles, clenching of teeth due to strong emotional stress.
The information provided about the probable causes of TMJ dysfunction is confirmed by clinical studies and the results of collected anamnesis about the disease.
Classification of TMJ arthritis
The nature of the course of arthritis implies the presence of acute and chronic forms. The acute form of this disease is characterized by a serous and purulent course. There is also a classification of TMJ arthritis, depending on the etiological origin:
- traumatic arthritis;
- infectious arthritis (nonspecific and specific);
- rheumatoid arthritis;
- other rare forms (reactive arthritis and others).
Specific infectious inflammations of the TMJ include: syphilitic, tuberculous, actinomycotic, gonorrheal, etc.
Characteristic symptoms
Symptoms characteristic of the manifestation of a destructive process in the joint, which ensures the mobility of the lower jaw, can be pronounced or blurred, which is typical for a protracted chronic process. Periods of remission followed by exacerbations are also likely, that is, symptoms can suddenly appear against the background of imaginary well-being.
Specialists in the treatment of TMJ destruction identify the following characteristic symptoms of this pathology:
- severe soreness of the muscles of the face, neck, shoulder girdle and parotid region with irradiation into the ear cavity;
- toothache;
- pain tends to intensify during speech, eating or yawning, that is, when the amplitude of movement of the lower jaw increases;
- there is pronounced stiffness and limitation in the movement of the jaws;
- partial ankylosis (immobility) may occur as a result of jamming or blocking of the joint;
- there is a pronounced sound when opening the mouth, for example, clattering, clicking or creaking, which, in most cases, is accompanied by sharp pain;
- tension and fatigue of the facial muscles;
- sometimes swelling of the affected joint increases;
- difficulty chewing, accompanied by a feeling that the jaws are not touching each other.
The patient's general condition also shows deterioration, characterized by headache, dizziness, noise and aching pain in the ears, and decreased performance. Acute pathological processes in the temporomandibular joint sharply reduce a person’s quality of life with debilitating manifestations, disrupting many vital functions.
TMJ. Complications and their solutions
The human body is an ordered multi-level biosystem, which includes molecular, cellular, tissue, organ and system levels of organization.
The processes occurring at all levels of human organization are always coordinated with each other. Such coherence and coordination occur due to the processes of regulation of the functions of the human body, and is possible only if each system functions correctly separately.
Chewing apparatus
The chewing function is performed by the chewing organ, which consists of several components. It is a mistake to think that only teeth are needed for proper chewing. The masticatory organ includes the upper and lower jaws, the temporomandibular joint (TMJ), the masticatory muscles and the neck muscles that move the lower jaw, teeth, gums and tongue. In general, all these organs involved in the act of chewing can be united by the concept of the masticatory apparatus.
The health and functionality of the masticatory apparatus largely depends on the balance between the teeth, the temporomandibular joint and the masticatory muscles. When there is a balance between these components, the chewing organ as a whole can be considered healthy. As soon as an imbalance occurs in one of the components, there will be a dysfunction of chewing and an imbalance in the entire body and human body.
Adaptation of the body
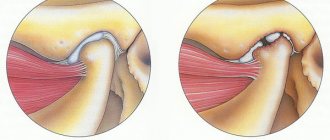
But our body has a unique ability to adapt, due to which we may not notice the problem. Adaptation of the body occurs constantly, for example, to regulate body temperature during severe frosts in the environment. Also, the adaptation process is activated when supercontacts occur on the teeth, or disturbances in the relative position of the skull bones, dysfunction or dislocation of the TMJ. If the relationship of the dentition becomes incorrect due to the loss of teeth or restorations, the lower jaw also changes its position, and after it the position in the joint changes. The head of the joint may rotate or distalize. This compresses the articular disc and can be pushed forward, causing disc dislocation. The masticatory muscles, which are in an overstrained state due to the fact that they are trying to hold the lower jaw in the “correct” position, also contribute to TMJ dislocation.
Chronic joint dislocation
Dislocation can occur with any movements of the lower jaw - opening and closing the mouth, thereby becoming chronic.
Typical symptoms of a TMJ dislocation include clicking, crunching, or discomfort in front of the tragus of the ear.
The head of the joint, on one or both sides, moves deeper into the articular cavity, beginning to put pressure on the bilaminar zone of the joint, rich in blood vessels and nerves, which is no longer protected by the anteriorly dislocated disc. Pain appears.
If left untreated
If the joint is not treated in time, the disc begins to deform, fragment, and wear out. The ligament holding the disc in place may be torn or stretched. Afterwards, the process of destruction of the surface of the joint head begins, which will move without shock absorption and become damaged. The clicking sounds are replaced by an unpleasant crunching sensation when opening the mouth.
But what is also important is that when there is a violation at the level of the TMJ, this leads to a violation of the remaining joints below the head, they adapt to the new position of the TMJ. The result is a deterioration in blood supply, lymphatic drainage, pinched nerve bundles, problems in the functioning of internal organs, and subsequently problems with human health and performance. The body in space is in a forced position, and maintaining overloaded muscles around the joints takes a lot of energy from the body.
An imbalance in the TMJ ligaments can cause various physical problems in the human body: hearing impairment, ringing in the ears, headaches, migraines - when the temporal muscle is pinched; problems with vision or color perception - when the sphenoid bone is pinched; excessive clenching of the jaws and tension of the masticatory muscle (hypertonicity), pain in the jaw when opening or closing.
Symptoms of hypertonicity of the masticatory muscles and/or TMJ disorders
- Increased sensitivity of teeth.
- Pathology of hard dental tissues.
- Cracks and fractures.
- Pathological abrasion of teeth.
- Periodontal pathology.
- Temporomandibular joint dysfunction (TMJ).
- Hypertrophy of the masticatory muscles.
- Chips of ceramic crowns and fillings.
- Compensatory hypertrophy of the periosteum in the area of the angles of the lower jaw.
- Crunches, noises in the TMJ area.
- Noise in ears.
- Headache.
- Wedge-shaped defects.
Where to start dental treatment for TMJ. Shock wave therapy.
It is important to begin dental treatment with relaxation and restoration of muscle tone. Through relaxation of the masticatory muscles, a powerful and at the same time gentle adjustment of the temporomandibular joint occurs. We achieve this effect using shock wave therapy (SWT). UVT is essentially a deep massage at the cellular level. During the passage of a shock sound wave of a given frequency through soft tissues, they are first sharply compressed and then stretched. Thanks to such a pulsating load, static tension and spasm are removed from the muscles, it relaxes, which in itself leads to relief after the first session.
All over the world, the SWT technique is positioned as a non-invasive biosurgery, as it allows to achieve profound changes in the structure of tissues and influence the immediate cause of the pathological process. The mechanism of action of UVT on soft tissue structures is due to the fact that the permeability of cell membranes changes at the site of inflammation. Healthy cells have an elastic membrane with normal permeability. During inflammation, cells have an altered membrane that is tense due to intracellular edema. Soft tissues, consisting of 80% water, transmit the energy of the focused shock wave. The shock wave does not destroy the elastic cell membranes when passing through them. Under the influence of high energy of a focused shock wave, a hydrostatic shock occurs in inflamed tissues, cell membranes changed during inflammation are destroyed - the so-called cavitation (collapse) effect occurs. The substances formed in this process, acting on nerve endings, enhance the breakdown of inflammatory mediators and trigger regenerative processes.
Effect of UVT
- increasing blood flow in damaged tissues and stimulating their regeneration;
- restoration of the structure and elasticity of ligaments;
- relaxation (relaxation of spasming muscles);
- long-term elimination of pain;
- acceleration of metabolism, loosening of microcrystals of calcium salts and areas of fibrosis, restoration of the structure and elasticity of ligaments, elimination of marginal bone growths;
- formation of a new capillary network – neoangiogenesis within 96 hours after the procedure.
The result of balanced work of the TMJ.
A balanced TMJ has a beneficial effect on the body as a whole. With proper functioning of the joint, problems such as headaches, migraines, insomnia, pain in the neck and back, arms, legs, knees, digestive tract disorders, allergies, arthritis, arthrosis, enuresis, and dehydration go away. A balanced temporomandibular joint eliminates physical tension in the jaw muscles, and also allows one to dissipate negative emotions that have been held in the subconscious for a long time. The quality of life improves: a person achieves harmony and balance in his body, acute and chronic stress and fatigue go away. Proper functioning of the TMJ has a beneficial and long-lasting effect on problems associated with pain and injury, and prolonged overexertion.
Based on the above, any dental intervention should begin taking into account a possible global problem, and not just an isolated one. That is, take into account the entire chewing apparatus and the body as a whole, and not just one tooth. After all, by introducing height, the number of teeth and the state of the bite, we break the entire adaptation of the body and make changes to the condition of the body as a whole.
Therefore, at the Prizma Medical Center, shock wave therapy is used at all stages of complex treatment of patients. You can eliminate the causes of bad breath at the Prizma dentistry in Podol.
Who treats TMJ dysfunction?
Degenerative processes in the lower jaw joint are a disease that is treated by dentists and specialists in treating problems of the maxillofacial apparatus, for example, orthodontists and orthopedists. However, the etiological factor may necessitate intervention in the treatment process by specialists from other areas of clinical medicine. Thus, to ensure maximum effectiveness of therapeutic measures, the direct participation of such doctors may be necessary:
- a traumatologist is needed when the temporomandibular joint is displaced due to injury;
- consultations with a neurologist will be needed, first of all, if the facial nerve is pinched, as well as when exposed to many other factors, since the disease often involves nerve endings in nearby tissues and organs;
- a psychologist will be needed to stabilize the patient’s psycho-emotional state if destruction in the lower jaw joint has occurred due to prolonged tension in the facial muscles caused by psychological trauma or stress.
Of course, dental specialists play a leading role in the treatment of temporomandibular joint dysfunction, and representatives of related areas act as consultants.
If you have pathological symptoms, you should immediately contact any specialist, for example, even a therapist. The doctor will definitely conduct an examination and coordinate the patient’s further actions if he detects signs of dental pathology. The variety of manifestations of the disease of the maxillofacial apparatus, in most cases, causes difficulties in diagnosis even for an experienced specialist. An accurate diagnosis is established after additional examinations.
Diagnosis and treatment methods
Inflammatory processes of the TMJ can be diagnosed in the early stages, but this requires timely treatment. Initially, the lesion is localized in the capsule, but as the problem progresses, it spreads to the surrounding tissues. If left untreated, joint mobility may be completely lost.
Diagnosis is made during the initial visit to the dentist. Additionally, consultations with a traumatologist, otolaryngologist, infectious disease specialist and other specialists may be required. The basic methods are CT, radiography, CBCT. Using an x-ray, the dentist is able to determine the presence of arthritis, widening or narrowing of the joint gap. The following types of examinations are also carried out:
- Schüller and Bordes techniques for lateral examination of the affected area;
- plain radiographs;
- layered tomography;
- zonography;
- contrast arthrography;
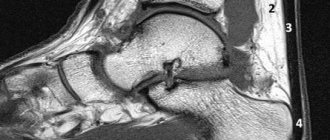
- magnetic resonance imaging;
- diagnostics ELISA (enzyme-linked immunosorbent assay);
- PCR study.
Treatment begins with analyzing the data obtained and drawing up a treatment regimen. The jaw is immobilized and the affected organ is kept at rest for 2-3 days. If necessary, a sling bandage, splint or interdental plate is applied. The patient should follow a semi-liquid diet, relieving tension on the joint. The treatment regimen depends on the form and degree of the lesion; physiotherapy and myogymnastics are usually prescribed.
In the acute form, injections of antibiotics, corticosteroids, and chondroprotectors are prescribed. In case of purulent form, surgical intervention, opening of the cavity, and drainage through an external incision are indicated. Chronic arthritis requires the use of physiotherapy methods, sanitation of the oral cavity and nasopharynx. In some cases, dental prosthetics are indicated.
Differentiation of diagnosis
The symptoms of pathological processes in the joint, which provides movement of the lower jaw, are similar to the manifestations of other diseases. Doctors, using special examinations, must accurately differentiate the diagnosis so as not to miss the development of the following serious pathologies:
- myocardial infarction, which is also characterized by pain radiating to the neck, lower jaw and shoulders;
- otitis media of unknown etiology can be suspected when there is severe pain and hearing loss;
- cerebrovascular accident may occur with dizziness, flashing of flies and nausea;
- cervical and thoracic osteochondrosis are similar in localization of pain;
- pinching of the facial nerve is also caused by unilateral tension of the facial muscles and swelling;
- complicated diseases of the gums and teeth, which are accompanied by inflammation and immobility of the lower jaw.
To avoid making an incorrect diagnosis, the doctor carefully studies the patient’s life history and illness, conducts a visual and palpation examination, and also prescribes the necessary tests.
[slide-anything id=”3470"]
Features of diagnostic measures for TMJ dysfunction
For the most accurate diagnosis of damage to the articular surface of the lower jaw at the junction with the temporal bone of the skull, specialists use the following methods and the following examination plan:
- clarification of the patient’s vital functions (work specifics, presence of chronic diseases, psycho-emotional background);
- questioning the patient about the probable cause of pathological changes in the jaw (trauma, inflammatory processes in the oral cavity, past dental history, the presence of neurological pathologies);
- visual inspection of the outer surface of the projection of the joint and the oral cavity, if possible;
- palpation examination of the joints of the mandible, which helps to identify muscle tension, swelling and displacement;
- listening to sounds when opening the mouth, which can be in the form of clicks or crackling sounds;
- determination of the amplitude of jaw mobility;
- identifying the scope of possible movements;
- assessment of the functionality of the masticatory muscles;
- determining the correct bite;
- X-ray examination of the dentofacial apparatus, which will be the most informative for excluding other pathologies of teeth and gums;
- the magnetic resonance imaging method allows you to examine the soft structures of the jaw, for example, intra-articular cartilage and its physiological position, the correctness of which determines the condition of the TMJ;
- CT scan results will provide a layer-by-layer image of the bone structure of the jaws.
The results of these examinations may require consultation and treatment with a dental surgeon, traumatologist or orthodontist.
What is jaw pain like?
Pain in the jaw usually brings very severe discomfort and anxiety. By nature, they can be acute, sudden, pulsating, or vice versa - aching, chronic, protracted. Often these sensations are so intense that they can even cause a depressed emotional state and depressive disorders [1[1]br> Largely depending on the nature of the pain in the facial area, as well as accompanying symptoms (joint mobility, clicks in it, the presence of swelling, etc. .) depends on why the patient's jaw hurts. During the examination, doctors also pay attention to the localization of sensations - whether they are unilateral or bilateral [1 [1] It is often difficult to determine exactly whether the pain in this area is associated with injury or pathology of the bones, joints, or is caused by some other reason.
Therapeutic measures for diseases of the temporomandibular joint
When an accurate diagnosis of TMJ dysfunction is established, the doctor prescribes a course of therapeutic measures, the features of which are determined by the degree of the pathological process and the etiological factor. The disease requires complex treatment. The most lasting effect in restoring the functions of the maxillofacial apparatus is provided by the following recommendations, methods and means:
- complete exclusion of solid food, which will make it possible to maintain conditional rest for the mandible joint;
- maximum restriction of mobility (no yawning, no talking);
- alternating warm and cold compresses in combination with certain exercises to warm up the joints, which is performed under the supervision of a physiotherapist;
- for pain relief, the doctor prescribes non-steroidal anti-inflammatory drugs in a certain dose and at the recommended dosage interval;
- in case of extremely severe pain, it is possible to take narcotic analgesics;
- muscle relaxants are used to eliminate tension in the muscles of the face, neck and shoulder girdle, if any;
- to restore harmony in the patient’s psycho-emotional background, it is possible to take antidepressants in small dosages;
- physiotherapeutic procedures (laser, electrophoresis with novocaine, ultrasound, radio wave therapy, neurostimulation);
- installation of a special design on the teeth (mouthguard, orthopedic splint), which allows you to prevent the closure of the dentition as much as possible, correct the bite and restore the movement of the TMJ joint in the physiologically correct position;
- orthopedic treatment involves the installation of crowns and bridges to align the dentition and ensure comfortable static and dynamic occlusion;
- avoidance of foods that irritate tooth enamel to prevent relapse of exacerbation;
- a slightly open position of the mouth, which is carried out using the tongue located between the front teeth, will ensure relaxation of the masticatory muscles and jaws;
- in some cases, doctors use the injection of analgesic drugs into the muscle tissue of the projection of the pathological joint.
Complex treatment using the listed methods and means, in most cases, gives a positive effect and long-term remission.