Foot anserine bursitis, also known as anserine bursitis, is an inflammatory disease of the bursa of the joint tendon of the gracilis, sartorius, and semitendinosus muscles. We can find it on the inside of the middle part of the knee joint, 5 cm below the projection of the medial part of the joint space between the pes anserine tendons.
What is pes anserine bursitis of the knee joint?
When crow's foot bursitis develops, it is difficult to understand what it is. The articular bursa (joint bursa) is located between the collateral-medial ligament and the tendon junction on the inside of the knee joint. Often, inflammation of this articular bursa is confused with a sprain or rupture of the collateral-medial ligament due to the similarity of symptoms.
Another name for this disease is anserine bursitis (BA). The development of the inflammatory process of the bursa can be caused by trauma directly in the area where it is located, increased friction caused by a number of reasons (osteoarthritis, infectious arthritis). Bursitis of the anserine bursa is considered a secondary form of the disease.
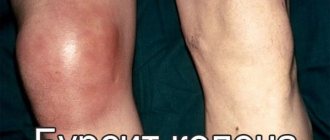
The disease is an inflammation of the knee joint
Anatomy
Anatomy of a crow's foot
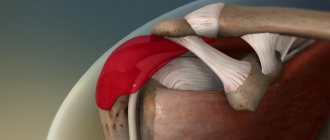
The anserine bursa, or crow's foot bursa, is a sac filled with fluid. It secretes synovial fluid to reduce friction between tissues and also serves as a shock absorber for bones, ligaments and muscles. Inflammation of the bursa does not occur suddenly, but develops over a long period of time. Bursitis can also occur in the joints of the shoulder, knee, hip, elbow and thumb.
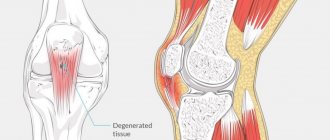
The pes anserine is the insertion site of the combined tendon of the sartorius, gracilis, and semitendinosus muscles on the superomedial portion of the tibia. The three pes anserine tendons are located superficial to the medial collateral ligament (MCL) of the knee. The sartorius and gracilis muscles are hip adductors (that is, they bring the thigh toward the median axis of the body). The semitendinosus muscle is part of the hamstring group and is located on the back of the thigh. Together, these three muscles are the flexors and pronators of the knee.
The main reasons for the development of anserine bursitis
The “crow's foot” on the leg carries shock-absorbing and stabilizing functional loads. Prevents joint instability and prevents excessive rotational movements of the joint. Direct injury to the anserine bursa is difficult.
The causes of the development of the disease are previous diseases of various etiologies and localizations:
- infectious, purulent arthritis;
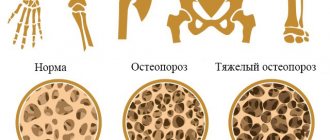
- DOA (deforming osteoarthritis);
- consequences of knee joint injuries;
- dysfunction of the tendon-ligamentous apparatus;
- autoimmune diseases (lupus erythematosus, rheumatoid arthritis);
- endocrine diseases (diabetes);
- excessive body weight;
- acquired or congenital flatfoot;
- pathological disorders of the development of the muscular and bone structure of the skeleton;
- penetration of pathogenic flora from a nearby inflammation site by hematogenous route.
Disease prevention
To reduce the risk of developing the disease, it is recommended to follow some simple rules:
- wear comfortable shoes;
- if you need to increase physical activity, do it gradually;
- stretch your muscles before and after workouts.
Do not self-medicate or try to diagnose yourself! If you have any suspicions about the development of the disease, consult a specialist!
Attention!
The information on the site does not constitute a medical diagnosis or a guide to action and
is intended for informational purposes only.
Forms and types of disease
The form of the disease “crow's foot” of the knee joint is determined by the anatomy of the localization of the affected bursa - the anserine bursa.
The disease is divided into two types - deep and superficial
Such bursitis is classified according to the factors of its development into four types:
- Aseptic, in which inflammation is caused by excessive mechanical stress or friction. Causes excessive production of synovial fluid and its accumulation in the cavity of the articular bursa. This type of disease has the most favorable prognosis.
- Infectious (purulent), caused by the invasion of virulent flora into the anserine bursa by blood flow or by an open wound. Without proper treatment it leads to sepsis. Requires treatment in a medical facility under the supervision of a physician.
- Post-traumatic, developed through injury to tendons, ligaments, articular surfaces, muscle fibers of varying severity.
- Caused by the appearance of osteophytes or the accumulation of calcium salts. It is a complication of chronic arthrosis.
Symptoms
Symptoms of damage to the joint capsule are not always clear enough to allow one to accurately determine which disease is causing them. The most characteristic symptoms of this disease include:
- pain on the inside of the knee;
- increased pain when moving the joint;
- increased pain with significant physical exertion.
Olecranon bursitis
It is worth immediately noting that such symptomatic manifestations are not uncommon in other equally dangerous diseases of the joints.
Considering that bursitis of the knee joint is accompanied by an inflammatory process, patients may experience a slight increase in body temperature.
In rare cases, mild swelling may be added to the above symptoms. Only a doctor can determine the presence of bursitis during an external examination, so it is very important to contact him at the first signs of this joint disease, treatment in this case will be more effective.
Main risk factors
The presence of risk factors in everyday life may contribute to the appearance of inflammation of the anserine bursa:
- Professional affiliation - the work of workers, construction workers, agricultural workers, associated with prolonged kneeling positions.
- Belonging to professional sports. The disease affects weightlifters, wrestlers, weightlifters, football players, and skiers. There is a direct correlation between the appearance of bursitis and excessive physical activity.
- Hereditary predisposition.
- Congenital pathologies and developmental anomalies of the musculoskeletal skeleton and tendon apparatus.
- History of autoimmune disorders.
- Hormonal imbalance. In women during menopause, as well as during long-term treatment with steroid hormones.
- Sudden and prolonged hypothermia of the lower extremities or the body as a whole.
Risk factors include: occupation, congenital pathologies
Treatment
Like any other type of inflammation of the periarticular bursa, the disease is treated with anti-inflammatory non-steroidal drugs .
The doctor prescribes a medication regimen depending on the intensity of symptoms. In addition, glucocorticosteroids may be prescribed for injection into the synovial bursa.
During treatment, it is necessary to ensure rest for the diseased joint and minimize all physical stress on it.
Passive physiotherapy , including ultrasound with hydrocortisone, has a beneficial effect. In order for the treatment to be as effective as possible, the load on the affected knee should be reduced as much as possible during the period of active tissue restoration.
After all the symptoms have subsided, you can gradually introduce loads by doing physical therapy.
Symptoms
The disease has a characteristic clinical picture, which includes the following symptomatic manifestations:
- pain in the inner part of the knee joint, which increases when climbing up a hill or up steps;
- swelling localized below the knee fossa;
- increased sensitivity of the knee;
- sensation of a foreign body inside the joint;
- hyperemia of the skin at the site of inflammation;
- deterioration of general condition;
- decreased range of motion or limited joint mobility;
- the development of muscle atrophy caused by sparing the diseased joint.
Manifestations of the disease depend on the reasons that caused its appearance. A differentiated diagnosis is established taking into account diseases with a similar clinical picture.
Symptoms vary from the causes of the disease
Kokurkin G.V., Karalin A.N., Nikolaev S.A., Romanova L.A.
Chuvash State University named after. I.N. Ulyanova
Cheboksary
Diagnosis of crow's feet syndrome
When examining the knee joint, its contours may not change. There is little or no effusion. When palpating, it is necessary to superficially stroke the anterior and posterior surfaces of the joint with four fingers. At the same time, in the area of the posterior internal surface of the joint, the sliding of the fingers seems to slow down, and hyperthermia can be detected. This indicates a violation of the trophism of the skin in the area of the inner surface, the posteromedial part of the knee joint. Superficial palpation of the knee joint causes pain in the area of the “crow’s foot” of the anatomical structures that form it (myoenthetic apparatus).
At the same time, the patient Fr. Palpation of other areas of the joint, even if accompanied by pain, does not give such a strong reaction from the patient.
With deep palpation, a dense, sharply painful ridge is detected along the m. semimembranosus et. m. semitendinosus, in which individual compactions, cords, etc. can be identified. (nodules of Müller, Cornelius). Directly in the crow's foot area, you can sometimes palpate a swelling of a tight-elastic consistency that is painful to the touch. This is reactive bursitis of one of the bursae in the “crow's foot” area.
Movements in the knee joint, passive and active, may be accompanied by pain in the area of the “crow’s foot” and the myoenthetic apparatus that forms it. This is especially evident if you resist the movement of the lower leg at the moment of its flexion (symptom No. 3). As a rule, the patient has a flexion contracture (a method for diagnosing contracture of the knee joint, including relaxation of the muscles of both lower extremities under the influence of its own weight, visual comparison of the spatial position of the apices of the anterior surfaces of the knee joints, provided that both limbs of the patient are placed in a sitting position on the buttocks without support on the hips, in a horizontal position with emphasis on the heels and the tops of the posterior surfaces of the heel areas, provided that both limbs of the patient are placed outside the supporting surface, on which the patient is laid in a prone position so that the upper thirds of the thighs of both limbs are on the edge of the supporting surface, and if differences in the spatial position of the vertices are identified, contracture of the knee joint is diagnosed).
This can be very clearly identified using the following techniques (Symptom No. 1): the patient is laid on the couch on his stomach, his legs at the level of the third hip lie on the edge of the couch. A normal knee joint extends up to 180°, and in women even more. The diseased joint is in a position of flexion contracture of varying degrees. Second symptom No. 2: the patient sits on a chair, the limbs are in a state of complete relaxation, with emphasis on the heels, placed on a second chair. In this case, the healthy knee joint extends to 180° (or more), and the diseased joint remains in a position of flexion contracture. Both symptoms are very obvious and demonstrative. They are observed in 100% of these patients. (Symptoms No. 1 and No. 2 can serve as a test of the severity of the syndrome: an increase in flexion contracture and the effectiveness of treatment (dynamic changes in contracture).
Well-known symptoms of “Lassegue”, palms (A.M. Land’s symptom) - they are most often caused by the rigidity of the muscles of the “crow’s foot” area.
Of the instrumental methods for diagnosing periarticular lesions, thermographic research is used, based on the difference in temperature gradients (d T). An increase in d T is observed with synovitis and periarthritis, but its value with periarthritis is much lower.
For accurate topical diagnosis of periarticular lesions, arthrosonography of joints is successfully used, which helps to identify the presence of exudate in bursae and synovial sheaths, latent ruptures of tendons and ligaments, and to see the exact localization of the source of inflammation.
As an illustration, we present one of our observations.
reference number 879. Patient:
Nikolaeva G. M. born 1959
Complaints
: pain in the area of the right knee joint, instability in the joint. The pain is localized in the area of the medial part of the joint, intensifies with load on the joint, appears in the morning, when starting to walk, in the form of a pulling character along the back surface of the lower leg. Sometimes there is swelling of the joint.
History of the disease:
three years ago there was an operation: meniscectomy. In the postoperative period, the pain that was there before the operation and was of the nature described above reappeared. The treatment had no effect. A diagnosis was made - disease of the operated meniscus, incomplete removal of the meniscus (the posterior horn remained), postoperative synovitis. Repeated surgery is recommended - arthrotomy and joint revision.
Consultation on January 24, 1996. Upon examination:
walks with a limp on the right lower limb. When examining the knee joint, its contours are not disturbed. There is a scar in the projection of the internal joint space. When stroking the front and back surfaces of the joint, there is a violation of the gliding of the fingers in the “crow's foot” area. On a healthy joint, this sign of trophic changes in the skin is absent.
When palpating the joint, pain is detected in the area where the “crow’s foot” forms and above it along the m. semimembranosus et. m. semitendimosus (in the projection n/3 of them and compaction of subcutaneous tissues). Other parts of the joint are painless. Positive symptoms of flexion contracture (Symptom I and II) and functional load (Symptom 3, increased pain in the “crow’s foot” area), with active flexion of the leg with increased intensity.
The X-ray shows grade II deforming arthrosis. There are also all the clinical signs of crow’s foot syndrome after meniscectomy, including characteristic, pathognomonic symptoms:
1. Symptom of trophic disorders of the knee in the “crow’s foot” area (slip disorder). 2. Symptom of flexion contracture (Symptom I and II).
3. Symptom of functional load (Symptom III).
Based on clinical data, a diagnosis was made: Crow's foot syndrome of the right knee joint. Deforming arthrosis of the knee joint, stage II. Treatment is conservative. The outcome is positive.
In the above clinical observation, the patient developed a typical picture of crow's foot syndrome after surgery. Initially, as a pathological reaction of the myoenthetic apparatus, forming the “crow’s foot” area to macrotrauma of the knee joint without a pronounced clinical manifestation. Subsequently, it was aggravated by a violation of the supporting function of the joint due to damage to the meniscus and surgery - meniscectomy. Moreover, the degree of functional impairment gradually progressed, because deforming arthrosis developed, which further impaired the spring function of the joint. All together led to the development of chronic functional insufficiency of the joint, which increased the load on the area where the “crow’s foot” forms and aggravated degenerative-dystrophic changes in it. As a result, a focus of chronic muscle hypertonicity arose in the area of crow's foot formation with a characteristic clinical picture.
Thus, the treatment eliminated the pain syndrome and improved the functional result, but the primary intra-articular cause of the pathology (deforming arthrosis) and the focus of postoperative irritation (scars) remained. They require independent treatment. In addition, an unloading orthopedic regimen is necessary, surgical reconstructive intervention on the joint for deforming arthrosis is possible, since in the presence of these pathological conditions of the joint there is a constant load of exacerbation of the “crow's foot” syndrome under any provoking factor: microtraumatization, macrotrauma, functional overload, increasing postural overloads associated with changes in statics due to the progression of joint deformation due to deforming arthrosis.
Diagnosis of anserine bursitis
It is important to correctly differentiate the diagnosis. When establishing it, a qualified orthopedist-traumatologist relies on an objective clinical picture, palpations and complaints of the patient.
To clarify the diagnosis, laboratory and instrumental studies are prescribed:
- physical examination - stress test;
- blood test with leukocyte formula;
- test for rheumatic factor;
- blood test for uric acid levels;
- X-ray of the knee joint;
- Ultrasound of periarticular tissues;
- MRI;
- puncture and culture of synovial fluid.
Diagnosis at the initial stage of the disease allows you to reduce the duration and intensity of treatment and speed up the recovery process.
X-ray of the knee joint
First aid
When you are concerned about pes anserine bursitis, you need to know the rules of first aid:
- Complete immobilization (ensuring immobility) of the knee joint. The maximum period if it is not possible to go to a medical institution is no more than 10 days.
- Cold compress. It is necessary to apply ice packs and apply cooling ointments.
- The use of pharmaceutical or self-made compression products (elastic bandages, tight bandages from improvised means, compression stockings, knee pads). Allows you to reduce pain.
- Ensuring that the limb is elevated to reduce swelling.
First aid for joint pain
Just in case, keep ice in the refrigerator so you can quickly make a cold compress.
First aid should be taken independently if it is not possible to visit a doctor. To relieve pain, apply a cold compress several times a day for 20 minutes. It is better not to take oral medications on your own; you need to know the exact dosage, which can only be indicated by your doctor. Ointments can be used simultaneously with the use of cold compresses. To relieve pain and relieve inflammation a little, use the following products for external use:
- "Ibuprofen";
- "Diclofenac";
- "Voltaren Emulgel";
- "Bystrumgel";
- "Indomethacin ointment";
- "Dolgit";
- "Nise";
- "Ketonal";
- "Deep Relief"
Hot compresses cannot be applied. If purulent inflammation is present, a hot compress will aggravate the patient's situation. A sore knee needs rest. It is necessary to reduce the load on the injured knee.
How to get rid of the disease?
An inflamed crow's foot in the knee joint causes suffering to the patient, causes lameness, and reduces ability to work. To get rid of the disease, you need to contact a specialist in the field of orthopedics and traumatology.
Once a crow's foot joint has been diagnosed, treatment consists of a set of measures:
- Elimination of the causes that caused the appearance of the disease - treatment of achillobursitis, diseases of the bone joints of infectious etiology.
- Conservative methods of influence. It includes medication, physiotherapy (magnetic, shock wave, UHF, cryotherapy, kinesitherapy, mud therapy, electrophoresis with novocaine, therapeutic gymnastics).
- Surgical treatment – puncture, bursa aspiration, excision. The indication for surgical intervention is the absence of positive dynamics after conservative therapy and the development of complications of the disease.
- Non-traditional treatment as an auxiliary method of influence.
Physiotherapy is part of the treatment of bursitis
Medications
Drug therapy can reduce pain, swelling, stop the process of inflammation at the initial stage of development, and prevent the development of a chronic form of the disease and the appearance of complications.
For these purposes, the following is used in medical practice:
- NSAIDs have the ability to relieve pain, fever and slow down the progression of inflammation (Ibuprofen, Nimid, Ketoprofen, Movalis, Meloxicam).
- Steroid hormones relieve acute pain and stop inflammation (Kenalog, Diprospan, Depo-Medrol).
- Antibacterial drugs - antibiotics, are prescribed depending on the pathogen and resistance.
- Muscle relaxants that reduce muscle tension (Mydocalm, Mefedol).
- Anesthetics, by blocking the affected area (Novocaine, Lidocaine).
Before using medications, it is necessary to consult a doctor to clarify the dosage of the drugs and the duration of therapy.
Medicines are the main method of treating pes anserine of the knee joint
Unconventional treatment
Methods, remedies, recipes of traditional medicine are not an independent therapeutic method. This type of therapy is used as an auxiliary therapy at the initial stage of the disease or in the absence of the opportunity to visit a doctor.
The active ingredients used in alternative medicine are:
- plant materials – fresh and dried parts of plants (leaves, inflorescences, fruits, bark, needles, rhizomes, stems);
- raw materials of animal origin (butter, lard, goat fat);
- bee products (propolis, honey, wax, dead wood);
- healing mud.
Based on the above active ingredients, the following is prepared:
- decoctions, infusions;
- tinctures, rubbing;
- compresses, applications, wraps;
- baths, lotions;
- creams and ointments.
Alternative treatments are:
- hirudotherapy (treatment using medical leeches);
- treatment with bee stings (apitherapy);
- manual, reflex therapy;
- acupuncture.
Before using alternative medicine methods, you need to make sure that there is no allergic reaction to the components included in the folk remedies.
Prevention of pathology
Following a set of simple rules will help prevent the occurrence of this disease:
- Avoid overloading the knee joint, ligaments and tendons.
- Treat infectious and viral diseases in a timely manner.
- Prevent lower extremity injuries.
- When playing sports, increase the load gradually, and before training, do a warm-up to warm up the muscles.
- Purchase and use shoes with low heels.
- If symptoms characteristic of this disease appear, immediately visit a doctor.
- Maintain constant control of body weight.
Diagnostics
Lateral radiographs of the patient's knee help rule out stress fracture, arthritis, and osteochondritis dissecans. MRI is necessary when it is necessary to clarify whether there are other damage to the medial surface of the knee joint. Also, MRI will allow you to do without arthroscopy. The MRI image must be compared with the data obtained as a result of the physical examination. Sinusography (radiography of the sinus after administration of a contrast agent) is the best assistant for making a diagnosis if other imaging methods, including MRI and CT, are not feasible for some reason. Injections of lidocaine/corticosteroids into the bursa area are possible, which will help assess the contribution of this pathology to the overall structure of the pain syndrome of the knee joint.
Rating scales
Lower Extremity Functional Scale (LEFS)
Physical examination
The pes anserine bursa can be palpated at a point slightly above the tibial tuberosity and 3-4 cm medially (about two finger widths).
Palpation of the crow's foot bursa
Examination of hamstrings should be carried out in the supine position. Flex the patient's hip 90° and then extend the knee as far as possible. The degree of knee extension will be an indicator of the length and tone of the hamstrings. If the patient's knee straightens completely, the hamstring is not constrained.
Estimating the length of hamstrings
If bursitis occurs due to sports activities, symptoms can be reproduced by resisting internal rotation and flexion of the knee. In the chronic version in older people, bending or straightening the knee usually does not cause pain.