Suprapatellar bursitis affects the knee joint approximately 3-4 days after injury or increased physical activity. Clinically, it manifests itself as pain, aggravated by walking, swelling, and limited mobility. Treatment of suprapatellar bursitis is predominantly conservative. But when purulent exudate accumulates in the cavity of the knee joint, surgical intervention is required.
General information about the disease
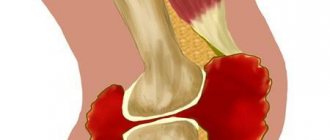
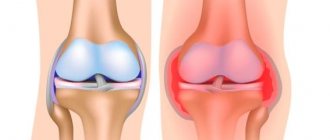
Suprapatellar bursitis is an inflammatory lesion of the suprapatellar bursa, which is located at the junction of the knee cartilages. This joint structure plays the role of a kind of shock absorber. The suprapetellar bursa protects the tendon from excessive mechanical stress, such as friction or compression. Normally, there is always a small amount of liquid in it. With bursitis, its production increases so much that a tumor-like compaction forms in the knee area. The liquid presses on the inner walls of the bag, which leads to the development of an acute inflammatory process.
Anatomy of knee rolls
The anatomy of inversion of the knee joint is due to the fact that the synovial membrane, when covering the surface of the condyles of the femur and tibia, forms the internal sinuses. They contain a small amount of synovial fluid, which, in the absence of pathological deformations of the membrane, circulates freely.
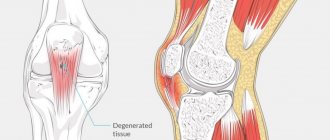
Synovial inversions of the knee joint increase the internal articular cavity, ensure uniform distribution of the shock-absorbing load and prevent the bone tissue from being subject to traumatic effects of movement. With the development of diseases (arthritis, arthrosis, bursitis, tendinitis, ruptures of ligaments and tendons, blood, serous effusion, fibrous exudate accumulate in the cavities of these volvuluses. They become inflamed and stimulate long-term circulation of the infectious agent.
The main inversions of the synovial membrane of the knee joint:
- recessus genus superior is located in the projection between the patella and the condyle of the femur from above;
- medialis recessus genus and lateralis recessus genus – medial and lateral pockets located on the top sides of the knee joint;
- below, between the condyles of the bones, the lower medial and lateral inversions are located;
- two back lower pockets;
- two rear top folds.
Anatomically, the posterior formations do not have a connection with the anterior ones. Therefore, when performing a diagnostic puncture, the doctor often tries to first check the contents of the anterior cavities, and then move through the canals to the rear. In this way, it is possible to determine with high accuracy the expected location of ligament rupture, inflammation of articular synovial bursae, etc.
Why does pathology appear?
Another name for suprapatellar bursitis is “nun’s knee.” Church workers often suffer from this inflammatory pathology due to prolonged kneeling during the day. Bursitis develops as a result of repeated microtraumas and overloads of the joint. Since the suprapatellar bursa is located close to the surface of the skin, even a minor single household or sports injury can provoke its inflammation. Factors predisposing to the appearance of bursitis include the following pathologies:
- rheumatoid arthritis, scleroderma;
- gouty, infectious, reactive arthritis;
- endocrine diseases, including diabetes mellitus, hypothyroidism;
- some renal pathologies;
- metabolic disorders;
- deforming osteoarthritis (gonarthrosis);
- stagnation of lymph in the knee joint;
- varicose veins, atherosclerosis, obliterating endarteritis.
Allergic reactions and the use of glucocorticosteroids can provoke inflammation. Infectious suprapatellar bursitis, which develops against the background of sepsis, osteomyelitis, phlegmon, and furunculosis, is also diagnosed.
Symptoms of pathology
In orthopedics and traumatology, acute and chronic suprapatellar bursitis are distinguished. The reason for the development of the latter is the patient’s ignorance of the symptoms characteristic of the initial stage of inflammatory pathology.
For acute bursitis
This form of the disease can manifest itself with moderate or severe symptoms. A round elastic seal is formed in the knee area. When you press it, you feel movement inside the liquid (fluctuation). The skin turns red, swells, smoothes, and becomes hot to the touch. The damaged knee increases in size compared to the healthy joint. The following symptoms also occur:
- pain increases when walking, going up or down stairs, flexing and straightening the joint;
- range of motion decreases.
Infectious suprapatellar bursitis is especially severe. Pathogenic microorganisms that penetrate the joint cavity release toxic products of their vital activity into the surrounding space. As a result, signs of general intoxication of the body appear. These are elevated body temperature, chills, excessive sweating, and in weakened patients - gastrointestinal disorders.
For chronic bursitis
The pathology that has taken a chronic form manifests itself with significantly less severe symptoms. An elastic formation is felt in the knee area, slightly painful when pressed. There is a feeling of stiffness when walking. The pain is mild, intensifying after a sudden change in weather, increased physical activity, hypothermia, or exacerbation of other chronic pathologies. Sometimes, usually in the evening, the knee swells, the local temperature rises, and hyperemia is observed.
Diagnostics
The diagnosis is made on the basis of specific external signs, medical history, and patient complaints. A series of functional tests are performed to assess range of motion and sensation. A puncture of the joint is performed to collect fluid and examine it further. This allows you to determine the nature of the inflammation and exclude infection of the joint capsule. The following instrumental studies can confirm the diagnosis:
- MRI to assess the condition of soft tissue structures of the knee, blood vessels, nerve trunks;
- arthroscopy to examine the inner surface of the knee joint;
- Ultrasound to determine the localization of the inflammatory process.
If an autoimmune disease is suspected, serological and biochemical studies are performed. The level of antinuclear antibodies, C-reactive proteins, and rheumatoid factor is determined.
Surgery
Surgical treatment is practiced in two cases - severe swelling and infectious inflammation. In the first case, it is necessary to reduce the fluid pressure inside the joint for a speedy recovery; in the second case, you need to install drainage and cleanse the cavity of purulent contents.
To reduce fluid pressure, a puncture is sometimes sufficient. For infectious inflammation, the doctor makes an incision about 3 cm long and then inserts a catheter into the bursa. Purulent contents are pumped out through it, and then the cavity is treated with an antibacterial solution. Additionally, the patient is prescribed antibiotic tablets to treat bursitis and prevent the recurrence of pus in the joint capsule.
How to treat suprapatellar bursitis of the knee joint
Treatment methods for acute and chronic disease differ. In the latter case, medications and physiotherapy are used mainly. In the acute course of the pathology, patients are advised to use a gentle motor regimen that eliminates stress on the knee. While walking, it is recommended to wear knee pads with hard metal or plastic inserts. Cold compresses are required. Every hour, an ice pack wrapped in thick cloth is applied to the joint for 10 minutes. This helps prevent inflammation from spreading to healthy tissue.
Conservative therapy
An integrated approach to conservative treatment is practiced using local and systemic medications and physiotherapeutic procedures. The main goals of therapy are the complete elimination of symptoms and the causes of their occurrence.
Drug treatment
Non-steroidal anti-inflammatory drugs are always the first choice. NSAIDs relieve acute and chronic inflammation, reduce the severity of pain, and promote the resorption of edema. Depending on the form of suprapatellar bursitis, therapeutic regimens include drugs in various dosage forms:
- solutions for parenteral administration - Movalis, Lornoxicam, Ortofen, Ketorolac;
- tablets - Diclofenac, Ketoprofen, Nimesulide, Ketorol, Ibuprofen;
- ointments and gels - Indomethacin, Fastum, Voltaren, Artrosilene, Finalgel.
External agents with a cooling effect are also used to relieve pain. This is Bom-Benge ointment, Ben-Gay with menthol. Antibiotic therapy is carried out when pathogenic bacteria are detected in the exudate. Patients are prescribed a course of cephalosporins (Cefazolin, Ceftriaxone), macrolides (Clarithromycin, Azithromycin), semisynthetic penicillins (Amoxiclav, Panclave) for 2-3 weeks.
Physiotherapeutic methods
Carrying out physical procedures helps to increase the body's susceptibility to drug treatment. The impact of physical factors on the inflamed suprapatellar bursa helps to quickly relieve inflammation, eliminate pain and limited mobility. The following physiotherapy procedures are most often used in the treatment of pathology:
- magnetic therapy;
- diadynamic currents;
- applications with ozokerite and paraffin;
- ultraviolet irradiation;
- UHF therapy;
- ultrasound;
- mud therapy.
In the acute and subacute period, to eliminate severe pain, patients are prescribed electrophoresis with glucocorticosteroids, anesthetics, and analgesics. For chronic bursitis, this procedure is carried out with B vitamins, chondroprotectors, and solutions of calcium salts.
Surgery
Despite their high therapeutic efficacy, systemic NSAIDs act nonselectively. Only a certain dose of drugs penetrates into the cavity of the knee joint. Therefore, in some cases, such drug treatment does not give a positive result. The patient is indicated for surgical intervention. The doctor inserts a thin needle into the cavity of the suprapatellar bursa and removes the accumulated exudate. He then rinses it with antiseptic solutions and then treats it with glucocorticosteroids. The post-traumatic wound is drained, and the knee is fixed with an elastic bandage. Patients are prescribed bed rest for 2 days.
The ineffectiveness of conservative therapy for sluggish chronic bursitis over several months becomes an indication for excision of the suprapatellar bursa. During the rehabilitation period, which lasts 2-3 weeks, physiotherapy and physical therapy classes are carried out to restore the functions of the joint.
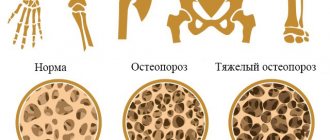
Therapeutic diet
Following a therapeutic diet can significantly speed up recovery by improving metabolism and accelerating recovery processes in the knee joint. It is necessary to limit foods high in fat and simple (“empty”) carbohydrates in your diet. These include semi-finished meat and fish products, fast food, confectionery and sausages, and baked goods made from wheat flour. Instead, you should include the following products in your daily menu:
- low-fat cheeses, cottage cheese, Varenets, kefir, fermented baked milk, containing a lot of calcium;
- fatty sea fish (salmon, herring, smelt) - a valuable source of polyunsaturated fatty acids and fat-soluble vitamins;
- fresh vegetables, fruits, berries, herbs, which contain a lot of vitamins, microelements, pectins.
Nutritionists recommend that patients with bursitis, in the absence of contraindications, drink at least 2.5 liters of fluid daily. This is clean water, lightly salted mineral waters (Slavyanovskaya, Nagutskaya, Essentuki No. 2), fruit compotes, berry fruit drinks, vegetable juices. Drinking plenty of fluids helps remove toxic products of the inflammatory process from the body.
Folk remedies
Remedies prepared at home according to traditional medicine recipes are used after conservative therapy or surgical treatment. They are used primarily for chronic bursitis during the recovery period. The ingredients of ointments, oil tinctures, herbal teas, infusions and decoctions can eliminate mild discomfort that occurs during increased physical activity. But you cannot use folk remedies with a warming effect, as this can cause inflammation to spread to healthy joint structures.
| Folk remedy for the treatment of suprapatellar bursitis | Recipe and method of use |
| Pain relieving ointment | In a mortar, grind a tablespoon of thick honey and aloe juice, add 15 drops of linseed or olive oil. Without ceasing to mix, add 50 g of Vaseline and fatty baby cream in small portions. Place the ointment in a glass jar, store in the refrigerator, and rub into the knee for pain. |
| Decongestant compress | Pour a tablespoon of dry crushed elecampane roots with 1/2 cups of boiling water. After an hour, strain and moisten a wide gauze napkin into the infusion. Apply to the sore knee for an hour |
Folk remedies
Compresses will help relieve swelling and reduce pain
Suprapatellar bursitis is a complex disease that requires urgent drug therapy. Treating the disease with folk remedies is unsafe. In the case of purulent inflammation, traditional medicine methods can only do harm.
You can use the recipes below only if the inflammation is non-infectious. It is recommended to first agree on the possibility of self-treatment with your doctor.
- To reduce swelling, take a few pieces of ice, wrap them in a towel, and apply a compress to your knee for 15-20 minutes. The manipulations should be repeated 2-3 times a day.
- Soak a towel in alcohol tincture of propolis and rub the sore knee. Movements should be soft and smooth.
- Dissolve a tablespoon of sea salt in a glass of warm water. Moisten a gauze compress in the resulting solution and apply to the sore knee for half an hour.
- Grate the onion, mix the resulting gruel with two tablespoons of honey and apply to the sore knee, securing with a bandage. You need to keep the compress for half an hour.
To speed up recovery, it is recommended to combine folk remedies with drug therapy. If you have infectious bursitis, you should never use local irritants, as this can lead to the spread of infection.
Consequences of lack of treatment
The chronic form of suprapatellar bursitis is especially dangerous. A person gets used to a certain limitation of mobility and rare mild pain, so he does not consult a doctor. Meanwhile, the inflammatory process in his knee joint slowly progresses, in which nearby connective tissue structures are gradually involved. What are the consequences of lack of medical intervention:
- scarring of the quadriceps femoris muscle, damage to its fascia and tendons;
- destruction of the cartilage layer of the knee with the subsequent development of deforming osteoarthritis;
- formation of cysts in the articular cavity;
- displacement of the kneecap, instability of the joint.
The inflammatory process is accompanied by the deposition of fibrin, which causes thickening of the walls of the suprapatellar bursa, proliferation of its tissues and a decrease in functional activity.
Symptoms
Different bursae become inflamed under different conditions. The bursa directly above the kneecap can be damaged by a fall on the knee. In this case, there is a high probability of wound infection, resulting in the development of suprapatellar bursitis of the knee joint.
Inflammation of the synovial bursa under the kneecap occurs after injury to nearby tendons - for example, as a result of an unsuccessful jump from a height with straight legs. Inflammation on the lower inner side of the knee is typical for women over 40 years of age who are overweight. Bursitis can also occur as a complication of gout, osteoarthritis, and infectious diseases.
Symptoms appear gradually, as follows:
- An increase in the volume of the knee joint without the appearance of severe pain and while maintaining the normal range of motion.
- Local increase in temperature and redness at the site of inflammation.
- Joint pain and limited mobility.
- In the case of bursitis development, a complication is an exacerbation of the symptoms of the underlying diseases.
Experts' forecast
When a patient seeks medical help with complaints about the appearance of the first signs of bursitis, the prognosis is favorable. Timely conservative treatment allows you to fully restore all functions of the knee. If complications develop, the prognosis is less favorable, especially if surgical intervention is necessary. Despite the proper execution of the operation, areas with rough fibrous tissues form in the joint cavity, so in the future there may be a disruption in the functioning of the knee.
Disease prevention
The main prevention of pathology is to exclude traumatic situations. During sports training or increased physical activity, it is necessary to wear elastic knee pads or bandages. They reliably fix all structures of the knee and soften impacts when falling. Orthopedists and traumatologists recommend prompt treatment of respiratory, intestinal, and urogenital infections, the pathogens of which can provoke inflammation of the suprapatellar bursa. You need to take balanced complexes of vitamins and microelements daily to strengthen bone and cartilage tissue, ligaments, tendons and muscles.