Publication date: March 13, 2021.
Date the information on this page was updated: October 04, 2021.
TMJ dysfunction is a fairly common pathology these days, as it is largely caused by stress factors. Here it can be difficult to understand what is primary and what is secondary, because people with joint dysfunction usually come with bite pathology, pathology of the musculoskeletal system (curvature of the spine, neck). Therefore, joint treatment is a complex story. It happens that the primary pathology is a pathology of the joint, and sometimes it is the musculoskeletal system.
Why do patients experience TMJ dysfunction?
Pathology, first of all, arises against the background of problematic functioning of the complex (hinge-shaped) joint connecting the upper and lower jaws.
There can be several causes of TMJ pathology:
- malocclusion;
- constant stiffness of the facial muscles as a result of neuropsychic or physical stress;
- absence of a chewing tooth or several units of chewing groups in the mouth;
- tendency to increased tooth wear;
- mechanical injury;
- poor-quality installation of prostheses;
- problems with the spine (for example, scoliosis);
- the habit of chewing on one side, thereby loading the TMJ;
- birth injuries;
- mistakes when installing fillings and treatment in the past;
- incorrectly selected orthodontic treatment in the past;
- anatomically incorrect structure of the joint (for example, when the shape and size of the articular head and the articular fossa of the TMJ do not correspond to each other).
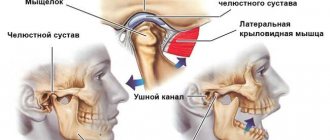
Structure and functions of the temporomandibular joint
The joint is formed by the head of the horn of the lower jaw and the articular surface (fossa) of the temporal bone. Between these bone formations there is a fibrous intra-articular disc, which is fused on all sides with the joint capsule. Ligaments and muscles help keep the joint in the correct position. They limit the range of motion in the joint. Attempting to exceed this functional limitation causes pain and prevents damage to the TMJ.
The main function of the joint is to ensure movement of the lower jaw in three directions:
- vertical: opening and closing the mouth;
- horizontal: lateral displacements of the lower jaw relative to the upper;
- sagittal: movement of the lower jaw back and forth relative to the upper.
The combination of movements of one jaw relative to the other allows us to chew, speak, and express emotions through facial expressions.
How does TMJ dysfunction manifest?
Manifestations of the disease cannot be ignored:
- Clicking sounds when opening the mouth and when at rest. The sound can be heard not only by the person with the problem, but also by those around him. In this case, the joint itself may not hurt. The clicks are especially audible when yawning and opening the mouth wide;
- Blocking or “jamming” of the TMJ. A problem that occurs when the mouth opens suddenly. To open the mouth wide enough, a person needs to adapt to the position of the joint, as if to “catch” it. Also, when jammed, the jaws do not “unclench”, but after such precedents they begin to close and open differently;
- Pain. It can be projected not only in the area of the joint, but also in the neck, entire mouth, back, shoulder and even arm. The pain occurs either suddenly or with prolonged chewing, often disturbing at night.
Also, in the absence of long-term treatment for disorders of the TMJ, the patient may experience headaches, dizziness, weakness, pressing sensations behind the eyes, squeaking in the ears, sleep disturbances, increased nervousness, etc.
When treatment is not provided, long-term degenerative processes occur:
- Firstly, the intra-articular disc is constantly subject to dislocation;
- Secondly, over time the disk changes its shape and wears out;
- Third, the ligament that holds the disc in place becomes thinner over time and can tear.
Classification of TMJ diseases
1. Musculo-articular dysfunctions associated with dysfunction of the masticatory muscles:
- muscle contracture;
- hypertrophy of individual masticatory muscles;
- myositis.
2. Associated with functional and morphological disorders in the joint:
- incorrect position of the head and disc of the joint;
- subluxation or dislocation of the articular head;
- subluxation or dislocation of the articular disc with reduction;
- thinning and perforation of the disc;
- hypermobility of the articular head;
- prolapse (prolapse) of the articular disc (disc dislocation without reduction);
- diseases caused by inflammation of the tissues of the joint capsule, synovial membrane, and retrodiscal zone (arthritis);
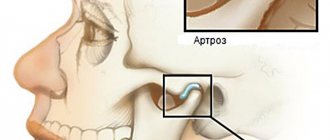
- chronic arthritis, arthrosis;
- ankylosis.
3. Anomalies and acquired diseases of the TMJ.
How can you tell if a person is suffering from TMJ dysfunction?
The listed symptoms are a clear sign that something is wrong with the joint and require mandatory comprehensive treatment. Even in the early stages of the development of the disease, a person does not feel any deviation from the norm, his jaw begins to behave differently, and the pain in the mouth intensifies over time.
To confirm the diagnosis, the dentist must:
- carry out a visual examination of the teeth and oral cavity as a whole;
- collect anamnesis and study the patient’s complaints;
- perform an ocludogram to study the position of the jaws in relation to each other;
- refer the person for orthopantomography, x-ray and computed tomography of the TMJ. An MRI may be needed to monitor and correct treatment.
In some cases, additional consultation with related specialists is required: neurologist, rheumatologist, ENT specialist, etc.
Based on the diagnostic procedures performed, the patient is diagnosed and step-by-step treatment is prescribed.
It is important! To effectively treat the disease, you need to contact an experienced dentist, who will not only diagnose the condition of the oral cavity, but will be able to distinguish a violation of the structure and functions of the TMJ from other pathologies. For example, from jaw dislocation, articular arthrosis, complex diseases, arthritis, synovitis, etc.
Diagnostics
In order to make a diagnosis, the doctor conducts an examination according to the following scheme:
- Questioning the patient. Of interest to the specialist are complaints, conditions for the appearance of unpleasant symptoms, duration of the disease, previous treatment and its effectiveness.
- External examination and palpation. The gnathologist examines the patient’s face, paying attention to the area where the TMJ is located. By feeling the joints, you can get an idea of its structure and the state of its tissues.
- Dental examination. Anomalies of occlusion and the degree of their severity are identified.
- X-ray examination. The photographs show the bone formations that form the joint. By their relative position one can determine the presence of dislocations and subluxations, and by the thickness of the joint space one can judge the condition of the cartilaginous disc.
Types of treatment for TMJ dysfunction
The basis of treatment for problems with TMJ is to find the cause of the current pathological condition. If this is the absence of chewing teeth, then it is necessary to perform implantation and prosthetics. If the cause is muscle tension, neurological treatment, etc. is necessary.
Common tactics for treating TMJ dysfunction involve the following ways:
- Drug therapy to eliminate pain. At this stage, the patient may be recommended to take a course of muscle relaxants, antidepressants, or glucocorticosteroid drugs. It is possible that during the treatment process, injections of botulinum toxin into the jaw projection will be necessary to reduce muscle spasm and alleviate the patient’s general condition.
- To functionally relax the jaw muscles, a course of psychotherapeutic assistance may be necessary. Physiotherapeutic procedures in the joint projection are also relevant, including electrophoresis, laser therapy, ultrasound, etc. Also at this stage of treatment, special relaxation exercises are recommended to control the condition of the muscles.
- Orthodontic care. This involves correcting the bite using braces or aligners. In some clinical cases, the patient is recommended to wear mouth guards, splints, orthodontic plates, etc. Wearing a special orthodontic bite splint will reduce the adverse effect of teeth grinding. Repeated prosthetics, implantation or filling of teeth may be necessary.
- Surgery is indicated in the absence of the desired effect in the case of using the above treatment methods, including after wearing orthodontic appliances. At this stage, myotomy of the pterygoid muscle, arthroplasty, and condylotomy of the head of the mandible can be performed.
Pain syndrome and restrictions in movements of the lower jaw
Before
Frontal photograph of the bite
Lateral photograph of the bite (right). Absence of tooth 4.5, absence of tooth 1.4 are noted with replacement of the defect with a removable partial apparatus
Lateral bite photograph (left)
MRI slice of the left TMJ. There is a structural change in the shape of the joint head. Anterior disc dislocation without reduction (without restoration)
After
Frontal photograph of occlusion after joint surgery
Lateral bite photograph (right)
Lateral photograph of the bite (left). There is a rise in the height of the bite on the operated side
MRI section of the left TMJ after surgical reduction of the articular disc. The correct position of the disc is noted
Frontal photograph of the bite in the mouthguard (Splint)
Lateral photograph of the bite in the mouth guard (Splint) (right view)
Lateral photograph of the bite in the mouthguard (Splint) (left view)
Specialists:
Nazaryan David Nazaretovich
Description:
A typical complaint for patients with TMJ problems is pain and restrictions in the movements of the lower jaw. Such complaints were also present in this clinical case. The entry MRI of the TMJ shows a pronounced structural change in the shape of the head of the left joint and an articular disc displaced forward without the ability to restore its position.
We carried out preliminary Splint therapy in preparation for joint surgery (we made a transparent rigid mouthguard for the lower dentition) and assessed the result over time with a series of control MRIs of the TMJ. Using the example of a section from one of these studies, one can clearly compare the picture before and after surgery. The patient also noted positive dynamics regarding pain symptoms already at the stage of wearing a mouth guard. In the postoperative period, pain was no longer observed. The range of movements of the lower jaw was restored. Of course, the closure of the teeth changed after placing the disc in the correct position. We will require orthodontic and orthopedic treatment to support the stability of the TMJ.
Splint therapy with an occlusal splint for the treatment of TMJ dysfunction
This type of dental treatment is a preparation for further correction of the bite with a brace system.
At this stage, a splint splint or a so-called occlusal splint is placed in the patient’s oral cavity, which is fitted by a specialist. It is made individually for each person. The plastic splint is designed to reprogram the muscles, after which the resulting position of the jaws is stabilized by a brace system.
Features of splint treatment:
- along with the gradual correction of the position of the jaws, the splint splint gradually wears off;
- recommended for constant wear (both day and night);
- It’s comfortable to talk to her, you just need to get used to her;
- as the splint corrects the position of the joint itself and the work of the masticatory muscles, the person does not experience pain or discomfort;
- caring for the splint during treatment is extremely simple - it is removed only when brushing your teeth, washed with warm water and toothpaste or soap;
- Putting on the splint is very simple and quick.
In some cases, wearing a so-called TMJ mouth guard is prescribed.
Quite often, TMJ dysfunction is treated through systematic orthodontic expansion of the upper jaw. As a result of this treatment, the width of the upper row of teeth is normalized, not only articular pathology goes away, but also the face becomes symmetrical and more harmonious.
The result of treatment with a splint or other orthodontic systems should be an ideal position (occlusion) of the jaws with correct fissure contacts. After wearing splints, prosthetics or artistic restoration are usually recommended as the final aesthetic stage of treatment.
Ankylosis of the TMJ appears:
- after a joint injury;
- after a long period of immobility, for example, being in a cast;
- due to inflammation or purulent process;
- as a consequence of arthritis.
When a joint fusions, as a result of the destruction of the articular cartilage, a bone growth appears near it, due to which the joints are connected and become immobile. Ankylosis is accompanied by breathing problems, tongue retraction, sleep apnea, snoring, and due to periodic lack of hygiene, tartar forms. This leads to tooth decay and other oral diseases. Ankylosis of the TMJ is eliminated with a surgeon’s scalpel.
The process of fusion of articular surfaces occurs gradually - as a result of violation of the integrity of the articular cartilage, the cavity around it is overgrown with connective bone tissue (growth), which ultimately leads to complete fusion and pathological changes in the joints, creating their immobility. Treatment of ankylosis of the temporomandibular joint is performed surgically.
Surgical treatment of TMJ dysfunction
Surgical treatment of TMJ dysfunction involves endoprosthetics or arthroscopy.
Arthroscopic surgery involves the use of a thin tube with a video camera at the end. With its help, it is possible to visualize the condition of the patient’s joint and monitor the progress of the operation. During arthroscopy, the surgeon removes adhesions, can correct the position of the jaw disc, and apply targeted pressure to areas of inflammation. The dentist also thoroughly rinses the jaw joint with antiseptic compounds to disinfect the area of inflammation. Anti-inflammatory drugs are administered. Thus, the blocking of movements is removed, the characteristic clicks go away, and the patient’s condition gradually normalizes.
As one of the options for solving the problem, a dental surgeon may recommend endoprosthetics. We are talking about replacing parts of the joint with implants. For example, a carbon fiber endoprosthesis is often installed.
During arthrocentesis, the surgeon cleans the joint by piercing it with a special needle, passing a sterile fluid through the joint cavity.
Arthroplasty involves realigning the joint.
Prevention of TMJ dysfunction
What to do to prevent the primary or secondary development of joint dysfunction?
- Have regular dental checkups (at least twice a year);
- take care of your teeth and oral cavity;
- reduce excess loads;
- do not expose the body to stress and anxiety;
- treat caries, pulpitis and gum diseases in a timely manner;
- wear orthodontic systems when indicated for bite correction;
- perform implantation and installation of dentures by experienced doctors;
- correct orthopedic problems in a timely manner;
- treat factors that increase the risk of joint dysfunction (bruxism, neurological diseases, etc.).
First aid
A joint dislocation or subluxation that occurs for the first time can cause severe pain. Joint dysfunction can also cause pain of the same intensity. Regardless of the cause of the discomfort, you must do the following:
- provide rest to the joint: do not eat, talk as little as possible;
- take a pain reliever;
- Consult a doctor as soon as possible and undergo the necessary examination.
Experts categorically do not recommend heating a sore joint if the cause of the pain is unknown. In case of dysfunction, heat exposure can lead to some relief of the condition, but in case of dislocation, on the contrary, it will cause harm. Under the influence of heat, blood flow to the tissue increases, which contributes to the development of edema and makes reduction difficult. Thus, when trying to help yourself or a loved one, you can unknowingly cause serious harm.
Prognosis for the treatment of TMJ dysfunction
Treatment of TMJ dysfunction cannot be delayed. The disease will not go away on its own! It can smoothly flow into further destructive processes, “resulting” in arthrosis of the jaw joint and other serious consequences. If nothing is done, ankylosis of the joint may occur, that is, its complete immobilization, and the person ceases to “own” his jaw.
At the same time, comprehensive treatment of the problem with strict medical supervision provides positive prospects for development and complete recovery.
Bone ankylosis
With bony ankylosis of the TMJ, there is a connection between the condylar process and the zygomatic arch. It turns out that bone tissue fills the joint cavity. Bone ankylosis of the TMJ can be partial or complete, depending on whether there are intact areas on the surface of the joints. If the disease affects only one joint, the face becomes asymmetrical. When two joints are affected, the upper jaw moves forward, the chin region falls, which leads to malocclusion and problems with teeth, speech and breathing. A person with this condition will have difficulty eating solid food. The full form is characterized by the fact that the joint space is not visible on the x-ray, and the condylar process appears wider than it should.