Clinical picture
The development of osteoarthritis of the TMJ begins in patients with degeneration of intra-articular cartilage tissue. As the pathology becomes more complex, it spreads to bone tissue. Dystrophy leads to severe thinning of cartilage tissue and a decrease in its performance.
After complete destruction of cartilage, the disease spreads to hard tissues, which is due to their constant friction. As a rule, the destruction of soft and hard tissues is chronic. Pathological changes lead to increased mobility of the TMJ, and osteoarthritis becomes more pronounced.
General symptoms:
- uncharacteristic noises and crunching sounds;
- aching or dull pain, aggravated by jaw movements;
- decreased joint mobility;
- spread of pain to the peritemporal tissues;
- difficulty eating due to deformities of the affected joint;
- facial asymmetry associated with swelling and inflammation (observed in advanced cases).
Patients often do not realize the seriousness of the consequences, feeling minor discomfort in the TMJ area and consult a doctor with complaints of stiffness and severe pain. It is the lack of timely treatment that leads to the destruction of cartilage tissue.
Treatment of TMJ osteoarthritis
The main task of the doctor in the treatment of this disease is to eliminate the symptoms and achieve a state of the joint in which it can adapt to the load acting on it. The treatment plan, as a rule, depends more on clinical symptoms than on X-ray data. It is recommended to resort to surgical intervention only after confirmation of the ineffectiveness of the main therapy. According to numerous studies, the prognosis after primary treatment is almost always satisfactory. Even despite the persistence of radiological signs of damage to the bone structures of the joint, clinically the condition often improves. After this, proper further management and observation of the patient is very important to stabilize the joint.
In general, treatment should be aimed at restoring protective mechanisms: sufficient blood supply, mobility in the joint, shock-absorbing properties, to ensure the ability of the TMJ to adapt. If necessary, therapy should be carried out aimed at reducing the load on the joint and increasing mobility in it, while eliminating pain and inflammation. Of course, patients who are at systemic risk should receive appropriate treatment under strict supervision.
Already at the stage of diagnosing osteoarthritis, one should try to identify the dominant risk factor. High load on the TMJ is caused by:
- clenching teeth,
- unfavorable changes in occlusion (loss of chewing teeth, premature occlusal contacts and bad habits).
Dental factors must be eliminated during treatment or minimized using occlusal trays and selective grinding. At the same time, it is recommended to switch the patient to soft food and help him get rid of bad habits.
To eliminate inflammation, medications (for example, nonsteroidal anti-inflammatory drugs) are used, which are prescribed orally, intramuscularly, or injected directly into the intraarticular space. Also, to reduce pain and inflammation, it is advisable to carry out physical therapy without stress on the TMJ. Exposure to heat and various compresses can effectively eliminate pain in order to continue to perform physiotherapeutic exercises aimed at strengthening the masticatory muscles, reducing joint contracture and maintaining a normal range of motion in the joint.
In general, treatment should be aimed at restoring mobility in the affected joint, which is an essential condition for complete rehabilitation.
Causes
Risk factors for developing osteoarthritis:
- people aged 40-60 years;
- injuries;
- bite defects;
- partial or complete loss of teeth;
- genetic predisposition;
- infectious processes of the ears.
It is difficult to determine the exact cause of the development of the disease, since the cause may be minor injuries that are left unattended.
Pathology can occur in adolescents with rapid growth, which is associated with anatomical features and accelerated growth of bone tissue against the background of underdevelopment of cartilage and muscles. Joint deformity can be diagnosed due to a lack of vitamins and an improper diet. If the body does not receive sufficient trace elements, this leads to deterioration of the cartilage.
Intense load on weakened temporomandibular muscles entails various microtraumas, the consequences of which are difficult to predict.
Non-surgical treatment of TMD
Nonsurgical treatments for painful and dysfunctional TMD include patient education, joint stress reduction, medications, and physical therapy. Of course, the patient cannot control nighttime chewing activity, which is precisely the main source of excess load on the TMJ. To control this activity and reduce the load on the joint, various occlusal devices (for example, mouthguards) are used. According to research, they can reduce the load on the TMJ when clenching teeth in 82% of patients. During the daytime, the load on the joint is reduced by increasing the patient’s attention to his condition, switching to soft foods, and taking anti-inflammatory painkillers. A physical therapist can teach the patient specific exercises to increase mobility in the TMJ and relieve pain and stress on the joint.
Treatment
Effective treatment of TMJ osteoarthritis requires an integrated approach.
In particular:
- taking medications;
- physiotherapeutic procedures to relieve symptoms.
Drug treatment
- The patient is prescribed non-steroidal drugs and anti-inflammatory drugs. In case of serious violations, the treatment protocol includes chondoprotectors that have a restorative effect.
- To relieve acute pain, potent analgesics are prescribed in various forms.
- In combination, the patient is recommended to install orthopedic structures (braces, mouth guards).
- It is recommended to limit your intake of solid foods.
Physiotherapeutic manipulations
- Ultrasound procedures.
- Laser therapy.
- Impact of dynamic currents.
- Electrophoresis.
- Microwave.
Surgery
If conservative methods do not bring the expected result, the patient is prescribed surgery. As a rule, surgical elimination of the problem is indicated only in complex cases when strong medications are ineffective. The operation is performed as an emergency if there is a purulent focus in the joint.
Instead of a conclusion
Statistics show that every third resident of the country has one or another joint pathology. Limitation of motor functions can lead to general complications, such as disruption of the metabolic and endocrine systems, hernias, limited mobility, etc. The earlier treatment is started, the higher the likelihood of recovery.
After successful treatment, a period of remission begins. The patient needs to remember that TMJ osteoarthritis is a chronic disease, so after the therapeutic course it is important to follow a diet and listen to the state of the body. Even minor infections can cause an exacerbation of the disease.
Treatment of degenerative-dystrophic diseases of the temporomandibular joint
Functional disorders of the temporomandibular joint (TMJ) are the result of a combination of a number of unfavorable factors that can reinforce each other. These may be dentofacial anomalies and deformations of the dentition, dysfunction of the masticatory apparatus and nearby anatomical structures, infectious diseases, psychogenic disorders, traumatic injuries, somatic pathology (connective tissue diseases, spinal diseases, etc.) (Persin L. S., 1996; Ivanichev G. A., 1997; Stohler C., Zarb G., 1999; Lund JP, 2001; Drobyshev A. Yu., 2010; Shipika D. V., 2012). TMJ disorders are a common phenomenon that occupies one of the leading places in dental practice with an incidence rate of 20 to 70% among those examined according to various authors. The incidence of TMJ diseases in men and women is different and is 1:4 (Kleinrok J., 2004; Smaglyuk L.V., Trofimenko M.V., 2005; Shibinsky V.Ya., 2009; Babov E.D. et al. , 2011; Shalender Sharma et al., 2011).
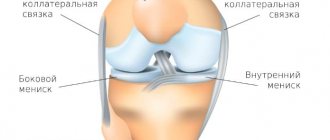
In the treatment of TMJ diseases, preference is given to traditional conservative methods (medication and physiotherapy of the affected joint, occlusal splints, selective grinding of non-supporting cusps of teeth, electrical neurostimulation of masticatory muscles, psychological support, diet), which often, even in combination, can be ineffective. Therefore, minimally invasive surgical techniques are used, such as arthrocentesis with lavage of the articular cavity and joint arthroscopy for changes in the position of the articular disc, capsular-ligamentous apparatus, synovial fluid composition, etc. (Nishimura M., et al., 2006; McCain, Undt G., 2008; Murakami KI et al., 2008; Nitzan DW, 2011; Mirella M. Nascimento et al., 2013).
Purpose of the work: to investigate the effectiveness of arthrocentesis in the complex treatment of degenerative-dystrophic diseases of the TMJ.
Materials and research methods
The clinical part of the study included examination of 222 patients (m - 39, female - 183) with TMJ diseases; the average age of the patients was 26 years.
161 patients were diagnosed with osteoarthritis (131 cases) and arthrosis deformans (30 cases). All patients were treated at the Dental Medical Center of the National Medical University named after A. A. Bogomolets at the Department of Surgical Dentistry and Maxillofacial Surgery. Patients complained of moderate pain localized in the TMJ, which occurred with prolonged chewing or eating solid food or prolonged conversation, and also indicated a crunching sensation in the TMJ, limited mouth opening, morning stiffness in the TMJ, and a block in the joint. Laboratory, radiological and functional methods were used to study TMJ diseases. Orthopantomography was performed to evaluate the structures of the condylar processes of the mandible, radiography of the TMJ with an open mouth according to Parma, computed or magnetic resonance imaging (MRI). If there were noises in the TMJ, a mandatory MRI examination was performed with the mouth closed and open.
From the life history of the patients, the following most common somatic diseases were revealed: chronic gastritis (34%), chronic gastroduodenitis (21%), chronic cholecystitis (60%), bile duct dyskinesia (29%), duodenal ulcer (12%), chronic pancreatitis (7%), reactive pancreatitis (6%), chronic cystitis (15%), urolithiasis (5%), mitral valve prolapse (19%), unilateral nephroptosis (14%), chronic tonsillitis (50%), disorder vision (51%). Patients noted periodic pain in the knee and ankle joints, and dislocations in the ankle joint (8%). In childhood there were acute respiratory diseases with a frequency of 3-4 times a year, chronic tonsillitis (51%) in the acute stage, acute purulent or chronic otitis.
It was found that 19% of patients received treatment before contacting the department. They were prescribed non-steroidal anti-inflammatory drugs, analgesics and physiotherapeutic treatment methods (UHF, microwave, electrophoresis with potassium iodide solution, calcium chloride). The treatment received did not produce a positive effect; the pain syndrome decreased in intensity, but remained.
We prescribed chondroprotectors to the patients, as well as drugs that improve tissue microcirculation, IV generation vitamin D and Ca preparations (Calcium D3 Nycomed, Kalcemin, Vitrum Calcium), antioxidant therapy, and magnetotherapy with a constant magnetic field with magnetic induction 240 mTl.
10 (4.5%) patients underwent arthrocentesis according to the Nitzan DW method (1991) [4], 6 patients had osteoarthritis of the TMJ in the initial stage, 3 patients had internal disorders of the TMJ (stage I-II according to the Wilkes classification, 1990) [8, 9], one clinical case was an acute TMJ block (“acute TMJ block”).
In order to block the peripheral branch of n. auriculotemporalis performed local anesthesia with sedation. The needle puncture points were determined along the trago-orbital line (Holmlund-Hellsing line). According to the topographic-anatomical features of the structure of the TMJ, the first point (point A) was found 10 mm in front and 2 mm down from the tragus of the ear, which corresponds to the anatomical projection of the articular fossa, the direction of the needle was upward, medial and forward at an angle of 45° to the trago-canthal lines. Point B was determined 20 mm forward from the tragus of the ear and 5 mm down from the drawn line, which corresponds to the anatomical projection of the articular tubercle for insertion of the second needle, the direction of which was upward, medial and posterior.
The upper space of the articular cavity was insufflated with physiological solution in an amount of 2-3 ml.
A syringe with a volume of 10 cm3 with a needle with a diameter of 18 mm was used, the total amount of injected solution was 250 ml. Immediately after lavage, passive movements of the patient’s lower jaw were carried out: the thumb of one hand was on the extreme lower molar on the side of the pathologically changed joint, the remaining 4 fingers of this hand covered the lower jaw in the body area; at the same time, the other hand, located at the temporal region on the same side, fixed the head.
The duration of arthrocentesis was 15-20 minutes.
After lavage, one patient was injected into the joint cavity with a hyaluronic acid preparation with a molecular weight of 3 MDa (Hialual) 1 ml for 1 week (course of treatment - 5 injections), 3 patients were injected with a complex homeopathic chondroprotective drug (Tsel T), 6 patients were injected into the joint cavity no drugs were administered to the joint. The patients were given stabilizing splints and prescribed antibacterial, anti-inflammatory, restorative therapy with individual recommendations to follow a gentle regimen and diet, as well as use the splint.
Repeated examinations of patients were carried out the next day after arthrocentesis, on the 7th day, and then after 1, 3, 6, 9, 12 months with assessment of the following parameters: the distance of mouth opening between the cutting edges of the incisors, the symmetry of movements of the heads of the lower jaw, arthralgia ( quantitative characteristics of pain: determined using a visual analogue scale (VAS) and the ability to chew fully [12].
results
The X-ray picture of the TMJ in the examined patients was characterized by uneven narrowing of the joint space, disruption of the structure of the bone tissue of the condylar process, in some cases the head was somewhat flattened [11]. Patients with TMJ murmurs had partial anterior disc displacement.
After arthrocentesis, there was an improvement in the TMJ condition on days 2-3. The patients had no complaints, the postoperative period was without complications. In a patient with an acute block of the TMJ, the movements of the lower jaw were restored immediately after lavage, the maximum opening of the mouth the next day was 30 mm, on the 4th day the movements of the lower jaw were painless and without restrictions, the maximum volume of mouth opening was 40 mm. The patients had complete chewing of food and no pain occurred. In the postoperative period, VAS was equal to 1, and after 1 month, VAS was equal to 0.
Discussion
Lavage of the upper floor of the articular cavity reduces the manifestations of pain due to the washing away of inflammatory substances (catabolism products, inflammatory mediators (arachidonic acid, cytokines) and tissue detritus) (Quinn, Bazan, 1990), the excursion of the lower jaw increases, and the phenomena of intra-articular adhesions decrease (Spallacia et al., 2000), negative pressure and blocking phenomena are eliminated during an acute block in the TMJ, but the articular disc does not move to the correct position (Moses et al., 1989; Nitzan, Florencio Monje-Gil et al., 1991, 2012) .
Taking into account the presence of a pathological process in the TMJ, confirmed clinically and x-ray, as well as on the basis of pathological changes in the tissues of the joint and the lack of positive dynamics after conservative treatment, lavage of the articular cavity was performed.
According to the literature, the effectiveness of arthrocentesis ranges from 70-75% (Murakami KI et al., Fridrich KL et al.) to 95-98% (Nitzan DW et al., Dimitroulis G. et al.). Using arthrocentesis in patients with degenerative-dystrophic changes in the TMJ and acute block, we obtained a 100% treatment result and positive postoperative dynamics of restoration of TMJ function.
The introduction of medications into the joint cavity has many supporters and opponents. According to the literature, intra-articular administration of corticosteroids is used for inflammatory processes, but in many cases local side effects occur - necrotic changes in cartilage tissue (Dimitroulis G, Dolwick MF., 1996). Undt G., Muracami KI (2005) and others do not support the point of view on the advisability of introducing hyaluronic acid into the joint cavity after arthrocentesis [7].
However, hyaluronic acid provides shock-absorbing and lubrication (lubricating) functions, is a substrate for the synthesis of proteoglycans, protects pain receptors of the synovial membrane from irritation, improves the properties of synovial fluid, and facilitates the penetration of nutrients that are necessary for the construction of the cartilage matrix in the TMJ [5]. The hyaluronic acid preparation (“Hialual”) is a combined preparation that contains unstabilized acid and succinate.
The complex homeopathic preparation (“Tsel T”) has a chondroprotective effect, affects the primary link of the degenerative process, stimulates the regeneration of cartilage and bone tissue, increasing local mitotic activity [6].
Both drugs showed positive dynamics and effect and were included in the treatment algorithm for our patients [5]. Thus, the use of irrigation fluid (saline solution, Ringer’s solution) eliminates symptomatic phenomena in the patient, and the task of medicinal intra-articular support was to influence the result of the pathological process, restore the function of the TMJ and the structure of its tissues [3] in patients who did not have a positive conservative result treatment of degenerative-dystrophic changes in the TMJ.
conclusions
Arthrocentesis is a minimally invasive manipulation that can be performed on an outpatient basis under local anesthesia and sedation, which can be used in cases of ineffective conservative treatment and the advisability of surgical intervention on the affected structures of the TMJ without or with the use of chondroprotective drugs.
LITERATURE
- Khvatova V. A. Clinical gnathology. M.: Medicine, 2005. - P. 296.
- Bezrukov V. M., Semkin V. A., Grigoryants L. A., Rabukhina N. A. Diseases of the temporomandibular joint. - M.: GEOTAR-MED, 2002. - P. 48.
A complete list of references is in the editorial office.
Features of treatment
| Click to sign up for a FREE consultation |
Treatment is complex, it requires taking medications and prescribing physiotherapeutic procedures that are aimed at eliminating symptoms. In addition, non-steroidal anti-inflammatory drugs and a course of treatment with chondroprotectors are prescribed to restore damaged tissue. The patient may be prescribed painkillers in the form of ointments, tablets or gels, and in some cases it is necessary to wear special mouth guards. For the entire duration of treatment, the patient must follow a diet, eat only soft foods, including mousses and pureed vegetables.
Physiotherapy includes such effective measures as ultrasound, microwave therapy, electrophoresis, laser therapy, and the use of dynamic currents. If traditional therapy has no results, surgical treatment will be prescribed; most often, such measures are necessary in case of a severe inflammatory process, which is accompanied by the accumulation of purulent masses.
Treatment of TMJ diseases:
Treatment is prescribed depending on the examination results. When treating a joint, the following is used:
- drug therapy
- physiotherapy
- myogymnastics (muscle gymnastics)
- splint therapy
Splin therapy is one of the most effective methods of treating musculo-articular dysfunction of the TMJ. An individual mouthguard is made for the patient, which helps to relax the masticatory muscles, set the joint in the correct position, thereby eliminating the cause of musculo-articular dysfunction of the TMJ.
The article was prepared by Kurakova A.S., orthodontist.
Symptoms
The absence of pronounced symptoms in the early stages is due to the latent course of the disease. Osteoarthritis gradually destroys the structure of cartilage tissue, the task of which is to maintain the gap between the bone elements of the jaw apparatus. Complete destruction leads to further spread of the dystrophic process, which results in:
- Aching pain syndrome caused by tissue inflammation;
- Extraneous sounds that occur when making movements of the lower jaw;
- Gradual decrease in the range of motion of the joint;
- Painful sensations radiating from the temporal lobes;
- Gradual loss of facial symmetry and problems with eating.
Unfortunately, in the early stages, most patients do not attach importance to mild discomfort, associating it with other factors. The result of untimely consultation with a doctor is the progression of pathology, which makes the treatment of osteoarthritis of the temporomandibular joint much more difficult.
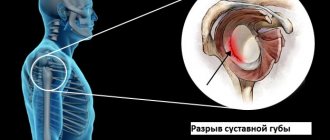
Indications for surgery for osteoarthritis
The most common indication is severe pain and/or dysfunction of the TMJ of articular origin, which is aggravated by activity of the lower jaw. The more severe the pain and dysfunction, the better the prognosis for surgical intervention. The lack of effectiveness of arthrocentesis (sampling fluid from the joint) also became an indication for further surgical treatment. This low effectiveness of the procedure is explained by adhesions, which, in the absence of bone deformation, are not visible on an x-ray.
Surgical treatment of TMD
Surgical intervention in the treatment of TMD does not play a major, but very important role. Surgery is indicated for approximately 5% of patients suffering from TMD. Moreover, the range of surgical interventions is very wide. Despite the many supporters of each individual surgical method, there are currently no strict clinical data substantiating the indications for a specific operation in a specific clinical case. Therefore, when deciding on any surgical intervention, the doctor uses criteria to assess the stability of the patient's condition.
Diagnosis of TMJ arthrosis
A disease such as TMJ arthrosis has been well studied and also has clear rules and diagnostic methods necessary for further treatment. The basis of diagnosis lies in the data obtained as a result of a medical examination. Also in diagnosis, an external examination of the patient by palpation of the affected side plays a significant role. The full picture of the disease is revealed by the results of tests and instrumental examinations. To treat arthrosis of the TMJ and establish a diagnosis, you must consult a dentist. It is during the dental examination that any dental anomalies (bad bite) are detected and the general condition of the teeth and dentures is assessed. The main indicator of TMJ arthrosis during a dental examination is traces of pathological abrasion of tooth enamel.
After a preliminary examination, the dentist prescribes an x-ray examination. It is based on its data that the nature of the pathological process of the joint will be established. The presence of stage 1 TMJ arthrosis in a patient is indicated by a slight narrowing of the joint space, and the disease is also indicated by the growth of bone osteophytes. The second stage is diagnosed by indicators such as osteosclerosis, destruction of cartilage tissue.
In the second and third stages of arthrosis of the TMJ, an X-ray image of the patient indicates a clear deformation of the bone and a decrease in the ligamentous apparatus, and contracture is formed. Additional diagnostic methods include computed tomography and blood tests, which are necessary to identify the inflammatory process.
Causes of TMJ arthrosis
The causes of TMJ arthrosis are usually divided into two categories:
- of a local nature - a long-term course of an inflammatory process in the body, in particular in the joint itself, increased loads on the head of the joint, which are present in diseases such as bruxism, in case of dental anomalies, when their absence is observed, in case of impaired occlusion between the jaws;
- of a general nature - dysfunction of various body systems (for example, endocrine or metabolic), the presence of infectious diseases.
Most often, arthrosis of the TMJ appears due to the complex presence of causes of one and two types. In this regard, the presence of bruxism in a patient, which is characterized by “grinding” of teeth along with pathological abrasion, leads to the absence of normal occlusion, which disrupts the functioning of the jaw joint and contributes to the development of arthrosis of the TMJ.
The main reason for the progression of dystrophic processes is a disruption of the process of cellular and extracellular nutrition. As a result of such dysfunction, dystrophy of the cartilage covering the head of the condylar process develops; the head itself gradually changes and takes on the shape of a hook or pin.