Many of our patients (as well as patients, for example, of chiropractors or neurologists) do not even realize how interconnected the problems they are being treated with are. For example, the jaw joint hurts, the head hurts, shooting in the ear, clicking in the jaw, pulling at the base of the skull... it would seem that these are different symptoms, but the reason may be the same for everyone: TMJ dysfunction
.
Functions of the TMJ
TMJ
or
temporomandibular joint
is a joint located above the ear that connects the temporal bone to the lower jaw and the lower jaw to the skull. The muscles that are attached to this joint are actively involved in speaking, facial expressions, chewing, and swallowing. Together, muscles, ligaments, cartilage and joints make up the apparatus, thanks to which we can generally open and close our mouth, move our jaw back and forth and left and right, and the load on this apparatus is significant - comparable to the load, for example, on the knee joint.
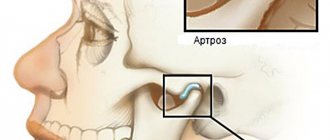
The temporomandibular joint is the only paired and symmetrically moving joint in the human body, and problems with its functioning lead to numerous unpleasant diseases. TMJ dysfunction—limited work and mobility of the jaw joint—occurs when the joint on the right and left sides of the skull does not move synchronously or evenly. For example, to open the mouth, the patient must first move the lower jaw from side to side, “until it clicks.” Or when you open your mouth, you feel pain in your jaw or temples.
This disease has many names: arthritis (arthrosis) of the TMJ, myofacial syndrome, myoarthropathy of the TMJ, chronic dislocation of the lower jaw, Costen's syndrome (named after the American doctor who first identified this disease). This pathology is difficult to diagnose and treat, and at the same time it can cause a wide variety of pain - from headaches to neck pain.
Statistical fact: from 30% to 70% of dental patients suffer from functional pathology of the temporomandibular joint. And these are not always older people, as one might expect. On the contrary, people of all ages, including children, suffer from TMJ pain and related pain.
TMJ dysfunction was first described by otolaryngologist (ENT doctor) Kosten in 1934. Kosten studied pain and noise in the ears and burning in the nose, which intensified during or after eating, and was the first to think of linking them with malfunction of the temporomandibular joint. Subsequently, his colleagues and other doctors who examined this problem expanded and supplemented the list of symptoms. Now this list is quite extensive, and often not all symptoms can be associated specifically with TMJ problems.
Diagnostics
Diagnosing TMJ disorders first involves taking a medical history, followed by a physical examination. The doctor applies light pressure on the side of the face where there is discomfort, on the masticatory muscle fibers. At the same time, the patient closes and opens his mouth. Popping or clicking sounds and jaw thrusting are analyzed. If indicated, an MRI may be prescribed. The procedure will show whether there are internal problems with the joint. If osteoarthritis is suspected, x-rays and CT scans can confirm the diagnosis.
Pain in the jaw joint when chewing and opening the mouth often occurs with infectious arthritis. Diagnosis is made by inserting a needle into the joint itself to collect fluid. This research method is called aspiration. The liquid is analyzed for the presence of pathogenic bacteria. Hypermobility and ankylosis are determined by the width of the mouth opening. Sometimes the patient is referred for polysomnography to determine sleep disorders. An orthopantomogram of the jaw plays an important role in the research process.
Symptoms of TMJ dysfunction
- Pain in the jaw, increasing when opening the mouth, chewing, speaking, yawning;
Clicking in the joint of the lower jaw, the jaw “jams”, it does not open, does not close, or has begun to close differently;- Pain in the temples, in the eye area, visual impairment, photophobia (sensitivity to light);
- Pain, ringing and noise in the ears, in the ear area, feeling of pressure in the ears;
- Frequent headaches, dizziness, migraines;
- Sleep disorders, insomnia, anxiety, depression;
- Pain in the neck, in the lower part of the skull;
- Tooth pain from sweets, hot, cold.
This diversity in symptoms, which often makes it difficult for doctors to diagnose, is explained by the fact that the joint is connected to many important organs and parts of the body (eyes, ears, neck, head) and errors in its functioning can affect everything at once, or they can only affect something one. It is usually possible to determine that the problem is in the temporomandibular joint only in a complex manner.
In most cases, TMJ dysfunction is manifested by pain in the face, joints of the jaw, neck, shoulders, ears, crunching and clicking. Complaints of dizziness, difficulty chewing food, speech and hearing disorders, difficulty opening the mouth, “jamming” of the jaw, or even the appearance of swelling and fever are also common.
Which doctor should I go to?
In order to properly treat pain in the jaw joint when opening the mouth, it is necessary to develop an optimal treatment regimen. This can be done by a professional orthodontist.
- If the patient needs to have braces, plates, dentures, or implants installed, impressions of the teeth are taken. Complex therapy for TMJ gives good results.
- In serious cases, surgical technologies are used - bone and muscle grafting. The pathology cannot be neglected so that it does not develop into arthrosis with the proliferation of connective tissue and subsequent immobilization of the joint. It is important to eliminate the root cause of the disease.
- Severe spasms and discomfort are relieved with compresses.
- For stress that leads to tension, the patient is prescribed sedatives.
- Sometimes splinting is required.
- The patient may be recommended physical therapy.
- Patients may be prescribed nonsteroidal drugs, muscle relaxants, and sedatives.
Therapy also includes eliminating defects in the masticatory organs, grinding fillings, correcting prosthetic errors, replacing structures, and correcting bites. The load on the joint must be reduced. To do this, you should include soft foods in your diet, perform relaxation exercises and massage complexes. Ultrasound and laser therapy may be required. It is easier to eliminate the disease at the initial stage so that it does not become chronic. Timely visits to the doctor, correction of posture, elimination of stressful situations, replacement of lost units are effective preventive measures.
Pain in the jaw joint: causes
- Defects in the dentition - lack of teeth, overestimation of fillings;
Pathological abrasion of teeth;- Broken bite
;
- Overload of the masticatory muscles (for example, if you chew on only one side for a long time);
- Inaccurate prosthetics, errors in orthodontic treatment;
- Other anomalies of the oral cavity and jaw structure;
- Bruxism, involuntary grinding of teeth.
- Birth trauma, trauma to the skull and jaw;
- Osteochondrosis and scoliosis of the spine;
- Severe constant stress
;
- An infection in the joint cavity that provokes inflammation of the TMJ.
Possible causes of pain
Most often, the joints of the jaw hurt because the muscle fibers are strained and anatomical changes occur in the joint unit. The situation is aggravated by psychological reasons, sleep disorders, and emotional stress. In addition, provoking factors include:
- Bruxism, that is, grinding of crowns;
- Osteopenic disorders of the body;
- Genetic bone pathologies;
- The jaw joint near the ear hurts when an infection develops, the patient has suffered a neck or head injury;
- Muscle pain, internal disorders, tension;
- Ankylosis, arthritis, excessive mobility;
- Lack of chewing organs, unprofessional orthodontic treatment;
- Active conversation load;
- Pain in the jaw joint and radiates to the ear in patients with the habit of biting nails or placing the smartphone close to the hearing organ;
- Problems of the central nervous system, scoliosis and osteochondrosis of the spine;
- Pathologies of the endocrine system;
In addition, dysfunction occurs with asynchronous movements of the joints on both sides.
Diagnostics and x-ray of the temporomandibular joint
Diagnosis of TMJ when it is dysfunctional is difficult due to the variety of clinical complaints. This leads to the fact that the patient can undergo examination by different specialists for a long time, wasting time. A full examination is carried out by dentists
(primarily an orthopedist or orthodontist) and neurologists.
Diagnosis with the naked eye is difficult, and TMJ problems can only be directly noticed if the malocclusion is clearly visible. Most often, dysfunction of the temporomandibular joint is associated precisely with disorders of bite and jaw closure.
The most reliable and effective way is to conduct x-ray diagnostics and orthopantomogram
jaws. In some cases, an MRI may also be done.
Causes of temporomandibular joint dysfunction
Scientists believe that TMJ dysfunction develops under the influence of many factors. The temporomandibular joint is one of the “target organs” that respond to factors of aggression of various origins. They can be local and systemic. Local factors include acute and chronic joint injury, lack of chewing teeth, bruxism (grinding teeth in sleep). TMJ pain dysfunction syndrome can develop under the influence of stress, anxiety, tension and other emotional factors.
Currently, there are two main theories of temporomandibular joint pain dysfunction syndrome: the theory of occlusal imbalance and the psychophysiological theory. Adherents of the first theory believe that the root cause of functional disorders is a violation of the closure of teeth. It leads to compensatory protective muscle contraction with the development of parafunctional increased activity. In the future, this causes muscle pain syndrome with temporary preservation of the correct position of the head of the lower jaw without disturbing the position of the articular disc.
At the beginning of the disease, residual tension occurs in the muscle, and then a stable local increase in tone develops. It causes short-term painful muscle spasms when you forcefully open your mouth or yawn. In other cases, increased tone leads to stable muscle tension.
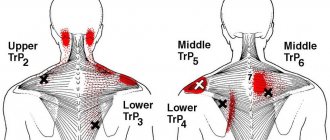
If increased tone persists for a long time, vascular, metabolic and inflammatory disorders occur in the muscle. Local hypertonicity becomes a source of pain and turns into trigger points, which can be found in the masticatory muscles, the lateral and medial pterygoids, and the temporal muscle.
With a long-term change in occlusal relationships, the load on the joint increases due to the type of compression. He begins to adapt to new intra-articular relationships. When compensatory capabilities are depleted, the shock-absorbing properties of the soft tissue components of the joint are lost. Compensation for the increased load on the tissues of the joint is manifested by degenerative changes and adaptive changes in the elements of the joint, which leads to pain.
Temporomandibular joint pain dysfunction syndrome also develops in patients suffering from depressive disorders. Many people in a state of emotional stress experience spontaneous contraction of the masticatory muscles. They experience spasm, loss of coordination, occlusal disorders, and injury to the soft tissues of the joint. Violation of occlusion against the background of chronic stressful situations turns out to be a direct cause of joint dysfunction.
Treatment of the temporomandibular joint
Complex treatment of TMJ is possible only in dentistry, and is possible thanks to:
- surgery on the lower jaw;
- orthodontic treatment
(prescribing special trainers that will be worn at night and reduce pain by adjusting the load on the joint - the same trainers are recommended for bruxism) and bite correction with braces;
- orthopedic treatment
and
implantation
(insert a suitable prosthesis to restore the correct closure of the jaws).
Treatment is always prescribed individually, based on the results of an examination by an orthodontist, and is most often carried out comprehensively. It is dangerous to neglect TMJ diseases: this can lead to arthrosis, in which connective tissue grows in the joint cavity, which, in turn, threatens complete immobilization of the joint (ankylosis).
Severe pain and joint spasms can be relieved with compresses and painkillers; Stresses that provoke tension in the joint can be relieved with sedatives, but all these are half measures that do not treat the root cause of the pain.