Detailed description of the study
Rheumatoid arthritis (RA) is an autoimmune disease that is accompanied by the development of chronic damage to the joints—usually the hands and fingers—and internal organs. The course of RA can be rapidly progressive or slowly progressive. Along with damage to the joints, swelling and pain in them, stiffness of movement in the morning after sleep, the disease has such nonspecific manifestations as weakness, fatigue, and weight loss. The disease is characterized by the formation of specific rheumatoid nodules under the skin, as one of the most common extra-articular manifestations.
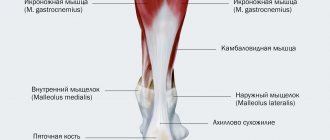
Delayed detection of RA has many adverse consequences. Long-term pathological changes in the joints cause impairment of their mobility and, without treatment, lead to disability. Deposits of pathological amyloid protein are found in organs and tissues, and amyloidosis develops. RA is also the cause of so-called tunnel syndromes, which are caused by compression of nerves and blood vessels in anatomical canals, or tunnels. The most common types are carpal tunnel syndrome and compression syndromes of the ulnar and tibial nerves.
Rheumatoid arthritis is differentiated from a number of other diseases that begin with joint damage. These include joint injuries, some acute infectious diseases such as influenza, rubella, measles, hepatitis, post-streptococcal arthritis, as well as gout, osteoarthritis and other rheumatic diseases.
This study is aimed at identifying RA and includes five important indicators. It is worth noting that RA has seropositive and seronegative forms, which are determined depending on the detection of rheumatoid factor in the blood.
Rheumatoid factor
Normally, immunoglobulins (antibodies, antibodies) protect a person from the harmful effects of microorganisms and foreign substances. They are proteins that differ in their structure and function. They are divided into five classes: IgG, IgM, IgA, IgD and IgE. Antibodies, united by the concept of “rheumatoid factor” (RF), most often belong to the IgM class, are produced against parts of one’s own IgG, altered in rheumatoid arthritis due to various not fully established reasons. Their determination is one of the key stages in establishing the diagnosis of RA.
SSR antibodies
Cyclic citrulline-containing peptide (CCP, CCP) is a protein in which the normally absent amino acid citrulline replaces the physiological amino acid arginine. Determination of antibodies to CCP makes it possible to determine the presence of the disease with a high probability, including in seronegative RA. For early arthritis, its sensitivity is 41-80% and specificity is 93-99%.
ASLO
Antistreptolysin-O (ASLO) are also a group of antibodies directed to bacterial molecules: group A beta-hemolytic streptococcus - streptolysin. This microorganism is one of the causative agents of sore throat, scarlet fever and some other diseases. Previous streptococcal infection is often associated with the subsequent occurrence of autoimmune diseases.
The study also contains two tests: determination of C-reactive protein and a clinical blood test. The concentration of the former may reflect the presence of an acute stage of RA and is associated with disease activity. Together, these two tests allow us to assess the presence of inflammatory processes and their intensity.
Thus, this complex study is widely used in clinical practice, since it can highly likely confirm or exclude RA; it is also used to monitor the effectiveness of treatment and assess the prognosis of the disease.
A detailed description of the studies and reference values are presented on the pages with descriptions of individual studies.
2. Reasons
In the most general terms, the etiopathogenesis of rheumatism is understood as an inadequate (pathologically aggravated) immune-allergic reaction to an infectious-inflammatory process spreading from an acute or chronic source of infection. In the presence of an innate individual feature, which consists in a certain similarity of connective tissue cells with pathogen cells, immune factors in the blood begin to attack their own tissues, mistaking them for the causative agent of infection.
The most common (although not the only) infectious agent that can trigger the rheumatic process is streptococcus, and the greatest risk is created by commonplace acute respiratory infections and nasopharyngeal inflammation (tonsillitis, pharyngitis, frequent sore throats, etc.). Under unfavorable conditions and individual predisposition, rheumatism begins as a result of streptococcal invasion in 0.3-3% of infected people, which is a very high risk, given the prevalence of pathogenic streptococcal strains.
Complex, multifactorial mechanisms and patterns of development of rheumatic diseases today remain the object of intensive scientific and medical research, which gives reason to hope for the emergence, in the foreseeable future, of methods of effective etiopathogenetic treatment (for example, immuno- or gene therapy).
Visit our Rheumatology page
References
- Rheumatoid arthritis. Clinical recommendations. Association of Rheumatologists of Russia, 2021. - 102 p.
- Rheumatology: National Guide / ed. E.L. Nasonova, V.A. Nasonova. - M.: GEOTAR-Media, 2008. - 720 p.
- Kishkun, A.A. Guide to laboratory diagnostic methods. - M.: GEOTAR-Media, 2007. - 800 p.
- Volkova, M.V., Kunder, E.V. Early arthritis: relevance, Immunopathology, diagnosis. Vestnik VSMU, 2013. - No. 3.
- Medical microbiology, virology and immunology: a textbook for medical students / ed. ed. A.A. Vorobyov. — 2nd ed., corrections and additions. - M.: Medical Information Agency, 2012. - 704 p.
3. Symptoms and diagnosis
Acute rheumatic fever develops quickly and in its manifestations is often indistinguishable from the clinical manifestations of severe ARVI (general malaise, fever itself, high temperature, headache and joint-muscular pain, etc.).
Chronic rheumatism occurs, as a rule, with several relapses per year and is a severe, disabling disease, which, in the absence of adequate treatment and with the accumulation of pathological changes in tissues and organs, becomes increasingly dangerous in prognostic terms.
The specific symptom complex depends on the predominant system of the body in which the inflammatory process develops. As stated above, there are various forms of rheumatism:
- cardiac (inflammation of certain myocardial structures, specific granulomatosis, formation of defects and general cardiac functional failure);
- articular (pain and swelling of inflamed joints, progressive failure of cartilaginous layers and joint capsules - rheumatoid arthritis);
- mixed (the general syndrome combines the first two variants of the clinical picture).
There are also neurological, pulmonary, and gastrointestinal forms, each of which is manifested by symptoms specific to a given system (in particular, disorders of muscle contractile activity, severe damage to the retina with the threat of complete blindness, and many others).
Rheumatic processes can create diagnostic difficulties, since in the acute period not only the clinical picture is nonspecific, but also the picture of laboratory parameters; chronic forms are much easier to recognize.
If rheumatism is suspected, the medical history is carefully studied (frequent acute respiratory infections, acute respiratory viral infections, chronic streptococcal tonsillitis, tonsillitis), and general clinical and immunological blood tests are prescribed (markers of inflammation and immune response factors). Of the instrumental methods, the most informative are ECG, echocardiography (ultrasound of the heart), radiography, if indicated - biopsy, arthroscopy, etc. Various criteria are used, developed for reliable recognition and differentiation of rheumatism from inflammation of other etiologies.
About our clinic Chistye Prudy metro station Medintercom page!
Treatment
Rheumatism reduces the quality of life, affecting the joints and heart. Inflammation must be treated quickly and effectively. The fight against rheumatism includes:
- antibacterial therapy aimed at eliminating streptococci and removing the products of their vital activity and decay;
- taking acetylsalicylic acid in high doses;
- hormonal therapy - prednisolone in the maximum allowable dosage;
- compliance by the patient with bed rest, excluding physical activity;
- long-term bicillin therapy.
In the remission stage, physiotherapeutic procedures, acupuncture, therapeutic exercises, and sanatorium treatment are prescribed.
You can make an appointment with a specialized specialist at EmmaClinic for consultation on the diagnosis and treatment of rheumatism by phone or by filling out an application on the website.
Branch:
Orthopedics
Make an appointment (video consultation available)
Your message has been sent
Thank you for contacting Multidisciplinary Medical!
Your message will be processed shortly and we will contact you to clarify the details.
Be healthy!
Join us on social networks!
Current news, promotions, useful information.
How to find us
OUR ADDRESS
Moscow, st. Shchukinskaya, 2
Shchukinskaya, Streshnevo, Sokol
TELEPHONE
+7
4.Treatment
Therapy for rheumatic disorders is effective and successful in cases where it begins in a timely manner, is comprehensive, covers a sufficiently long period of time and is carried out with full compliance (meaningful, “cooperative” position of the patient). Thus, in a number of cases, the use of antibiotic drugs (a primary measure) is prescribed for a period of several years, in combination with powerful non-steroidal and/or hormonal anti-inflammatory drugs, immunocorrectors, cardio-, chondro- and angioprotectors, other medications according to indications, as well as physiotherapeutic and spa treatment. An acute period of rheumatism creates indications for hospitalization and inpatient treatment; in the future, dispensary observation with control examinations every six months and resolution of medical and social issues, as necessary, is mandatory.
Symptoms
Rheumatism is accompanied by:
- high temperature, fever, and such symptoms appear two to three weeks after an infectious lesion of the upper respiratory tract;
- weakness, lethargy, fatigue, sweating, loss of appetite;
- severe joint pain (rheumatoid arthritis);
- pain in the heart area, tachycardia, shortness of breath (rheumatic heart disease, heart defects);
- involuntary twitching of the face, eyelids, lips, head (chorea);
- ring-shaped erythema;
- subcutaneous rheumatoid nodules.
If these symptoms appear, you should immediately consult a doctor. In medicine, experienced doctors are able to identify rheumatic lesions of the heart, joints, and nervous system in the early stages of the inflammatory process.
General blood analysis
A general blood test for knee arthritis reflects general signs of inflammation.
In a healthy person, the hemoglobin level varies from 120 to 150 grams per liter. In rheumatoid arthritis, a chronic inflammatory process leads to a gradual depletion of red blood cell synthesis and the development of anemia. The severity of anemia in the case of a confirmed diagnosis of rheumatoid arthritis is proportional to the intensity of the inflammatory process.
Finger prick blood test
Types of anemia found in chronic arthritis:
- Normochromic anemia is characterized by a preserved color indicator with a decrease in the number of red blood cells per unit volume of blood.
- Hypochromic anemia - the color index is reduced, the number of red blood cells decreases.
- Normocytic anemia is characterized by preservation of the diameter of red blood cells.
- Microcytic anemia is a decrease in the diameter of red blood cells.
Anemia in rheumatoid arthritis is moderate and not pronounced.
Another indicator characterizing the presence of an inflammatory process is an increase in the number of leukocytes per unit volume of blood.
The norm for a healthy adult is the number of leukocytes from 4 to 9 *10. Leukocytosis in arthritis varies from moderate to severe.
- ESR in rheumatoid arthritis - Orthopedist.info
Erythrocyte sedimentation rate (ESR) is an indicator of the presence of inflammation in the human body. The indicator determines the rate at which red blood cells settle to the bottom of a laboratory test tube. The rate depends on the density of plasma protein, which is associated with the presence of inflammatory mediator proteins in the plasma. At this time, protein fragments are adsorbed on the walls of red blood cells, making them heavier and causing them to settle faster. In a healthy person, the rate does not exceed 10-15 millimeters per hour.
ESR is not highly specific for any type of disease; it is a general sign of the presence of a nonspecific inflammatory process. With arthrosis, the ESR level remains normal and serves as a criterion for differentiation.
The value of the indicator is proportional to the intensity of the inflammatory process.
In order for a general blood test to show reliable results, it is worth knowing the donation rules. This is done in the morning on an empty stomach. For a few days, you should stop eating foods rich in animal fats. The day before, you should limit physical activity. Those who come to the clinical laboratory on their own should sit down and take a break before taking a general blood test.
Increased indicators in a child
Even the youngest children can have pathologies of a rheumatic nature. Symptoms appear in a hidden form, and due to unconsciousness, it is more difficult for the child to explain what is bothering him. Complaints of pain in the legs, arms and knees, or simply constant crying may be the first signs of the development of the disease. A disease such as juvenile rheumatoid arthritis has a chronic nature of manifestation and develops in children under 16 years of age.
Pathology can be detected even in young children
During a diagnostic examination to clarify the diagnosis, the following is carried out:
- Blood test to detect infectious viruses: beta-hemolytic streptococcus, cytomegalovirus, herpetic type virus, chlamydia.
- Collection for the study of intestinal bacteria (Yersinia, Shigella, Salmonella) and parasites.
- Electrocardiogram.
- Ultrasound of the abdominal organs, heart, kidneys.
- X-ray of joints, sternum, sacroiliac joints and spine.
In addition to a general differential examination, all children with joint diseases are advised to visit an ophthalmologist and undergo a slit lamp examination.