The main function of the shoulder joint is to move the arm in different planes. To avoid damage to the body during this process, there are three bursae or bursae located inside the shoulder. They contain a special liquid that acts as a natural lubricant. In case of injury, accumulation of salts, severe infection in the body and other reasons, there is a possibility of developing bursitis. It is an inflammatory disease that is usually classified by location. For example, one of the common types of this disease is subdeltoid bursitis of the shoulder joint. In this article we will look at the causes of development, main symptoms and ways to prevent this disease.
What is shoulder bursitis - description of the disease
Bursitis of the shoulder joint is an inflammation that develops in the synovial bursa, leading to damage to the tendons and the formation of a tumor with purulent contents. Develops as a result of severe trauma, regular stress, or infection. The shoulder joint consists of the humerus, forearm and cartilage. There are a large number of muscles around the joint that are needed for normal bone mobility. To avoid rubbing of the bones and their deformation, there are special bags around them - synovial pockets, which contain a viscous liquid inside. It provides elastic movement of the bag and helps maintain its normal shape. The shoulder is surrounded by three such synovial pouches, one of which is called subdeltoid, which is the name given to the form of the disease. This bursa is located at the back of the joint and is especially important for vertical movement of the arm.
Causes and mechanism of development
All causes that can lead to inflammation of the bursa can be grouped into 2 groups - infectious and aseptic. More often, the disease is caused by non-infectious factors, such as injuries and excessive stress on the shoulder. The chronic form is common among men who play sports professionally or are engaged in heavy physical labor with a load on the shoulder joint (these are miners, loaders). Sometimes just one bruise, dislocation or sprain is enough for shoulder bursitis to appear.
Aseptic inflammation can also be triggered by other factors:
- metabolic disorders, such as gout;
- autoimmune diseases;
- allergic reaction.
Predisposing factors for bursitis include old age over 50 years. Due to age-related changes, the ligamentous-muscular system loses tone, so the joint is more susceptible to mechanical damage.
Infectious bursitis occurs when exposed to pathogenic microflora. It comes in two types:
- nonspecific – caused by nonspecific agents, for example, streptococci, staphylococci;
- specific - arising against the background of a pale spirochete, tuberculosis bacillus.
Infectious agents can penetrate the synovial bursa through microdamages, adjacent infected tissues (boils, abscesses), as well as through the blood and lymph flow if the source of infection is far from the shoulder.
An infectious form can occur against the background of an existing aseptic form.
How does shoulder bursitis occur? The bursa protects joint elements and tissues from damage. It contains a small amount of liquid. As soon as its inner lining becomes inflamed, the production of effusion increases, and it begins to accumulate inside the bursa. With aseptic bursitis, the bursa is filled predominantly with serous exudate, and with infectious bursitis, it is filled with purulent exudate.
Causes
Most often, shoulder bursitis appears in people with increased physical activity, athletes, and people working in heavy work. But there are other causes of inflammation:
- excessive constant loads;
- gout;
- injury, bruise;
- impaired metabolism of the body;
- allergic reactions;
- weak immune system;
- poisoning the body with alcohol or nicotine.
Bursitis can appear due to one or several reasons. More often, inflammation occurs due to a shoulder injury. In this case, during a blow or bruise, the synovial bursa is compressed. Its walls are deformed and cannot take their original shape - an inflammatory process appears, which also affects the cavity of the bag and the fluid in it. Pathological changes occur in the fluid, which entail the appearance of swelling of the joint and the appearance of pain with any movement of the hands.
The inflammatory process in this part of the shoulder joint occurs in professional athletes, especially volleyball players, basketball players, and tennis players. The disease develops due to the fact that the bursa does not have time to fully recover in the short period between workouts.
Is it possible to run with calcaneal bursitis? It is discussed in this article.
Treatment methods
Subdeltoid bursitis must be treated comprehensively. Only in this case can you count on a speedy recovery. A course of therapy against this disorder usually includes several methods that promote the restoration of damaged tissue.
Drug therapy
For various types of bursitis, anti-inflammatory and painkillers are prescribed. They usually come in the form of tablets and are meant to be taken orally. Additionally, doctors recommend using ointments with an anti-inflammatory effect. Such medications are more preferable because they do not affect internal organs. The active substances enter exclusively the damaged joint.
Surgical intervention
This treatment method is required for advanced bursitis. During surgery, the surgeon removes part of the periarticular bursa that has been damaged due to the disease. It may be necessary to completely open the bursa and thoroughly rinse it with an antiseptic solution.
Physiotherapeutic procedures
During treatment, patients are advised to tie a tight bandage around the affected limb. To restore the shoulder joint, you should attend therapeutic massages. Physiotherapy helps eliminate pain. These include phonophoresis, magnetic therapy, laser irradiation and electrophoresis. Additionally, painkillers are used, which enhance the effect of the treatment course.
Throughout the entire treatment, a patient with shoulder bursitis must strictly follow all the specialist’s instructions. Under no circumstances should you replace medications or change their dosage yourself. Also, do not refuse to attend physiotherapeutic procedures. Otherwise, the course of treatment for subdeltoid bursitis will be greatly delayed. In addition, this can lead to complications in the pathological process.
Differences between subdeltoid and subdeltoid bursitis of the shoulder
Often subdeltoid bursitis of the shoulder is diagnosed with subdeltoid. However, there are some differences between:
- The inflammatory process with subdeltoid (subacromial) bursitis affects the upper and lower surfaces of the joint capsule . Blood enters the synovial cavity of the pouch, and the normal lubricating fluid disappears. In this case, the patient experiences severe sharp pain when moving the arm to the side, but when moving forward and backward, there is no discomfort;
- with subdeltoid bursitis, a point pathology of the bursa occurs behind or above, but it is rarely completely affected . This form of the disease is accompanied by constant severe pain not only in the shoulder, but also in the adjacent arm with any movement, touch, and even when changing body position.
Technically, the difference between these types of bursitis is only in anatomy and physiology. The general course, treatment methods and symptoms are very similar.
Symptoms of bursitis
Symptoms of bursitis in acute and chronic forms differ in the intensity of the pain syndrome. During an exacerbation, a rounded swelling forms in the area of the affected joint, palpation of which causes sharp pain. In the acute period, body temperature often rises.
Symptoms of acute joint bursitis increase gradually, along with increased swelling and redness of the tissue. Severe pain syndrome significantly reduces performance, leads to motor restrictions and deterioration of well-being. At the height of the disease, body temperature can rise to 40 °C. With an unfavorable course and the absence of effective anti-inflammatory treatment, the risk of purulent tissue melting increases sharply.
Up to contents
Symptoms
Identifying symptoms is an important part of visual diagnosis of the disease. Signs of an inflammatory process in the subdeltoid part of the shoulder are:
- swelling of the tissues around the sore joint;
- severe pain that intensifies when moving the arm to the sides and palpating the shoulder;
- discomfort when carrying objects or bags on the shoulder;
- mobility of the stave is severely limited;
- joint sensitivity is reduced;
- in rare cases, the hand and forearm may become numb;
- muscle tone is increased.
Bursitis is often accompanied by swelling of the affected shoulder, where inflammation occurs. In case of improper treatment or lack thereof, the swelling hardens and develops into a tumor. Its size can reach up to 18 cm in diameter. Such a neoplasm significantly worsens the quality of life and causes discomfort. A person with such a tumor will not be able to fully lower and raise his arm or make swings. After some time, the bursa begins to constantly hurt on its own, and the pain intensifies at night and can spread to neighboring joints - the elbow or scapula. This may also cause the limbs to go numb. The pain becomes stronger every day, hyperthermia occurs, and vomiting is possible.
The tumor prevents a person from lifting objects due to strong pressure on the subdeltoid bursa. At the same time, it is deformed: the walls thicken, and the shape becomes elongated.
When to remove the bandage after the elbow bursitis fluid has been pumped out, you can find out in this material.
Bursitis - causes and effective treatments for bursitis
open page: treatment of bursitis
Bursitis (bursa) translated from Latin means bag.
Bursitis is an inflammatory disease of the synovial bursae, accompanied by increased formation and accumulation of exudate in their cavities. The ESMA company presents professional medical equipment and devices for the treatment of bursitis and other diseases and injuries. Equipment for sports rehabilitation medicine.
According to the clinical course, bursitis can be acute, subacute, chronic, recurrent; by the nature of the pathogen - nonspecific or specific (gonorrhea, brucellosis, tuberculosis, syphilitic); according to the nature of the exudate - serous, purulent or hemorrhagic. Some authors distinguish aseptic and infected bursitis.
Synovial bursae
- slit-like cavities formed by the synovial membrane, containing synovial fluid. Synovial bursae belong to the auxiliary apparatus of muscles. They are located in the tissue between protruding areas of bones and soft tissues (skin, fascia, muscle tendons, muscles). The following synovial bursae are distinguished: subcutaneous - located in the subcutaneous tissue on the convex surface of the joint, subject to sharp flexion; subfascial - located under the fascia; subtendinous - located under the tendons; axillary - lying under the muscles. Subtendinous bursae in adults often communicate with the joint cavity. Surrounding the muscle tendon for a considerable extent, they can form a synovial tendon sheath.
Exudate
- a liquid rich in protein and containing formed elements of blood; formed during inflammation.
The inflammatory process can occur both in permanent and newly formed bags in places of continuous pressure and friction of the skin, fascia, muscles, tendons on bone protrusions. The most common bursitis is bursitis of the elbow bursae and synovial bursae of the knee and shoulder joints. The frequency of such localization is determined by constant injury to the corresponding parts of the body due to the characteristics of certain sports. This allows us to classify bursitis as an occupational disease. The incidence of bursitis depends on the type of sport and other variables (sports activity regimens, equipment, skill level, etc.).
Causes of bursitis
The cause of acute bursitis is often trauma - bruise, abrasion, minor wounds and secondary infection of the synovial bursa with pyogenic microbes. Infection of the synovial bursae occurs through the lymphatic ducts from purulent foci (with erysipelas, boils, carbuncles, osteomyelitis, bedsores), and infection through the blood cannot be excluded. The possibility of infection due to a cut or abrasion in the area of the joint capsule (falling from a bicycle, playing football) cannot be ruled out. Chronic bursitis is often the result of long-term, constant mechanical irritation. Pathological anatomy. Pathological changes in acute bursitis are expressed by signs of acute inflammation of the walls of the synovial bursa.
The initial stages of acute bursitis are characterized by serous penetration of tissues and accumulation of serous exudate in the cavity of the bursa (acute serous bursitis). In the presence of microbial flora, serous inflammation quickly turns into purulent inflammation (purulent bursitis). The spread of the purulent process to surrounding tissues can occur as a phlegmonous inflammation with necrosis of the bursa wall and the formation of subcutaneous and intermuscular phlegmon. In advanced cases, fistulas that do not heal for a long time are formed. The breakthrough of pus into the joint cavity leads to the development of purulent arthritis.
In acute traumatic bursitis, hemorrhagic fluid (blood or plasma) accumulates in the stretched synovial bursae and their pockets. With reverse development, fibrin is organized and the vessels of the synovial membrane are obliterated. Persistent changes develop in the wall of the bursa, which thickens, the surface of the synovial membrane is covered with growths of connective tissue (proliferative bursitis), dividing the cavity of the bursa into additional pockets.
When acute inflammation subsides and in the subacute course of bursitis, encapsulated areas of necrotic tissue or exudate remain in the wall and pockets of the bursae, which, with repeated injury and infection, serve as fertile ground for the development of recurrent inflammation (recurrent bursitis).
Symptoms of bursitis
At the site of the anatomical location of the bursa, a round, limited, painful swelling of a soft-elastic consistency, fluctuating, is determined. The diameter of the swelling can reach 8-10 cm (Fig. 1). The patient complains of pain in the area of swelling, malaise; body temperature rises; joint function is moderately limited.
With phlegmonous inflammation, there is swelling of the tissues surrounding the bursa, hyperemia of the skin (lymphangitis), and general symptoms of the disease are pronounced (especially with gonorrheal bursitis): severe pain, fever up to 39-40°. As inflammation progresses and spreads to soft tissue, signs of phlegmon are determined.
In chronic bursitis, at the location of the bursa there is a rounded, limited swelling of soft consistency, the skin over it is mobile, not changed, and the function of the limb is not impaired. The chronic process may worsen; this increases the amount of fluid in the cavity of the bag, which sometimes leads to the formation of an isolated cystic cavity filled with fluid, called a hygroma.
Features of bursitis of different localization
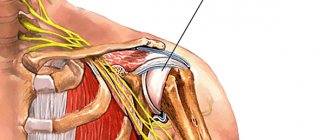
Shoulder joint
In the area of the shoulder joint, the most commonly affected bursae are those that do not communicate with the joint cavity, the subcutaneous acromial, subdeltoid and subacromial (Fig. 2). Complaints boil down to pain during abduction and rotation of the upper limb. Bursitis of the subdeltoid bursa is especially painful.
Area of the left shoulder joint, rear view (Fig. 2):
- Bursa between the crura of the coracoacromial ligament
- Bursa of the coracobrachialis muscle
- Shoulder joint capsule
- subscapularis bursa
- Bursa of the teres major muscle
- Latissimus dorsi bursa
- Subacromial bursa
- Acromial bursa
Upon examination, the contours of the shoulder are smoothed, and there is an apparent uniform increase in the deltoid muscle itself; with large bags, swelling is visible on the outer surface of the shoulder. Palpation usually reveals pain when pressing on the inner edge of the greater tuberosity of the humerus. Supraclavicular bursitis often has to be differentiated from purulent arthritis, as well as from a very common disease of the shoulder joint - glenohumeral periarthritis.
Elbow joint
Acute bursitis of the ulnar bursa is most often the result of mechanical damage and infection of the subcutaneous ulnar bursa due to injury. The bag increases sharply in size and takes on a hemispherical shape. The addition of infection is accompanied by the appearance of severe pain, redness of the skin in the area of the olecranon, and increased temperature. Acute bursitis often affects the radiohumeral bursa, located between the tuberosity of the radius and the biceps tendon (Fig. 3) (tennis players' bursitis).
The area of the right elbow joint, rear view (a) and front view (b) (Fig. 3):
- ulnar subcutaneous bursa
- interosseous ulnar bursa
- shoulder bag
Hip joint
Bursitis in the hip joint varies in severity; inflammation often spreads to the hip joint. More often, the deep-lying iliopectinal bursa, located between the muscles and the joint capsule, as well as the superficial and deep bursa of the greater trochanter are subject to inflammation. With purulent inflammation of these bags, sharp pain is noted when abducting the limb, extending and rotating the hip. The hip is in flexion, abducted and slightly externally rotated. Upon palpation, a painful, elastic swelling is determined along the anteromedial surface of the thigh under the inguinal ligament. With purulent inflammation of the greater trochanteric bursa, the swelling is often located on the outer surface of the thigh. Based on the severity of the clinical course and the similarity of symptoms, these types of bursitis are in some cases difficult to distinguish from purulent inflammation of the hip joint. With bursitis, in contrast to arthritis, the following are observed: 1) relative painlessness of flexion and adduction of the hip; 2) absence of pain when loading the limb along its length; 3) the presence of a swelling located on the anterior inner side of the thigh below the inguinal ligament. To distinguish the lesion of the subcutaneous bursa of the greater trochanter from the lesion of the deep bursa allows the displacement of the latter during posterior movements of the hip; with inflammation of the subcutaneous trochanteric bursa, no displacement is noted.
Knee-joint
In the area of the knee joint, the prepatellar bursae are most often affected - subcutaneous, subfascial and subtendinous (Fig. 4); they do not communicate with the knee joint. Due to its more superficial location, the subcutaneous bursa is most often affected. Inflammation is accompanied by severe local edema, fluctuation, increased temperature, and enlarged regional lymph nodes. Inflammation of the deep infrapatellar bursa often occurs secondarily as a complication of acute gonitis. Popliteal bursitis is difficult to diagnose due to the deep location of the bursa; with it there is some restriction of movement and pain in the knee joint.
The area of the right knee joint, front view (a) and longitudinal section (b) (Fig. 4):
- 1-6. joint capsule
- Deep infrapatellar bursa
- Superficial pretibial bursa
- Bursa of the semimembranosus muscle
- Medial subtendinous bursa of the gastrocnemius muscle
- Superior patellar bursa
- Subcutaneous prepatellar bursa
- Subfascial prepatellar bursa
- Subtendinous prepatellar bursa
Ankle joint
A common type of bursitis in the foot area is inflammation of a large bursa located between the heel tubercle and the heel tendon - Achilles bursitis. It is caused by trauma to the synovial bursa with shoes, hematogenous or lymphogenous infection. Bursitis of the subcutaneous heel bursa is a painful swelling in the area of the heel tubercle. The inflammatory process may be limited to the serous impregnation phase or lead to abscess formation. In some cases, this type of bursitis must be differentiated from inflammation caused by injury to the soft tissues of the heel “spur.”
Treatment
Diagnosis
is simple for inflammation of superficially located bursae and is based on the typical clinical signs described above. The diagnosis is facilitated by puncture of the bursa cavity, which makes it possible to determine from the resulting contents the nature of the inflammation (serous, purulent, purulent-hemorrhagic, etc.), to determine the nature of the microbial flora and its sensitivity to antibiotics.
To carry out the most effective treatment, it is important to exclude the specificity of the infection that caused the inflammation (gonococci, brucella, spirochetes, etc.), which is possible on the basis of a carefully collected anamnesis, bacteriological examination of the contents of the bags, and the results of specific serological reactions. The main differential diagnostic feature to distinguish bursitis from arthritis is the preservation of movement in the joint. X-ray diagnosis of superficial (subcutaneous) bursitis of any location is relatively simple. Due to their availability for clinical recognition, it is usually only of a clarifying nature. X-ray diagnostics of deep bursitis is of much greater practical importance. Among them, the radiologist most often encounters bursitis of the knee joint and greater trochanter of the femur, achillobursitis and inflammation of the unstable subacromial mucous bursa, and on the upper limb - with chronic subacromial bursitis.
For acute bursitis in the early stages, rest, a pressure bandage, and warm compresses are recommended. To prevent purulent bursitis, early active treatment of the serous form of acute bursitis and the use of fixing bandages is necessary.
In case of chronic bursitis, they often resort to puncture with removal of exudate and subsequent washing of the bursa cavity with solutions of antiseptics or antibiotics. For traumatic bursitis, a hydrocortisone solution is injected into the cavity of the synovial bursa (25-50 mg with antibiotics 2 to 5 times after preliminary administration of 8-10 ml of a 2% novocaine solution). Careful adherence to asepsis is important, as otherwise serious complications are possible. For purulent bursitis, puncture treatment is used. If the process progresses, they resort to opening the bag and removing the pus; a purulent wound is treated according to general rules. The disadvantage of this method is the duration of healing of the surgical wound.
Forecast
in acute bursitis depends on the degree of pathological changes in the tissues of the affected bursae, their prevalence, the ability of the infection to spread, and the patient’s body’s resistance. Unfavorable outcomes of acute bursitis can occur when it is complicated by arthritis, osteomyelitis, fistulas, and sepsis. Relapse in chronic traumatic bursitis is observed in 2-2.5% of those operated on.
Prevention
consists of eliminating constant trauma to the synovial bursae, in particular wearing protective bandages, careful primary treatment of wounds of the synovial bursae with antiseptics (treatment with hydrogen peroxide, application of a bactericidal patch/bandage), timely and rational treatment of pustular diseases.
Professional medical equipment and devices for sports rehabilitation medicine ESMA.
The photo shows the following models of devices: Computer medical equipment - device - complex ESMA 12.48 FAVORITE Multifunctional portable device ESMA 12.04 MINIMAX
ESMA devices cosmetology ESMA devices therapy ESMA devices sports medicine, fitness High performance sports
Features of treatment
If characteristic symptoms of the disease or any other discomfort in movement appear, you should consult a doctor for help. Only he will be able to make an accurate diagnosis and prescribe the necessary treatment. To diagnose the disease, the doctor may prescribe the following methods :
- Blood and synovial fluid tests;
- X-ray;
- Ultrasound of the shoulder.
Ultrasound examination of the shoulder joint.
The disease can be treated in several ways, depending on the severity and cause of inflammation. There are such treatment methods:
- Medicines and drugs . If the disease is not protracted and it is possible to cure the disease without surgery, medications are prescribed. If the cause of the disease was pathogenic microorganisms, then the patient is prescribed broad-spectrum antibiotics (Penicillin, Tetracycline, Levomycetin). If the cause is not clear, then non-steroidal anti-inflammatory drugs are prescribed.
- Surgical intervention is necessary in case of protracted bursitis with a severe degree of the disease. If the bursa cannot be treated, it is removed. If the inflammatory process occurs in a chronic form, then the cavity of the bag is opened and thoroughly washed from pus or blood using antiseptics.
- At home, it is necessary to limit the load on the sore shoulder, prescribe complete rest and special therapeutic massage procedures. It is also necessary to wear a fixation bandage to prevent any movement of the shoulder joint. It is worn during treatment and a month after it. The bandage helps keep the joint in the desired position without movement to eliminate the risk of deformation of the synovial bursa.
Treatment of bursitis is a complex and lengthy process that can take several months. During this time, you need to limit the load on the joint as much as possible and follow all doctor’s instructions. General restoration of the joint is usually achieved only a year after the start of treatment. The duration of therapy depends on the age and structural features of the body.
Diagnostics
The specialist can make a presumptive diagnosis for the patient based on the information that was collected while asking the person about his complaints. The mechanism of injury is also taken into account. To confirm the doctor’s assumptions, the patient must undergo a series of tests and undergo standard diagnostic procedures.
The pathological condition observed in the shoulder joint is recognized using the following studies:
- Blood test to determine the presence of an inflammatory process in the body;
- Analysis of synovial fluid. It is obtained by puncture. This diagnosis makes it possible to determine the location of inflammation, its nature and even its cause. Not only pathogenic bacteria, but also impurities of pus or blood can be detected in the liquid;
- X-ray examination. Allows you to exclude or confirm the presence of trauma to the bone elements of the upper limb;
- Ultrasound. Required to examine the joint itself. During the procedure, the doctor will see swelling of the bursa and its stretching. It will also determine the volume of liquid that has accumulated in this area.
The results of the patient’s diagnostics give the doctor the opportunity to correctly determine the diagnosis. After this, he will prescribe suitable treatment for him, which should lead to recovery.
To make a final diagnosis, both laboratory and hardware tests are needed
Prevention
After treatment, prevention and rehabilitation are necessary.
When the inflammation has completely passed, the patient is prescribed a course of physical procedures to restore shoulder mobility, form a muscle corset and normalize functioning. Prevention means a set of actions that minimize the risk of recurrence of the disease. To do this, patients are advised to wear special fixing bandages and avoid injuries or bruises to the shoulder.
In case of wounds, cuts or scratches on the shoulder, they must be immediately treated with disinfectants to prevent pathogenic microflora from entering the body.
Treatment of the problem
Therapy for subdeltoid inflammation of the shoulder joint begins with immobilizing the joint using a fixator, as well as removing physical stress from the limb. After this, the use of therapeutic agents is aimed at relieving pain attacks and eliminating inflammation in the joint. For this purpose, use: “Celebrex”, “Fastum-Gel”, “Nise” or “Nise-Gel”. In the case of an infectious nature of the lesion, the patient is prescribed medications that destroy pathogenic microbes and bacteria. To make the therapy more effective, the patient may be prescribed special exercises, massage sessions or physical therapy.
conclusions
- If you suspect bursitis, there is no need to self-medicate , since improper treatment will only lead to serious consequences in which surgery cannot be avoided.
- In case of a strong blow or bruise to the shoulder, it is better to consult a doctor, and in case of scratches and cuts, you should immediately treat the wound to reduce the risk of illness .
- In case of excessive physical activity, you need to protect your ligaments and joints using special bandages .
- It is easier to treat shoulder bursitis in the early stages, so do not delay a visit to the hospital if signs of the disease are detected.
Diagnosis of shoulder bursitis
Diagnosis of shoulder bursitis is carried out in several modern ways:
Analyzes
Ultrasound of joints
Shoulder MRI
Causes
Pathogenic microorganisms are one of the most common causes of bursitis. In a number of diseases, infection penetrates into the bursa, causing purulent bursitis to develop. Microorganisms can also enter through an open wound.
Injuries, bruises, and sprains can often cause bursitis. Falls, blows, and prolonged overloads lead to inflammation of the periarticular bursa.
Overload also occurs in people of certain professions. Thus, athletes and loaders often suffer from subdeltoid bursitis. A joint that is constantly in motion stretches the synovial bursa, which leads to the development of inflammation.
Other causes of this disease include metabolic diseases (gout), autoimmune, allergic reactions, and general intoxication.
How to identify the disease
Most often, the diagnosis of the disease is made based on characteristic symptoms and examination of the patient. To differentiate the disease from other pathologies, it is necessary to prescribe instrumental examination methods:
- Radiography . It is used to rule out another disease. This research method is used if the patient’s inflammatory process has been observed for a long period and is characterized by an infectious nature.
- Magnetic resonance imaging. This research method is widely used due to its high information content. With its help, it is possible to determine the presence of minimal violations.
- Ultrasound examination . With its help, the localization of inflammation is accurately determined. This diagnostic procedure is also prescribed to detect effusion in the area of the synovial bursa. Manipulation allows you to determine whether the walls of the bag are fused.
- Puncture . If an effusion was detected in the synovial bursa, then the use of this diagnostic method is recommended. It involves taking the contents of the bag. Subsequently, bacteriological, cytological and microscopic examination is carried out. Also, this examination method makes it possible to determine the nature of inflammation. It can be hemorrhagic, serous or purulent.
Diagnostic measures should be used in combination, which will make it possible to determine the location of inflammation, as well as the degree of subcoracoid bursitis.
Symptoms and diagnosis
This disease has certain symptoms. Knowing them, it is much easier to determine the presence of pathology. But they will not give absolute certainty, since the similarity of symptoms has much in common with other diseases associated with damage to the upper extremities. Therefore, the disease should be treated under the strict supervision of doctors who are able to establish an accurate diagnosis.
The danger of the pathology occurring in the subacromial form of the initial stage is that at rest there is no pain, there is only slight tingling in the areas of pathology, and sometimes unpleasant twitching occurs. And only when raising the arms to chest level or higher, as well as when trying to move the arm back, does a person experience discomfort and limited mobility.
Since the disease occurs as a result of inflammation of tissues and their changes, one of the next signs of the disease is the appearance of edema and swelling of the affected area, which causes tissue hyperemia. All these signs are quite easy to detect, and preventing further development of the disease can be avoided by seeking qualified medical help. Negligent attitude towards the disease can lead to the development of a general increase in intoxication of the body and destruction of limb tissue.
Fortunately, the level of modern medicine allows us to diagnose and apply the correct therapy at all stages of the disease. Diagnosis consists of:
- examination by a doctor for the presence of inflammation and pain using palpation;
- collection of a puncture from the bursa, necessary to determine the presence of pathogenic microorganisms;
- blood analysis;
- radiography - carried out in order to determine the presence of a fracture or crack that has similar inflammatory processes;
- Ultrasound diagnostics – helps in visualizing pathology and its precise localization.
Drug and surgical treatment
In order to alleviate the patient’s condition as quickly as possible, he is prescribed complex therapy for bursitis. The sore shoulder should be at rest. If necessary, the patient is given a temporary splint. Pathology therapy is developed in such a way as to relieve pain and eliminate the inflammatory process. Thanks to this, the functionality of the hand is completely restored.
The use of bondage is one of the most effective ways to gently treat bursitis.
If the pathological process is mild, then therapy consists of the use of non-steroidal antiviral drugs. The use of ointments, physical therapy and compresses for bursitis is also recommended. Therapy of the pathological process is carried out using massage and physiotherapy. When the disease develops against the background of infection, bursitis is treated with antibiotics. The prescription of drug therapy is carried out in accordance with the nature and characteristics of the pathological process. For bursitis it is recommended to use:
- Antibiotics . The selection of a specific drug is carried out in accordance with the results of bacteriological examination.
- Painkillers . In most cases, patients are recommended to use medications that have a local effect. Experts recommend lubricating the affected area with Deep Relief, Finalgon, Apisatron, Diclofenac, which are produced in the form of creams and ointments for bursitis and are characterized by the presence of an analgesic effect.
- NVPD . From this group of drugs, the use of Zomepirac, Epirazole, Fenclofenac, Indoprofen, Meloxicam is recommended.
If the disease develops against the background of exposure to staphylococcus, then the use of Cefazolin, Dicloxacillin, Cephalexin is recommended.
In order to reduce the severity of pain and reduce the inflammatory process, the use of physiotherapeutic procedures is recommended. They also help improve tissue trophism. The choice of a specific therapeutic method directly depends on the stage of the pathology. In most cases, patients are prescribed:
- naftalan applications;
- high-intensity pulsed magnetic therapy;
- local cryotherapy;
- laser therapy;
- ultraphonophoresis, which requires the use of hydrocortisone;
- transcutaneous electroanalgesia.
Physiotherapy exercises are prescribed after the acute symptoms of the pathology have been relieved. With its help, the tendon-ligamentous apparatus is strengthened and the functions of the shoulder are completely restored.
To combat pain and inflammation, experts recommend massage. It should last no more than 15 minutes. To obtain the highest therapeutic effect, it is recommended to carry out 10 to 12 procedures. If conservative treatment is ineffective, surgical intervention is recommended. In this case, the affected synovial bursa in the shoulder joint is excised.
There are a large number of methods for treating bursitis, which allows you to choose the most appropriate option for the patient in accordance with his individual characteristics. To speed up the process of treating the disease, it is recommended to use several therapeutic methods simultaneously.
If the form of the disease is severe or complicated, then injectable glucocorticosteroids are taken, which have a prolonged effect.