The anterior cruciate ligament (lat. lig. cruciatum anterius) starts from the postero-superior part of the inner surface of the lateral condyle (bone protrusion) of the femur, crosses the cavity of the knee joint and is attached to the anterior part of the anterior intercondylar fossa of the tibia, also in the joint cavity. The cruciate ligament stabilizes the knee joint and prevents the tibia from moving excessively forward, and also supports the lateral condyle of the tibia. The posterior cruciate ligament of the knee joint (lat. lig. cruciatum posterius) starts from the anterosuperior part of the lateral surface of the internal femoral condyle, crosses the knee joint and attaches to the posterior intercondylar fossa of the tibia. It stabilizes the knee joint and keeps the lower leg from moving backward.
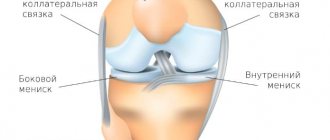
The articular surfaces of the bones are covered with cartilage. Between the articulating surfaces of the femur and tibia there are internal and external menisci, which are crescent-shaped cartilages. The knee joint is enclosed in a joint capsule. In humans, the knee joint allows movements of flexion and extension, and when bent, rotation around an axis.
The knee is the most common site of sports injuries (such as a torn meniscus or ligament).
Cruciate ligament injuries
Anterior cruciate ligament rupture can occur when a forward force is applied to the back of the knee joint while the shin is flexed and internally rotated. Ruptures of the cruciate ligaments may be accompanied by avulsion fractures of the bone plates at the attachment points of the ligaments or a fracture of the intercondylar eminence. Which makes subsequent treatment much more difficult. Very often, ruptures of the cruciate ligaments occur in athletes while playing football, while practicing alpine skiing, and in wrestlers. The posterior cruciate ligament is torn when the tibia is sharply extended at the knee joint or when there is a direct blow to the front surface of the tibia when it is bent at the knee joint.
Ligament ruptures are often combined. The most severe damage is considered to be ruptures of both cruciate, both lateral and joint capsules. This leads to laxity of the knee joint and loss of the ability to walk with that leg. When the cruciate ligaments rupture, sharp pain occurs. Bleeding occurs in the joint (hemarthrosis). The joint increases in size. The symptom of “balloting” of the patella is revealed. However, for some patients, the moment of injury itself may go unnoticed. Later, a feeling of instability and looseness in the knee joint appears.
Causes
The main cause of corresponding knee injury is excessive flexion or extension of the joint, as well as lateral mechanical forces. This injury may more often occur in athletes, especially those involved in contact (wrestling) or active (running, football, hockey) sports.
In everyday life, such a knee injury occurs in the winter season when there is ice, as well as when walking or running on an uneven surface with a sharp turn of the body. This injury also occurs in cases of direct impact with a blunt object to the knee area.
The main symptom of a torn cruciate ligament is the “drawer” sign.
Using special techniques, the doctor moves the patient’s lower leg forward or backward. When the anterior cruciate ligament ruptures, the tibia moves excessively forward - the “anterior drawer” symptom.
, and when the posterior cruciate ligament is torn, the tibia easily moves backward -
a symptom of the “posterior drawer”.
With old ligament tears, the “drawer” sign may become unclear due to the development of fatty tissue around the tear site, which partially stabilizes the knee joint. The diagnosis is confirmed by MRI examination.
REHABILITATION
Small tears of the medial or lateral collateral ligaments heal within 4-6 weeks. For more serious ligament ruptures, the rehabilitation period is extended to 2 months. A complete tear of the collateral ligament takes at least 3 months to heal, although surgery is sometimes required to restore the integrity of the ligament. Rupture of the lateral collateral ligament more often leads to the development of instability of the knee joint, which is an indication for surgical treatment. After suturing the collateral ligament, a dosed load on the operated leg is indicated, for which it is necessary to use crutches. After collateral ligament replacement, the load on the operated limb must be limited for 12 weeks after surgery. Many doctors prescribe patients to wear braces and knee pads to stabilize the knee joint.
Treatment of anterior cruciate ligament injuries
Conservative treatment of the cruciate ligament of the knee joint
In the acute period, i.e. immediately after an injury, treatment should be aimed at relieving pain and swelling of the knee joint, and later at restoring normal mobility in the joint. Immediately after an injury, do not attempt to move without assistance. You must protect your knee from further damage that may occur without proper treatment. Conservative treatment includes ice packs, anti-inflammatory medications, and rest. If hemarthrosis is present, it is necessary to suction out the accumulated fluid. Physiotherapy and exercise therapy may also be prescribed.
Physical exercise will help quickly restore normal mobility in the joint and prevent muscle atrophy. Specific exercises focus on strengthening the hamstrings and quadriceps muscles, which help stabilize the knee. An important argument in favor of treatment is the fact that long-term instability of the joint leads to early arthritis of the knee joint.
Knee pads - bandages, orthoses and supports.
Bandages are knitted products that fit tightly around a joint and improve its stability. They may have special silicone inserts for better fixation of the patella - in the form of a ring or half ring. An orthosis is an orthopedic device whose main task is to compensate for impaired joint functions. Orthoses are usually called complex structures made of metal, plastic and fabric, which are used for more serious disorders and better stabilize the joint (Fig. 1). Sometimes it is difficult to draw a clear line between a bandage and an orthosis, since there are bandages with side iron inserts in the form of elastic springs or simple hinges, which are additionally secured with Velcro. The word "support" comes from the English word support, which is translated as "support" and is used as a general term. Calipers are often used for knee instability. If you do not lead an active lifestyle, you can completely do without surgical treatment. The caliper will provide the necessary stability.
However, there is no evidence that the use of knee supports prevents the development of arthrosis of the knee joint. Using a caliper can give a false sense of security when playing sports. Calipers will not always be able to protect your joint completely, especially during sudden movements, stops and jumps. Therefore, in case of severe instability of the joint, surgical treatment is recommended for people leading an active lifestyle and playing sports. Many doctors recommend using calipers for at least a year after surgery. So if you have an injured cruciate ligament, you will need supports in any case.
Surgical treatment of anterior cruciate ligament rupture of the knee
If, after a course of conservative treatment, the stability of the joint does not meet the requirements of physical activity and the calipers do not provide the necessary stability of the joint, then it is proposed to resort to surgical treatment. Even when it is obvious immediately after an injury that surgery is necessary, most doctors prescribe a course of physical therapy and exercise therapy to quickly relieve swelling and restore full mobility to the joint. Only after this is surgery possible.
Surgical treatment for a torn anterior cruciate ligament involves arthroscopic reconstruction of the anterior cruciate ligament. Arthroscopy is a method of endoscopic surgery on joints. Operations are performed using very thin instruments and special optics connected to a digital video camera (Fig. 2). During the operation, the surgeon looks at the monitor and sees everything that is happening at the moment in the joint, with high magnification - from 40 to 60 times. The use of modern instruments and highly sensitive optics makes it possible to perform the finest manipulations on the knee joint with minimal damage to surrounding structures and the joint itself (for example, suturing or removing part of the menisci, cartilage transplantation, ligament reconstruction) - and all this through 2-3 small incisions. After such an operation, the patient is usually discharged on the same day.
To reconstruct the anterior cruciate ligament, leading sports medicine clinics currently use grafts that are pieces of human tissue. In world practice, several sources of graft are used: autograft from the patellar ligament, autograft from the hamstrings, allografts.
- Reconstruction from the patellar ligament.
This ligament connects the patella to the tibia. The autograft is cut off from the tibia and patella with bone fragments. Using the bone fragment, the autograft is subsequently fixed in the bone canal. This technique not only increases the strength of attachment of the graft to the new bed, but also ensures its faster fusion with the latter, since the fusion of spongy bone in a canal, the walls of which are represented by a spongy structure, requires 2-3 weeks, which is significantly less than the period of fusion of such a ligament or tendon with bone. The edges of the cut ligament are sutured. Channels are drilled in the tibia and femur bones, leading into the cavity of the knee joint. The internal openings of these channels in the joint are located in the same place where the attachment points of the anterior cruciate ligament to the articular surfaces of the femur and tibia were located. The ligament graft is passed into the joint cavity through the bone canal of the tibia. The ends of the prosthesis are fixed in the bone canals using special metal or biopolymer absorbable screws. This is the method most often used in most clinics around the world.
- Autograft from hamstrings.
Tissue from the semitendinosus tendon can be used as graft material. There is still no consensus on which autograft is best. Reconstruction with an autograft from the patellar ligament is more traumatic and recovery after such an operation is more difficult due to injury to this ligament. But it is believed that such an operation is more reliable. The knee is then more stable and can withstand loads better. Although, if the surgeon has well mastered the technique of performing reconstruction from the tendons of the semitendinosus and gracilis muscles, comparable results are obtained. With the second method of surgery (from the tendon of the semitendinosus muscle), fewer incisions are made and in the future it is almost invisible that a knee operation was performed. With the first technique (from the patellar ligament), an additional 5-centimeter scar will remind you of the operation, which in reality is not very noticeable, especially in men. Recently, preference has been given to semitendinosus autografts or the quadriceps tendon, but this technique The operation is not applicable in all cases; the patellar ligament is no less rarely used. This issue is approached individually. Allografts are tissue obtained from a donor. After a person dies, tissue is removed from the body and sent to a tissue bank. There she is checked for all infections, sterilized and frozen. When surgery is necessary, the doctor sends a request to the tissue bank and receives the necessary allograft. The source of the allograft may be the patellar ligament, hamstrings, or Achilles tendon. The advantage of this method is that the surgeon does not have to cut the graft from the patient's body, disrupting its normal ligaments or tendons. This operation takes less time, because no time is wasted on isolating the graft. Considering the complex structure and biomechanics of the anterior cruciate ligament, during the development of the surgical technique, the term “cruciate ligament reconstruction or plastic surgery” was rejected. Performing only one stage of the operation, namely the location of the graft in the joint cavity is similar to the course of the normal cruciate ligament, does not give grounds to call this surgical intervention restoration of the cruciate ligaments, since the structure of the ligament is not completely recreated, each portion of which plays a significant role in its effective functioning. Therefore, the term “restoration of stability” or “stabilization of the knee joint in one way or another” would be correct and theoretically justified.
x-ray examination
x-ray examination
- 1st degree – the integrity of the structures is preserved. Partial rupture of several fibers occurs (this degree of rupture is also called stretching).
- Grade 2 – a more severe rupture with a significant amount of damaged connective tissue fibers. In general, the anatomical relationship of the ligaments and their integrity are preserved.
- Grade 3 – severe injury with complete rupture of one or more ligaments. This severe injury is usually accompanied by damage to the meniscus of the knee or the articular processes of the femur, tibia or fibula.
Dividing the injury into severity levels is possible after an objective diagnosis with visualization of the tissues and structures of the joint.