Your orthopedist
Everything about the musculoskeletal system on one site: Back, Joints, Bones and more
Home › Joint diseases › Specific joint diseases › Lisfranc joint and Chopart joint: location, injuries, diseases, treatment methods
Many people, even those who know the anatomy of the human skeleton well, do not know such names as Lisfranc joint and Chopard joint. And this is not surprising. These joints are located in the foot area and are low-moving connections of a number of tarsal bones with nearby bones.
Does the arch of your foot hurt in a certain place? Possible damage (pathology) to the Lisfranc or Chopard complexes
The information, drawings, photos and videos in this article will help you get an idea of the anatomical structure of the Lisfranc and Chopard joints, typical injuries and diseases in these areas, as well as standard treatment protocols operated by a traumatologist or orthopedist.
- Anatomy of Chopart and Lisfranc joints
- Traumatology
- Treatment of traumatic injuries
- Orthopedics
Localization and structure
Chopart's joint is located in the tarsal region, closer to the ankle, and combines the talonavicular and calcaneal-cuboid joints. They are held in place by a strong bifurcated ligament that originates from the top of the calcaneus and encircles the scaphoidocuboid bony structures. This connective tissue is called "Chopard's key".
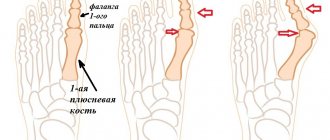
The anatomy of the Lisfranc joint includes the cuneiform and cuboid metatarsal joints, which are located toward the distal end of the foot. The joint formations strengthen the interosseous wedge-metatarsal ligaments, which unite the second wedge-shaped and metatarsal bones. This ligamentous device is called the Lisfranc key.
Complications
For the treatment of fractures and fracture-dislocations of the tarsometatarsal bones, traditional medicine recipes are not used. This kind of injury requires mandatory medical intervention, as it is necessary to set the bones in place so that the joint can recover normally. If a patient refuses hospital treatment and the foot recovers on its own, but the bones are in the wrong position, the patient has a 90% chance of remaining disabled and limping even after the bones have healed.
In addition, due to the displacement of the bones, the joint begins to fray and collapse, subsequently causing chronic pain. A deformed foot ceases to perform a normal shock-absorbing function, which leads to the destruction of the ankle, knee and hip joints.
With open injuries, the wound may become infected and suppurate; as a result, blood poisoning and other complications may occur. Open fractures require immediate hospitalization and surgical treatment.
If you consult a doctor in a timely manner, in most cases the disease can be cured without consequences for later life. Over time, the foot is completely restored and its function returns to normal. But it is worth remembering that the earlier treatment for fracture dislocation was started, the better the prognosis.
Why do pathologies of Chopart and Lisfranc joints occur?
Such movable joints of the foot experience a large load, since they support the weight of a person’s body during movement and in a standing position, they are most susceptible to injury and illness.
The Chopart and Lisfranc joints are the most traumatic movable joints of the foot.
The main causes of traumatic injuries and diseases of the musculoskeletal system (MSD) are the following factors:
- twisting the leg;
- jumping from heights;
- direct blow to the foot/feet on a hard object;
- playing sports where the main load falls on the lower limbs;
- professional activities associated with prolonged stay in the zone of vibration and shaking;
- lack of calcium in the body;
- bad habits and unhealthy diet.
Anatomy of the lower leg
The tibia is the part of the leg from the knee to the heel, consisting of two bones: the tibia (located medially), the fibula (located laterally) and the patella. These tubular bones have internal and external processes below. Between them is the interosseous space of the leg. The tibia is the thickest part of the lower leg, its body is triangular in shape with three distinct edges.
The fibula has almost the same length as the tibia, but is much thinner. The body of the bone is triangular, prismatic in shape, curved at the back and twisted along the longitudinal axis.
The foot is structured and functions as an elastic movable arch, the task of which is to create a certain elevation so that a person rests on individual points, and not on the entire foot. This anatomy of the foot allows you to avoid overstrain in the muscles and joints. Thanks to the vaulted structure, a person can walk upright.
Symptoms: how to recognize the disease?
Traumatic injuries
The most common injuries to the Chopart and Lisfranc joint are bruises, sprains, dislocations or fractures. Signs of various types of injury are given in the table:
| Type of injury | Symptoms | |
| Injury | Pain when pressed | |
| Swelling and hematoma | ||
| The functionality of the leg is preserved | ||
| Sprain | Severe pain, especially when moving | |
| Joint instability | ||
| Swelling | ||
| Dislocation and subluxation | Intense pain | |
| Edema and hematoma | ||
| Joint instability | ||
| Partial or complete loss of foot functionality | ||
| Fracture | Crack | Pain, swelling and swelling |
| Difficulty moving | ||
| Closed with offset | Loss of foot functionality | |
| Unnatural bone mobility where it should not be | ||
| Extensive hematoma | ||
| Often combined with dislocation (fracture dislocation) | ||
| Open | The bone breaks into fragments | |
| Violation of skin integrity by bone fragments and wound formation | ||
Bone diseases
The most commonly diagnosed are arthrosis, arthritis and osteoporosis. How ailments manifest themselves in the Chopart and Lisfranc joints is shown in the table:
| Disease | Symptoms |
| Arthrosis | My foot hurts a lot |
| Creaking or crunching | |
| Gait disturbance | |
| Severe foot deformity | |
| Arthritis | Strong pain |
| Joints are increased in size | |
| Swelling, puffiness, redness | |
| General deterioration | |
| Local and general increase in temperature | |
| Osteoporosis | Characterized by brittle bones and frequent fractures that occur without force |
Diagnostic features
After an injury, the patient should contact a surgeon or traumatologist at a clinic or a trauma center as quickly as possible. When examining the victim, the doctor collects complaints and medical history (fact of injury), and carefully examines the pathological symptoms. But in order to definitively establish the type of injury to the foot and, in particular, the Lisfranc joint, it is necessary to conduct additional research.
The most common and accessible is x-ray examination, which is carried out in 3 projections: direct, lateral and oblique, that is, at an angle of 30 degrees. If the displacement of bone structures is sufficiently pronounced, then the X-ray photographs clearly show the lines of fracture and separation of bone fragments, the expansion of interosseous spaces, and signs of inconsistency of bone surfaces with each other.
In these cases, diagnosis occurs quickly and reliably, but sometimes it can be difficult. In particular, diagnostic inaccuracies may be due to the overlapping shadows of the tarsal bones on each other, which can visually create a fracture line. To exclude these issues, it is necessary, for example, to also take an x-ray of the healthy foot and compare the data obtained.
X-ray examination remains the most important method for diagnosing injuries
Unfortunately, it is not possible to determine the type of ligament and tendon damage using X-rays, so computed tomography often becomes the next diagnostic step. This method allows you to “see” the smallest details of the injury that affected the bone, cartilage or soft tissue structures of the Lisfranc joint, as well as diagnose hidden injuries to the foot.
The success of therapy and, without exaggeration, the patient’s future life depend on the timeliness and correctness of the diagnosis.
If seeking medical help was late, if the injury is multiple and severe, if all therapeutic resources have not been used, then serious complications are very likely to develop after injuries to the Lisfranc joint. These include persistent foot deformity, arthrosis of a post-traumatic nature, and chronic pain syndrome.
Diagnostic methods
If a joint is damaged, you must contact a traumatologist.
Pathologies of the Chopart and Lisfranc joints are diagnosed by an orthopedist or traumatologist. The doctor collects anamnesis, conducts a visual examination and prescribes diagnostic procedures, such as:
- radiography;
- scintigraphy;
- arthroscopy;
- Ultrasound;
- computed tomography or magnetic resonance imaging;
- general and biochemical blood tests.
First aid
Fractures and dislocations of the foot require timely treatment, like any other fractures and dislocations. Therefore, if the foot is injured as a result of a collision with a car, or the fall of a heavy object, or under other circumstances, the first step is to fix it.
Immobilization of the injured limb
The victim is not recommended to stand on his sore leg on his own, to set the bones in place; he must call an ambulance, or take the patient to the hospital on his own.
Before placing the victim in a vehicle, it is imperative to immobilize the limb to prevent further displacement of the bones and deterioration of the condition.
To fix the leg, a splint is placed on it. If the fracture is open, you cannot remove anything from the wound and set the fractures yourself. Typically, the wound is covered with a loose sterile dressing or a clean handkerchief to protect it from dirt and infection. It is very important to give the victim pain relief so that during transportation the pain does not intensify and traumatic shock does not occur.
Treatment: which methods are effective?
Drugs
Traumatic injuries are treated with immobilization and the application of a cast, orthosis or splint. To relieve pain and inflammation, the following medications are recommended:
- "Diclofenac";
- "Dolobene";
- "Apizartron";
- "Deep Relief";
- "Longit."
For degenerative-dystrophic diseases, it is necessary to take chondroprotectors:
- "Dona";
- "Arthra";
- "Chondroxide".
The drug restores bone tissue.
If the Shopar and Lisfranc joints are affected by osteoporosis, calcium supplements should be used:
- "Calcium gluconate";
- "Calcemin";
- "Calcium D3 Nycomed";
- "Calcium-Vitrum".
All medications must be taken as prescribed by a doctor; self-medication is unacceptable. To restore foot mobility, you should attend sessions of physiotherapy, massage, manual therapy, water treatments, as well as do strengthening and restorative exercises daily. The degree of load on the foot should be determined by the doctor to avoid relapse of the disease.
Do you still think that it is impossible to cure your joints?
Judging by the fact that you are now reading these lines, victory in the fight against inflammation of cartilage tissue is not yet on your side...
Have you already thought about inpatient treatment? This is understandable, because joint pain is a very dangerous symptom, which, if not treated in a timely manner, can result in limited mobility. Suspicious crunching, stiffness after a night's rest, the skin around the problem area is stretched, swelling in the sore spot...
III.2.Specific goals for independent in-class topic development
III.1. The minimum basic level of knowledge and skills that are necessary to master the topic.
1) Describe the classification of SDS
2) Pathogenesis of diabetic polyneuropathy
3) Pathogenesis of diabetic osteoarthropathy
4) Pathogenesis of diabetic microangiopathy
5) Pathogenesis of diabetic macroangiopathy
6) Development of the wound process in patients with DFS
Arteries of the foot (according to Prives M.G.)
A.) 2-3 cutaneous arteries that branch in the skin of the dorsum and medial side of the foot;
B) the medial tarsal arteries extend to the medial edge of the foot;
B) lateral tarsal artery - extends to the lateral side and its end anastomoses with the arcuate artery;
D) arcuate artery, originates against the medial sphenoid bone, goes to the lateral side along the bases of the metatarsal bones and anastomoses with the lateral tarsal and plantar arteries; the arcuate artery gives off three aa anteriorly.
Metatarseaedorsales - the second, third and fourth, heading into the corresponding interosseous metatarsal spaces and each dividing into two aa. Digitales dorsales to the sides of the fingers facing each other; each of the metatarsal arteries gives off perforating branches, anterior and posterior, passing to the sole.
Oftena. arcuata is weakly expressed and is replaced by a.
metatarsealateralis, which must be taken into account when examining the pulse in the arteries of the foot during NK ischemia;
D) the first dorsal metatarsal artery is one of the two terminal branches of the dorsal artery of the foot, goes to the space between the I and II fingers, where it divides into two digital branches; but before division the branch gives off to the medial side of the thumb;
E) deep plantar branch, the second, larger of the terminal branches into which the dorsal artery of the foot is divided, goes through the first intermetatarsal space to the sole, where it participates in the formation of the plantar arch, arcus plantaris.
On the sole of the foot there are two plantar arteries - aa.Plantares medialisetlateralis, which represent the terminal branches of the posterior tibial artery.
The medial plantar artery (the thinner of the two) is located in the medial plantar groove. At the head of the first metatarsal bone, it ends, connecting with the first plantar metatarsal artery or flowing into the plantar arch; along the way it gives branches to adjacent muscles, joints and skin.
The lateral plantar artery (larger) goes in the lateral plantar groove, to the medial side of the base of the 5th metatarsal bone, where it turns sharply to the medial side and, forming an anterior convex arch on the bases of the metatarsals (arcus plantaris), ends on the lateral side of the 1st metatarsal bone by anastomosis with deep branches of the dorsal artery of the foot.
In addition, it gives a branch to the connection with the plantar medial artery.
Thus, the arteries of the sole, which experience constant pressure when standing and walking, form two arches, which, unlike the arches of the hand, are located not in parallel, but in two mutually perpendicular planes: in the horizontal - between the plantar medial and lateral arteries, in the vertical - between lateral plantar artery and branches of the deep plantar artery.
Periostitis of the metatarsal bone
The Lisfranc joint (articulationes tarsometatarseae) is formed by four joints: three wedge-metatarsal and one cuboid-metatarsal. External landmarks that determine the position of the joint space are: tuberositas ossis navicularis, tuberositas ossis cuboidei, base of the first metatarsal bone, tuberositas ossis metatarsalisv.
The interarticular space of the tarsometatarsal joint is defined along the entire length from the tuberosity of the fifth metatarsal bone to the base of the first metatarsal. You can feel the joint space by alternately flexing and extending each finger, and IV and V combined.
The Lisfranc joint gap is projected along a line running immediately posterior from the tuberosity of the fifth metatarsal bone to a point located 2 - 2.5 cm distal to the tuberosity of the scaphoid bone.
The first (internal) sphenoid-metatarsal joint is formed by the medial sphenoid bone and the base of the first metatarsal bone. The capsule is internally reinforced by the tibialis anterior tendon. On the plantar surface, the capsule is covered by the flexor pollicis brevis. The extensor pollicis longus tendon runs along the dorsal surface.
The second (middle) sphenoid-metatarsal joint is formed by the II metatarsal and middle sphenoid bones. Due to the fact that the medial and lateral cuneiform bones are located distal to the middle cuneiform, the second metatarsal bone, with its base, enters the space between these bones.
The third (external) sphenoid-metatarsal joint, formed by the external sphenoid and III metatarsal bones, is strengthened from the plantar surface by the initial part of the oblique head of the adductor pollicis muscle, and from the back by the muscle belly of the extensor digitorum brevis muscle.
“Surgical anatomy of the lower extremities”, V.V. Kovanov
The metatarsus consists of 5 metatarsal tubular bones, each toe except the big toe (2 phalanges) consists of three phalanges. The bones have some upward curvature, which allows them to participate in the formation of the arch of the foot.
The metatarsophalangeal and interphalangeal joints attach the phalanges of the fingers to the metatarsus. In addition to the thumb, the skeleton of each finger consists of a proximal, intermediate and distal phalanges.
The foot can withstand serious static and dynamic loads due to its anatomical structure and the presence of a large number of elastic elements.
Caused by inflammatory processes in the periosteum, developing against the background of excessive stress and injuries. Inflammation occurs in the outer and inner layers of bone, including the Chopart joint. People with flat feet and women who like to wear high heels suffer from the disease more often.
Hypoplasia of the metatarsal bones of the foot is characterized by the presence of a shortened forefoot. The deformity may be congenital or post-traumatic. In addition to the obvious cosmetic defect, there is pain and contracture of adjacent joints with subluxation in the metatarsophalangeal joint.