Haglund's disease (Haglund-Schinz) is a type of osteochondropathy. It is characterized by a violation of the ossification processes of the apophysis of the calcaneus. It is the most common cause of Achilles tendon pain in adolescents with increased physical activity.
The main cause of the disease is hereditary predisposition and repeated microtrauma of the growth plates of the heel bone. It appears in the form of a bone growth “bump” in the back of the heel bone.
Haglund's deformity can be either unilateral or bilateral.
Osteophyte of the calcaneus
An osteophyte (bone spur) that appears on the back of the heel bone slightly above the insertion of the Achilles tendon is called Haglund's deformity, named after the author who first described this disease. Haglund's disease is a fairly common cause of posterior calcaneal pain. The clinical diagnosis of the syndrome is most often confused with Achilles tendon bursitis and rheumatoid arthritis, since the clinical picture is quite similar in these pathologies. See symptoms below.
Anatomy of the heel region
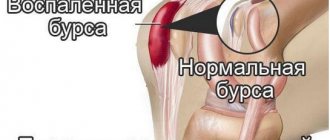
The calcaneus is the largest bone in the foot. The Achilles tendon, the largest and most powerful tendon in the human body, is attached to its tuberosity. By contracting the posterior calf muscles (gastrocnemius and soleus), the Achilles tendon pulls on the heel bone, allowing plantar flexion of the foot. This function allows us to walk, run, stand on our toes, and jump. Between the tubercle of the calcaneus and the Achilles tendon is the posterior calcaneal mucous bursa, which helps the tendon glide easily when the foot moves. Such bags are found in almost all joints, for example, in the elbow, shoulder, etc.
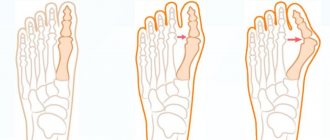
Pathogenesis of Haglund's deformity
During constant friction of the Achilles tendon, inflammation of the mucous membrane of the bursa begins. This chronic multi-month impact is transmitted to the posterior calcaneal tubercle and pathological cartilage slowly begins to form, changed, often with sharp spines. This can even be seen on an x-ray. The formation of this cartilage occurs due to the body’s protective reaction. The desire to strengthen the area of constant irritation and improve tendon gliding. But, unfortunately, pathological cartilage is not capable of this. It turns out to be a vicious circle.
The pressure on the bursa and Achilles tendon increases even more, which increases inflammation, pain and swelling. Inflammation of the mucous bursa and Achilles tendon without bone deformation is called achillobursitis (posterior calcaneal bursitis). Typically, bursitis precedes Haglund's deformity.
Patients do not pay much attention to the “bump,” thinking that it is a callus until it hurts. And as a rule, this condition is quite difficult to treat conservatively. This is why it is so important to see an orthopedist in the early stages of Haglund's disease.
Causes of Haglund's deformity
- High arches can contribute to Haglund's deformity because in a person with high arches, the heel bone is tilted posteriorly and the Achilles tendon rubs more against the normal heel tubercle, causing it to enlarge. Eventually, due to this constant irritation, the bursa and tendon become inflamed.
- Stiffness (decreased elasticity) of the Achilles tendon may also increase the risk of Haglund's deformity as it rubs more against the heel tuberosity. In contrast, a tendon that is more flexible results in less pressure on the posterior calcaneal bursa.
- Planovalgus foot deformity or varus deviation of the calcaneus changes the biomechanics of foot movement and increases the pressure of the Achilles tendon on the heel bone, triggering this pathological mechanism.
Classification of pathology
Schintz's disease has its own ICD-10 code in the category “Other osteochondropathy” - M93.
There is Haglund's deformity - a chronic enlargement of the posterior-superior and lateral part of the heel, which periodically reminds itself of pain. With Haglund syndrome, severe pain occurs due to inflammation of the retrocalcaneal bursa, the Achilles tendon. This condition can develop without bone growth.
Schinz's disease can be unilateral or bilateral, depending on the spread of the pathological process to one or two limbs. What is Schinz's disease in children? Let's consider the stages of osteopathy of the apophysis of the calcaneal tuberosity:
- Problems of local blood supply lead to disruption of tissue nutrition and aseptic necrosis;
- Due to the accumulation of dead tissue, the heel area is pressed through, forming an impression fracture;
- The affected area of the bone crumbles into fragments - a process called fragmentation;
- Dead tissue is dissolved;
- During repair, new connective tissue appears on the affected area, which will be replaced by new bone.
Symptoms of Haglund's deformity
Haglund's deformity itself can occur without pain and inflammatory symptoms. Only pathological exostosis (bump on the heel) is noted on the back of the heel. The deformity usually does not cause any problems with foot function. But in most cases, the deformity is accompanied by inflammation of the mucous bursa and tendon sheath, and swelling. Then patients experience pain when walking, and sometimes at rest.
The syndrome can occur on one or both feet.
Signs and symptoms of Haglund's deformity include:
- A noticeable bump on the back of the heel;
- Pain in the area of the Achilles tendon;
- Swelling, calluses on the back of the heel area;
It is pain that forces the patient to see a doctor.
The most important
Haglund's deformity is not only a cosmetic defect, but also a serious pathology that can lead to serious complications. The appearance of an osteophyte on the back of the heel inevitably leads to inflammation of the synovial bursa and damage to the Achilles tendon.
When the first symptoms occur, you must contact the clinic where treatment will be prescribed. At first, it may be conservative, but when the inflammatory process begins, doctors are inclined to remove the growth surgically, since drug treatment threatens relapses.
Diagnosis of Haglund's deformity
Diagnosis begins with a patient interview and a detailed physical examination. Be sure to look at the back of the heels to make sure there is no heel varus (heel pointing inward).
In case of varus deviation of the calcaneus, a certain surgical technique is used - corrective osteotomy. Standard surgical methods will not exclude the possibility of relapse (recurrence of the disease). Usually the diagnosis is obvious without additional diagnostic methods. But radiographs must be taken to rule out other causes of heel pain.
In controversial situations, magnetic resonance imaging (MRI) is used to rule out a disease called achilles tendinitis, which is similar in symptoms. For example, after injuries to the Achilles tendon, a dense scar (in the form of a lump) appears at the site of injury and, as a rule, it is painful. It can be confused with Haglund's deformity if the patient does not remember the moment of injury.
Diagnostics basic research methods
The most clear diagnosis is observed with an X-ray or MRI examination.
Since the growth is not initially accompanied by pain, people whose growth has already reached its full size consult a doctor. The doctor conducts an anamnesis and physical examination. To make a diagnosis, doctors use:
- X-ray;
- MRI.
More often, the disease is easily determined visually, since external changes begin immediately, without pain or inflammation. By excluding hereditary predisposition and possible injury, the main cause of the disease is determined. MRI is used in controversial situations when it is not possible to determine the extent of the lesion, and X-ray images do not show the whole picture of bone and soft tissue deformation. A timely visit to a doctor will avoid complications; moreover, treatment in the early stages is more effective and will not require surgical intervention.
Conservative treatment
If Haglund's disease is accompanied by pain, then the first step is to relieve inflammation from the affected mucous membrane of the bursa and Achilles tendon:
- During an exacerbation, wear shoes with a soft back or without a back (clogs);
- Local use of anti-inflammatory analgesic ointments (for example: dolobene gel, voltaren, traumeel);
- Taking non-steroidal anti-inflammatory drugs (for example: ketonal, nurofen, nise);
- Physiotherapeutic methods: magnetotherapy, laser therapy, shock wave therapy (SWT)
- Wearing an ankle orthosis that limits movement.
These simple and widely available methods will allow you to return to normal walking as quickly as possible.
We do not recommend injecting hormonal anti-inflammatory drugs, in particular Diprospan, into the area of inflammation, as this greatly increases the risk of tendon rupture.
Surgery
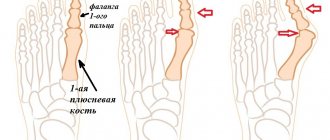
If conservative methods of treating Haglund's deformity are ineffective, surgical treatment is performed using various techniques, which depend on the shape and degree of the deformity. The goal of most surgeries is to remove bony exostosis at the back of the heel to relieve pressure on the bursa and Achilles tendon. Inflamed, swollen tissues will return to normal volume when the pressure is removed.
If the clinical picture is dominated by pain, swelling, and inflammation of the calcaneal structures, then in addition to resection (cutting off) of the exostosis, the mucous bursa is removed. Because it will continue to hurt even after surgery.
Removal of exostosis (spurs) of the heel bone. This operation can be performed under conduction or local anesthesia in an open traditional way through a small (4-5 cm) incision outward from the Achilles tendon, or minimally invasively through 2 5 mm incisions using video endoscopic technology.
- Open method.
During the operation, the Achilles tendon is moved medially (inward) with instruments to eliminate the possibility of damage. Next, the exostosis is cut off with a medical saw. Sharp edges are cleaned by cutting with side sharpening. If necessary, the mucous bursa is excised. The wound is sutured and a sterile dressing is applied. - Endoscopic method.
As a rule, patients move in an orthosis for the first week to reduce mobility of the foot and, consequently, swelling, pain, and hematoma.Wedge-shaped osteotomy of the calcaneus.
This method of surgical treatment of Haglund syndrome is used if the patient has a high arch of the foot and, as a result, the angle of the heel bone is greater. It follows from this that the pressure of the posterior calcaneal tubercle on the Achilles tendon will be greater. To do this, the surgeon cuts out a wedge during the operation in the posterior part of the heel bone and fixes it with titanium screws, as shown in the diagram. This results in a relative decrease in the angle and the tubercle no longer exerts strong pressure on the tendon.
- Corrective osteotomy of the calcaneus.
This is the third type of operation - elimination of varus deviation of the calcaneus.
After operation
As a rule, during the first week after surgery for Hoogland's deformity, patients move independently, limiting the load on the operated leg, but sometimes crutches are required. In the early postoperative period, anti-inflammatory painkillers and antibiotics are prescribed. Dressings are carried out until the wound heals. Physiotherapy can be performed from the first day after surgery. These methods can reduce swelling and pain after surgery. Typically, 10 sessions of magnetic therapy and laser therapy are prescribed. Stitches are usually removed between 10 and 14 days. Sometimes the suture is removed intradermally with absorbable sutures. In this case, there is no need to remove anything. Complete rehabilitation takes place in 4-6 weeks with the first type of operation (removal of exomtosis). For the other two types of surgery, recovery may take 2-3 months. While the heel bone is healing.
Rehabilitation
In most cases, during the first 7 days, operated patients move with crutches, limiting the load on the leg. To reduce inflammation or prevent its development, the doctor prescribes an antibiotic and NSAIDs, and junior medical staff regularly perform dressings to speed up the healing of the wound surface. To improve the patient’s condition, doctors recommend physiotherapeutic procedures, such as:
- magnetic therapy;
- laser therapy.
The course of treatment with this method is at least 10 procedures. The stitches are removed after 1.5 weeks. If absorbable threads were used, then this is not necessary. If the operation is performed openly, then rehabilitation takes no more than 1.5 months, and in more severe cases it can take up to three months, until the heel bone has completely fused.
Prevention of Hoogland's deformity
- Wearing shoes with soft backs.
- Use shoes with 2-4 cm heels for high arches.
- If you have flat feet or planovalgus deformity, you need to wear custom orthopedic insoles every day.
Don't self-medicate!
Only a doctor can determine the diagnosis and prescribe the correct treatment. If you have any questions, you can call or ask a question by email.
| Correction of Haglund's deformity | Price, rub |
| Removal of calcaneal osteophyte | from 34 000 |
| Conduction anesthesia | from 3 000 |
| Dressing, suture removal | from 500 |
| Laser removal of bunions | To the list of articles | Taylor deformation |
Prevention of pathology
To prevent the development of pathology, doctors advise following a number of recommendations. Prevention includes:
- performing a set of special exercises with alternating load and rest regimes;
- children are prohibited from lifting heavy objects;
- overwork must be avoided;
- rational balanced diet (more nuts, greens, vegetables and fruits, reduced consumption of flour and sweets);
- taking vitamins and minerals in courses, most often in the form of complex supplements - Complivit, etc.;
- maintaining a healthy lifestyle (giving up bad habits, daily routine, proper sleep);
- if you have flat feet, you need to purchase special orthopedic insoles;
- limiting the wearing of high-heeled shoes (some doctors recommend abandoning stiletto heels and wearing shoes with heels no higher than 4 centimeters);
- use of foot baths.
Following these tips allows you to reduce the risk of developing pathology, the likelihood of relapse of inflammation and avoid the reappearance of growths.