Occipital neuralgia is a condition that causes damage to the nerves that arise from the top of the spinal cord and run upward under the scalp in the occipital region. The result is pain.
Our expert in this field:
Lashch Natalia Yurievna
Neurologist of the highest category, candidate of medical sciences, associate professor. Laureate of the Moscow City Prize in the field of medicine.
Call the doctor Reviews about the doctor
Why does the disease occur?
Possible causes of occipital neuralgia:
- Acute injury to the back of the neck and head.
- Constant tension in the neck muscles. For example, office workers who spend most of the day sitting at a computer.
- Protrusions and herniations of cervical intervertebral discs.
- Osteochondroma (benign tumor) of the vertebrae.
- Infectious diseases and inflammatory processes.
- Diabetes.
- Gout.
- Multiple sclerosis.
- A rare cause is metastasis of malignant tumors to the spine.
Sometimes the doctor is never able to fully understand why the disease occurred.
We will call you back
Message sent!
expect a call, we will contact you shortly
Causes of cervical radiculopathy
Any condition that somehow compresses or irritates a nerve root in the cervical spine can cause cervical radiculopathy.
The most common reasons are:
- Disc herniation. If the internal material of the intervertebral protrudes and irritates the nearby root in the cervical spine, then the development of radicular syndrome (cervical radiculopathy) is possible. If a young person (20 or 30 years old) has cervical radiculopathy, the most likely cause is a herniated disc.
- Cervical spinal stenosis. As part of the degenerative process of the cervical spine, changes in the spinal joints can result in decreased space in the spinal canal. Spinal stenosis is a common cause of cervical radicular syndrome symptoms in people over 60 years of age.
- Osteochondrosis (degenerative disc disease). As discs in the cervical spine degenerate, the discs become flatter and stiffer and do not support the spine. In some people, this degenerative process can lead to inflammation or damage to a nearby nerve root. Cervical degenerative disc disease is a common cause of radiculopathy in people over 50 years of age.
- Cervical radiculopathy may be caused by other conditions that put pressure on the nerve roots or cause damage to the cervical nerve roots, such as tumors, fractures, infections or sarcoidosis, synovial cyst, synovial chondromatosis of the facet joints, giant cell arteritis of the radicular vessels.
- Factors associated with an increased risk of developing cervical spine syndrome include: heavy manual labor requiring lifting more than 10 kg, smoking, and long periods of driving or working with vibrating equipment.
Symptoms of occipital neuralgia
The main manifestation of the disease is headaches. They occur in the back and top of the head, at the base of the skull, and in the neck. Pain may spread to the eyebrows and behind the eyes.
Usually the pain resembles strong injections or electric shock. It can be pulsating, shooting, accompanied by a burning sensation. In some patients, sensitivity to light and sounds increases. Pain can be caused by movements in the neck.
Typically the pain begins in the neck and lower part of the head and spreads upward. Most often it occurs on one side, but the occipital nerves can be affected on both sides.
Chronic headaches occur due to various diseases. Often, people who experience symptoms of occipital neuralgia (and even their doctors) believe that they have tension headaches or migraines.
Anticonvulsants in the treatment of neuropathic pain
About 20% of cases of chronic pain are neuropathic pain, which reduces the quality of life of patients, their ability to work, their ability to socially adapt, and in many cases is difficult to treat.
This indicates the high social and medical-economic significance of the problem of diagnosis and treatment of neuropathic pain. According to the modern pathophysiological classification of pain syndromes, based on the identification of the main mechanism of pain formation, neuropathic pain, as defined by the International Association for the Study of Pain (IASP), is caused by primary damage or dysfunction of the structures of the peripheral or central nervous systems that provide pain signals. Thus, neuropathic pain is based on pathological activation of pain pathways, which may be associated with damage or dysfunction of the nervous system at the level of the peripheral nerves and dorsal roots (peripheral neuropathic pain) or the spinal cord and brain (central neuropathic pain). Typical examples of peripheral neuropathic pain associated with peripheral nerve damage are painful diabetic neuropathy and neuroma pain, and when nerve roots are affected, discogenic radiculopathy and postherpetic neuralgia. Central neuropathic pain develops, for example, with damage to the spinal cord in patients with traumatic injury and syringomyelia, with brain damage in patients with multiple sclerosis and after a stroke. It should be noted that the issue of criteria for including specific pain syndromes in the category of “neuropathic pain” continues to be discussed. There is a point of view that only cases with proven damage or pathology of nociceptive structures can be classified as neuropathic pain. Studies conducted in various countries have shown that neuropathic pain occurs in 6-8% of the population. Risk factors for the development of neuropathic pain are chronic pain syndromes, as well as female gender, older age of patients and low level of social status. Neuropathic pain is associated with greater pain intensity and frequent visits to medical care and is caused by a wide range of injuries, diseases and dysfunctions of the peripheral and central nervous system, of which the most famous and widespread are painful diabetic polyneuropathy and postherpetic neuralgia.
Clinical variants of neuropathic pain:
1. Lesions of the peripheral nervous system:
- traumatic nerve damage (including iatrogenic damage during surgery);
- ischemic neuropathies;
- nerve compression;
- polyneuropathies (hereditary, dysmetabolic, toxic, inflammatory, infectious, paraneoplastic, with amyloidosis and vasculitis);
- compression of the nerve root (radiculopathy);
- postherpetic neuralgia;
- neuralgia of the trigeminal and glossopharyngeal nerves;
- neuropathies associated with cancer (polyneuropathy caused by chemotherapy and radiation therapy, nerve invasion by a tumor);
- complex regional pain syndrome.
2. Lesions of the central nervous system:
- post-stroke pain syndrome;
- multiple sclerosis;
- spinal cord injury;
- syringomyelia;
- volumetric formations of the brain and spinal cord;
- epilepsy.
Diabetic polyneuropathy is observed in approximately 50% of patients with diabetes, while neuropathic pain is observed in 11-24% of patients with polyneuropathy, which depends on the duration of the disease with diabetes and polyneuropathy, as well as the type of diabetes. The frequency of herpetic lesions ranges from 10 to 20% in the population, and in these patients, postherpetic neuralgia is observed in 15-22% of patients. Neuropathic pain is most often observed in patients with traumatic injury to the spinal cord and in cases of spinal cord injury in cases of syringomyelia.
Clinical manifestations of neuropathic pain, regardless of the level of damage and the etiological factor, are characterized by spontaneous (stimulus-independent) and caused by various stimuli in the patient’s daily life or when examined by a doctor (stimulus-dependent) pain. The occurrence of spontaneous and stimulus-dependent pain is associated with various mechanisms of changes in excitability, transmission of pain stimulus and inhibition of excitation in the nociceptive system.
With peripheral damage to nociceptive fibers, the mechanisms of pain syndrome formation may be associated with changes in the excitability of pain receptors, which leads to their activation even with low-threshold stimuli, which is not observed under normal conditions. Thus, pain afferentation increases, which subsequently leads to a change in the excitability of nociceptive neurons of the dorsal root ganglion and dorsal horn. The main mechanisms explaining the increase in excitability of nociceptive fibers of the peripheral nerve under pathological conditions are the formation of new ion channels, which are the source of ectopic activity of peripheral nerves with the development of pain, and the emergence of the possibility of transferring excitation from one fiber to another - the phenomenon of ephaptic excitation. With mechanical damage to the nerve, the formation of neuromas is possible, which is the result of compensatory reinnervation (sprouting), which can be a source of pathological nociceptive afferentation.
The dorsal horn of the spinal cord is the center of modulation of the normal pain signal and is where the “pain gate” opens or closes. In this regard, the changes that occur in the dorsal horn under pathological conditions are largely decisive for the development of neuropathic pain. Random excess afferentation along Aδ- and C-fibers leads to increased excitability of nociceptive neurons of the dorsal horn (central sensitization) with the development of the inflation phenomenon, when in response to one painful stimulus the neuron responds with a burst of impulses. Increased excitability of dorsal horn nociceptors is associated not only with excessive constant nociceptive afferentation, but also with the fact that prolonged depolarization causes activation of glutamate NMDA receptors (N-methyl-D-aspartate). Activation of NMDA receptors leads to the entry of calcium and sodium ions into the neuron, which causes a further increase in its excitability. The formation of neuropathic pain is associated not only with glutamate activity, but also with a decrease in GABA-mediated inhibitory effects on nociceptive neurons and a decrease in the content of active opioid receptors in the dorsal horn.
Nociceptive signals from dorsal horn neurons travel to the thalamus opticum and then to the somatosensory cortex, where pain is perceived. Neurons of central sensory structures can also change their excitability with the formation of the phenomenon of sensitization. All central structures for the conduction and perception of pain have close connections with descending inhibitory and activating pathways. The main inhibitory (antinociceptive) influences are associated with descending pathways from the periaqueductal gray matter and the rostro-ventral parts of the medulla oblongata to the dorsal horn. These descending inhibitory influences are realized through the norepinephrine and serotonin neurotransmitter systems.
In clinical practice, diagnosing the neuropathic nature of pain is often difficult. The experience of pain is always subjective, it cannot be accurately measured, and there are no absolute criteria to distinguish neuropathic pain. Judging the pathophysiological mechanisms underlying the pain syndrome can only be tentative, based on the characteristics of pain, data from a neurological examination and the results of a neurophysiological study. Moreover, the identification of clinical signs and changes in electrophysiological parameters showing a pathological change in the state of the nociceptive system does not reliably prove the presence of neuropathic pain. Neuropathic pain can occur immediately after damage to the nociceptive system, for example, in acute small fiber neuropathy in diabetes mellitus, or it can develop years or even decades after the damage, for example, in post-stroke pain.
The neuropathic nature of pain can be diagnosed if a dysfunction of the nociceptive system is confirmed in the presence of: 1) spontaneous sensory symptoms; 2) the results of a clinical examination identifying symptoms of damage to the nervous system: positive neuropathic symptoms (stimulus-dependent pain) and negative neuropathic symptoms (neurological deficit); 3) data from neurophysiological studies (EMG, quantitative sensory testing, somatosensory evoked potentials). In this case, the choice of research methods is determined by the results of a neurological examination.
One of the most important positive symptoms of neuropathic pain is allodynia, the identification of which during examination serves as a strong argument in favor of the neuropathic nature of the pain. Allodynia is a painful sensation that occurs when a stimulus of a non-painful modality is applied. Patients with allodynia often complain of pain associated with the touch of clothing or bedding to the area where allodynia is localized. Hyperalgesia, an increased pain response to a normal painful stimulus, is a quantitative change in the pain signal. It, like allodynia, is typical of neuropathic pain, especially in cases of chronic pain syndromes. A special variant of hyperalgesia is hyperpathy, in which, after the application of a painful stimulus, there is an increased perception of pain, while the pain continues and can even intensify within a few seconds after the cessation of painful stimulation.
Neurological symptoms make it possible to determine the presence, extent and localization of damage to the nervous system. To diagnose the phenomenon of neuropathic pain, the doctor must first assess the state of the sensory system. Depending on the peripheral or central localization of the pathological process, a study of the general neurological status, including the motor and autonomic systems, is of great importance for diagnosis; in this case, negative symptoms will include, for example, decreased reflexes, muscle strength, the presence of muscle atrophy, dryness and changes skin coloring. When identifying damage to the sensory system, to diagnose neuropathic pain, they focus on the state of sensitivity associated with the activation of thin, weakly myelinated Aδ fibers (response to cold stimuli and blunt prick) and thin unmyelinated C-fibers (response to painful and thermal stimuli). It should be remembered that neuropathic pain usually occurs in the area of decreased or lack of sensitivity, i.e. the zone of pain and sensitivity disorders in these cases coincides.
Treatment of neuropathic pain is based on modern ideas about the pathophysiological mechanisms of its development. Pharmacological interventions are used aimed at reducing peripheral afferentation, which supports changes in the excitability of nociceptive structures of the spinal cord and brain, drugs that reduce the excitability of nociceptive neurons, and drugs that enhance supraspinal descending inhibitory antinociceptive effects. In severe cases, administration of pharmacological drugs close to the central receptors (intradural) is used. It is possible to use electrical stimulation of peripheral nerves, primarily proprioceptive fibers, to enhance the inhibitory effects on the excitability of nociceptive neurons of the spinal cord and acupuncture. Surgical treatment for cases refractory to pharmacotherapy may include the use of electrodes implanted in the brain or spinal cord, nerve release or decompression, chemical destruction, or nerve transection. The table presents European recommendations for the treatment of neuropathic pain, based on an analysis of a database of controlled trials dating back to 1966.
The administration of local anesthetics leads to a reduction in neuropathic pain, especially in cases where its development is primarily due to pathological changes in the peripheral nerves. At the same time, drugs, due to absorption and systemic effect, can affect upstream nociceptive structures. The most widely used of all local anesthetics is lidocaine, which has an inhibitory effect on sodium channels. When 5% lidocaine is applied cutaneously using a patch, its absorption is minimal, the effect on other structures is not manifested and, accordingly, there are practically no possible systemic side effects. Thus, its use is justified for neuropathic pain accompanied by allodynia. The duration of pain and allodynia reduction with cutaneous application of lidocaine ranges from several hours to several days.
The clinical effect of intravenous administration of lidocaine in the form of a 5% solution has been confirmed in many types of neuropathic pain, for example, in painful diabetic polyneuropathy. It is interesting that the duration of the period of reduction or disappearance of pain in this case ranges from one to several weeks, which significantly exceeds the time of elimination of the drug. However, significant inconveniences of using intravenous lidocaine include the need to carry out treatment in an intensive care unit under constant ECG monitoring, because Cardiac side effects are possible.
Capsaicin - a cream that contains red pepper in a concentration of 0.025 or 0.075%, has the ability to activate the synthesis and release of a specific algogen - substance P, both in skin nociceptors and when the active substance is transferred by axonal current, in neurons of the dorsal ganglion and even the dorsal horn . The drug is applied to the skin at the site of pain, which initially leads to an increase in pain intensity, but then the pain decreases due to the depletion of substance P. The drug is recommended for use in cases of peripheral genesis of neuropathic pain and a small area of its localization. The main disadvantages of capsaicin treatment are the frequently occurring very intense pain syndrome with allodynia, which patients are unable to tolerate.
In cases of sympathetically supported pain, transdermal use of clonidine, a drug that has the effect of an α2-adrenergic receptor agonist, is possible, and both local and systemic effects of the drug on overlying sympathetic formations are possible.
Anticonvulsants and tricyclic antidepressants have an undoubted effect on the peripheral mechanisms of neuropathic pain, but the basis of their analgesic effect in neuropathic pain is still other mechanisms.
Nonsteroidal anti-inflammatory drugs that reduce peripheral inflammation are not used to treat neuropathic pain due to their ineffectiveness. However, their use is justified in cases of a combination of nociceptive and neuropathic pain, for example, with back pain, or with CRPS, where peripheral inflammation plays an important role in the development of the pain syndrome.
Ketamine, the main drug of the group of NMDA receptor blockers, was developed as a dissociative anesthetic and later began to be used in small doses for the treatment of neuropathic pain of various etiologies, incl. for cancer pain. The main mechanism of action of ketamine is the blocking of NMDA receptor ion channels in the dorsal horn of the spinal cord. Thus, ketamine reduces the excitability of nociceptive neurons, in particular reducing the winding phenomenon. It can be administered parenterally, intravenously, or orally. Clinical studies have shown the effectiveness of ketamine for postherpetic neuralgia, postoperative pain, as well as for central neuropathic pain (post-stroke, pain after spinal cord injury). Several studies have shown that ketamine enhances the effects of opioids (morphine) in cancer pain. The main disadvantage of the drug is the pronounced side effects of its use, which may be due to the additional effect of ketamine on opioid and muscarinic receptors, sodium and potassium channels and inhibition of serotonin and dopamine reuptake. More than 40% of patients receiving ketamine reported psychotomimetic effects, including hallucinations.
Currently, antidepressants are most widely used in the treatment of neuropathic pain of various etiologies. Tricyclic antidepressants (TCAs), which began to be used in the 50s. last century, primarily amitriptyline, are highly effective for neuropathic pain.
In diabetic painful polyneuropathy, TCAs reduce pain or lead to its disappearance in more than 80% of cases. The main mechanism of their action is blocking the reuptake of norepinephrine and serotonin into the presynaptic terminal due to the effect on sodium and calcium channels, which leads to increased activity of central antinociceptive structures, dependent on noradrenergic and serotonergic neuromediation. Selective serotonin reuptake blockers (paroxetine, fluoxetine) do not act on postsynaptic receptors, and therefore have fewer side effects, but they are significantly inferior to TCAs in their ability to reduce neuropathic pain. Amitriptyline has been studied in numerous controlled studies for postherpetic neuralgia and painful diabetic polyneuropathy, the most common forms of neuropathic pain, and its effectiveness does not require further research. The standard dose of amitriptyline to start treatment with is 25 mg, then it can be increased to 75-150 mg. TCAs are limited in use for neuropathic pain, especially in elderly patients, due to the onset of numerous and sometimes severe side effects: orthostatic hypotension, urinary retention, constipation, tachycardia, “sicca syndrome”. Contraindications for the use of TCAs are glaucoma and prostate adenoma. In addition, it has been proven that long-term use of TCAs increases the risk of myocardial infarction by 2.2 times.
Additional disadvantages of amitriptyline include nonlinearity of pharmacokinetics, i.e. when taking small doses, the concentration of the substance in plasma may be greater than when taking large doses. In this regard, the need arose to create new highly effective drugs that do not have such pronounced side effects. Recently, the so-called balanced norepinephrine and serotonin reuptake inhibitors with fewer side effects. The drug in this group, duloxetine, is used in the United States to treat neuropathic pain in diabetic polyneuropathy and other forms of chronic pain. However, it should be noted that duloxetine is still inferior to amitriptyline in the effectiveness of reducing neuropathic pain.
Anticonvulsants began to be used to treat pain syndromes in the 40s. last century, when the effectiveness of phenytoin (diphenin) in the treatment of trigeminal neuralgia was shown. In 1962, the anticonvulsant carbamazepine (finlepsin), a drug similar in structure to TCAs, was first used to treat trigeminal neuralgia, which to this day remains the first-line drug in the treatment of this variant of neuropathic pain. The main mechanism of action of phenytoin and carbamazepine is the blocking of voltage-dependent sodium channels, i.e. they have a peripheral mechanism of action. The main direction in the development of first-generation drugs is the creation of drugs that are similar in structure, have similar effectiveness, but fewer side effects, incl. hepato- and nephrotoxicity. A typical example of such a new drug is oxcarbazepine (Trileptal), which is similar in structure to carbamazepine.
The most effective drug for the treatment of neuropathic pain of various etiologies has proven itself to be a new generation of anticonvulsants - gabapentin (tebantin). The latest generation of anticonvulsants have a wider spectrum of action, which ensures their effectiveness in treating neuropathic pain.
Gabapentin is similar in structure to gamma-aminobutyric acid (GABA), but it does not interact with GABA receptors. Tebantine reduces the sensitization of central nociceptors, mainly due to binding to the α2δ subunit of voltage-gated calcium channels in the membrane of nociceptive neurons, which leads to blocking of the channels and a decrease in neuronal excitability. In addition, gabapentin retains a blocking effect on sodium channels and additionally has a stimulating effect on the synthesis and release of GABA. The drug has few side effects. In a study of 2216 patients, drowsiness was observed in 15.2%, dizziness in 10.9% and ataxia in 6.0% of patients, but the severity of side effects was insignificant, and their duration did not exceed 2-3 weeks. even if you continue to take the drug. The drug is not metabolized in the liver and is excreted as a whole molecule through the kidneys, but should be used with caution in patients with impaired renal function.
The effectiveness of tebantil has been shown in double-blind, placebo-controlled studies in cases of neuropathic pain in patients with diabetic polyneuropathy, postherpetic neuralgia, trigeminal neuralgia, and multiple sclerosis. In 2002, a controlled study examined the effectiveness of gabapentin for post-amputation phantom pain in 19 patients and showed that taking the drug at a dose of 2400 mg for 6 weeks. statistically significantly reduced the severity of pain compared to the placebo effect. In these studies, gabapentin was prescribed to men and women aged 20 to 90 years with a wide range of neuropathic pain syndromes caused by various diseases and lesions of the peripheral and central nervous system, and was shown to be effective and well tolerated with minimal side effects. Based on these studies, a drug dose titration system was created to reduce the frequency and severity of side effects, and the maximum possible doses of its administration were determined. Gabapentin is prescribed starting with a dose of 300 mg per day (evening, at night), then the dose is increased to 600 mg (300 mg during the day and 300 mg in the evening) and finally the dose is increased to 900 mg (300 mg 3 times a day). While taking the drug at a dose of 900 mg per day, the dynamics of the pain syndrome are analyzed, and if there is no effect, it is increased to 1800 mg/day. (increasing by 300 mg/day). The maximum doses of gabapentin in some studies that showed high effectiveness of the drug in the treatment of neuropathic pain reached 2700 or 3600 mg. Moreover, most researchers noted a decrease in pain syndrome in various types of neuropathic pain already in the first week of treatment with gabapentin. The drug has high (more than 60%) bioavailability, maximum plasma concentration is achieved 2-3 hours after taking the drug. Eating food does not affect the pharmacodynamics of gabapentin.
The appearance of tebantine has significantly increased the capabilities of doctors in the treatment of neuropathic pain syndrome, because When the drug is prescribed, pain is relieved in most patients, the effect occurs quickly, there are no significant side effects, and if necessary, it can be taken for a long period. With regard to other new generation anticonvulsants - topiramate, lamotrigine - it is necessary to clarify that although some controlled studies have shown their effectiveness in the treatment of neuropathic pain, they are not registered in Russia as drugs for the treatment of pain.
Among the new anticonvulsants whose effectiveness in the treatment of neuropathic pain has been studied in recent years, pregabalin (Lyrica) attracts attention. There were 10 double-blind, placebo-controlled studies involving almost 10,000 patients, mainly with painful diabetic polyneuropathy and postherpetic neuralgia. As a result, it was shown that the drug, which is similar in structure to GABA, is highly effective in treating neuropathic pain. Also important is the lower frequency of administration (2 doses per day) and the lower dose of the drug compared to gabapentin (from 75 to 600 mg), which leads to a decrease in the severity of side effects. Otherwise, the drug has the same advantages as gabapentin, i.e. rapid onset of effect (after the first 3 doses), a small number of side effects, the possibility of long-term use, no interaction with other drugs and independence from food intake.
Source: Medical Council magazine No. 3-4 2008.
Diagnostics
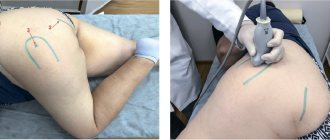
During the appointment, the neurologist asks the patient about when the pain began to bother him, where it occurs, what provokes it, and asks him to describe the sensations that arise during the attack. A neurological examination is then performed. The doctor asks the patient to turn, tilt his head, presses on certain points on the neck, trying to cause pain.
If after the examination there are still doubts about the diagnosis, or unusual symptoms are detected, the neurologist prescribes an examination. This may include blood tests, MRIs and other diagnostic tests.
Surgery
If conservative treatments do not provide pain relief, or if neurological symptoms such as numbness and arm weakness continue to worsen, then surgery may be considered.
The following surgical techniques are most often used in the treatment of cervical radiculopathy:
Anterior cervical discectomy and fixation
. This surgery is performed through a small incision in the front of the neck to remove the herniated disc, and then fixes that motion segment of the cervical spine to ensure spinal stability. This is the most common operation for root decompression.
Replacement of an intervertebral disc with an artificial disc
. This technique allows you to replace the fixation of the vertebrae. A potential advantage of this technique is that it aims to maintain mobility at this level of the cervical spine rather than fusion of two vertebrae.
Surgical treatment of radicular syndrome in the cervical spine can effectively reduce symptoms and restore conduction through nerve fibers. According to statistics, the efficiency rate ranges from 80% to 90%. As with any surgery, there are some risks, but most often the benefits of surgery outweigh the risks.
Treatment of occipital neuralgia
Many patients benefit from simple measures: rest, warmth on the neck, painkillers (ibuprofen, naproxen). Massage courses are useful: they help to stretch tense neck muscles.
If this does not help, your doctor may prescribe other medications: muscle relaxants (drugs that relax tense muscles), some anticonvulsants, antidepressants. Sometimes occipital nerve blocks are required - injections of drugs that interrupt the transmission of pain nerve impulses.
In rare cases, surgical treatment may be necessary. If the pain is due to the fact that the nerve is pinched by a blood vessel, microvascular decompression is performed. Sometimes, in order to block pain impulses, a special device is used - a neurostimulator.
In general, occipital neuralgia is not dangerous; most patients can cope with it. But in order to prescribe the appropriate treatment, you need to establish the correct diagnosis. Make an appointment with our neurological center by phone.
The material was prepared by Natalya Yurievna, a neurologist at the international clinic Medica24, Candidate of Medical Sciences Lasch.