Rheumatoid arthrosis is different in that it can affect patients at completely different ages. If degenerative osteoarthritis is often associated with aging processes in the body and occurs for the first time over the age of 50, then this form is characterized by early manifestation.
This article talks about the symptoms and diagnosis of rheumatoid arthrosis, the treatment of this formidable disease that can lead to disability and loss of performance at a fairly young age. If the symptoms of rheumatoid arthrosis are detected in a timely manner, treatment usually leads to the pathology entering a stage of long-term remission. In this case, no further destruction of the cartilaginous synovial tissue is observed. Putting arthrosis into remission is the most important task for every doctor dealing with this issue.
Rheumatoid deforming arthrosis is a chronic disease, which is based on a disruption of the immune system. Rheumatoid processes occur during a long-term state of carriage of pathogenic microflora. As a result, immune cells stop separating proteins into foreign and self. The attack begins on the serous membranes, synovial cartilage tissue, epidermis, etc. This is due to the fact that the markers of most strains of pathogenic coccal microflora are very similar to the collagen and hyaline cartilage that make up the membranes inside large joints.
Arthrosis is a pathology in which the cartilaginous synovial layer is destroyed. It protects the bone heads from friction and deformation. The cartilage layer inside the joint capsule plays the role of a shock absorber during movements. During compression, it releases synovial fluid, and when expanded, it absorbs it. This ensures tissue nutrition and uniform distribution of shock-absorbing load when walking, running or performing other movements.
Arthrosis begins with an inflammatory process. Most often this is arthritis or traumatic impact on the joint. During inflammation, the synovial cartilage membrane becomes fragile and undergoes rapid destruction. If the inflammation is stopped, but no measures have been taken to rehabilitate the cartilaginous layer, then it remains thinned. The next case of arthritis may cause the cartilage layer to proliferate in some places.
During the development of arthrosis, microscopic cracks form on the head of the exposed bones. They are filled with osteophytes and calluses. This stage is called deforming. When it occurs, the patient loses the ability to move independently and experiences constant pain. A secondary form of local osteoporosis and bone tissue destruction may develop. This leads to significant shortening of the limb.
If you develop rheumatoid arthrosis, then it is necessary to carry out regular maintenance therapy, which will inhibit the process of destruction of cartilage and bone tissue, prolonging the period of physical activity for the patient. In Moscow, to develop an individual course of treatment and rehabilitation, you can contact our manual therapy clinic. Experienced doctors work here. They will conduct a comprehensive examination and examination, make an accurate diagnosis and tell you what you need to do to maintain the possibility of physical activity for the rest of your life.
Causes of rheumatoid arthrosis
Etiologically, there is only one significant cause for the development of rheumatoid arthritis. This is rheumatism or a disruption of the immune system as a result of the carriage of pathogenic microflora. But not every patient who has suffered several cases of tonsillitis or suffers from chronic glomerulonephritis develops rheumatism. Therefore, it is logical to assume that there are negative factors that increase the risk of developing rheumatoid arthrosis. Let's look at them.
The reasons are divided into external and internal. Internal factors of pathogenic interference include:
- the presence of chronic connective tissue diseases such as psoriasis, systemic lupus erythematosus, gout, ankylosing spondylitis, etc.;
- improperly organized nutrition and insufficient consumption of clean drinking water;
- use of pharmacological drugs without a doctor’s prescription;
- various intoxications;
- disturbance of microcirculation of blood and lymphatic fluid;
- hypotension of skeletal muscles, including those associated with disturbances in innervation processes;
- diseases of the cardiovascular system;
- endocrine disorders (hyperfunction of the thyroid gland, hypersecretion of the adrenal cortex, diabetes mellitus, etc.);
- deficiency of certain nutrients (proteins, minerals, vitamins);
- destruction of bone tissue due to menopause (osteomalacia, osteoporosis);
- excess body weight.
With a high degree of probability, the development of rheumatoid arthrosis can be provoked by physical activity, hard work, prolonged stay in a static position, injuries in the form of bruises, cracks, fractures and sprains.
What is this?
Arthrosis is a chronic degenerative disease of the joints, which is expressed in their destruction (Fig. 1). In this case, all structures of the joint articulation are damaged - cartilaginous, bone, connective tissue (ligaments and joint capsule). The disease is common: it affects from 6–7 to 10–15% of the population of different countries. Thus, in the territory of the former USSR, 6-7% of the population suffers from arthrosis, and in the United States, 32.5 million adults suffer from arthrosis. Most often, this percentage includes people over 45 years of age, but there are also patients younger.
Figure 1. Development of arthrosis of the right hip joint (front view, diagram). During arthrosis, cartilage is destroyed, which over time leads to bone deformation. The damaged joint swells and hurts. Source: CC0 Public Domain
Rheumatoid arthrosis of the knee joint
Knee rheumatoid arthrosis is the most common form of the disease. Therefore, using his example, we will consider the stages and classification of the disease. Other joints are characterized by exactly the same pathological changes, but with a different localization.
Rheumatoid arthrosis of the knee joint is divided into the following forms of the disease:
- primary deformation of the joint without the primary development of arthritis (inflammation in the joint cavity);
- secondary post-traumatic arthrosis - develops against the background of aseptic inflammation, which can turn into a rheumatoid process and create conditions for long-term proliferation of cartilage and bone tissues;
- generalized variety - several joints (both knees) are involved in the pathological process at the same time.
In the area of the spinal column, an uncovertebral form of rheumatoid arthrosis may also develop with severe ankylosis and loss of flexibility and mobility. It develops according to the type of ankylosing spondylitis, but has a milder course with a more positive prognosis for the patient’s life.
In general, rheumatoid arthrosis goes through four stages in its development:
- on the first there are no visible signs of destruction and deformation of bone tissue;
- on the second, stiffness occurs, the leg muscles quickly tire, which indicates serious destruction of the cartilaginous synovial membrane of the joint;
- at the third stage, constant pain appears, crunching, creaking in the joint, stepping on the leg becomes painful and uncomfortable, secondary dystrophy of the muscles of the thigh and lower leg begins;
- the fourth stage is characterized by the development of secondary ankylosis - contracture makes the joint immobile, the patient can no longer step on the leg, and surgery is necessary to restore functionality.
Effective treatment using manual therapy methods is possible only at stages 1-2. With the third and fourth degrees of destruction and deformation of the joint, endoprosthetic surgery will be required.
Mechanism of disease progression
When any of the reasons that provoke joint disease with arthrosis appear, pathological processes begin to develop in it. The mechanism of their progression is not fully understood, but the main stages are known to official medicine.
At the initial stage, depletion of the cartilage tissue structure and abnormal changes in the synovial fluid occur. All this occurs as a result of metabolic disturbances, in which the tissues of the joints do not receive the necessary components in sufficient quantities, or are deprived of some of them.
Next, the elasticity of collagen fibers and the flexibility of cartilage are lost, due to the fact that the body, with a lack of nutrients, does not have time to produce hyaluronic acid, which ensures the softness and flexibility of the structural composition of collagen fiber. The cartilage gradually dries out, becomes brittle and cracks. The fluid in the synovial capsule is gradually depleted and subsequently disappears completely.
Roughness and hard bone formations form on the cartilage tissue. At the same time, deformation of other joint tissues develops, their pathological degeneration, dystrophy and loss of physiological activity.
For the patient, these changes mean the appearance of pain, lameness, and joint immobility.
Symptoms of rheumatoid arthrosis
Clinical symptoms of rheumatoid arthrosis depend on the stage of development of the pathological process. At an early stage, it is a vague, periodically occurring dull pain in the area of the affected joint. It occurs exclusively after heavy physical exertion on the articulation of bones. After a short rest, everything goes away without a trace.
At the second stage, the symptoms of rheumatoid arthrosis become more pronounced and include:
- almost constantly present pain that limits mobility;
- stiffness that does not allow you to make movements in the usual volume in the morning;
- the appearance of unpleasant extraneous sounds when making movements (creaking, crunching, grinding, squeaking, etc.);
- local swelling of the joint, pain on palpation, increased temperature and redness of the skin are determined.
At the third stage, joint deformation is visible to the naked eye. When taking an x-ray, areas are identified where synovial cartilage tissue is completely absent. They are covered with osteophytes and bone growths. When moving, they injure the joint capsule, provoke internal capillary bleeding and the development of a secondary inflammatory reaction.
Other diagnostic methods include MRI examination, ultrasound of soft tissues, blood test for rheumatic factor, general clinical blood test.
Diagnostic methods
To correctly prescribe treatment procedures, it is necessary to eliminate the cause of arthrosis. To detect it and make an accurate diagnosis, the following diagnostic methods are used:
- puncture with collection of synovial fluid;
- biopsy of cartilage tissue to check its structure;
- radionuclide examination method;
- radiography;
- Ultrasound.
Together with a rheumatologist or orthopedist, additional laboratory tests are prescribed - a general blood test, a study of electrolyte content, rheumatic tests, detection of sugar levels in blood samples, examination of protein fractions.
How to treat rheumatoid arthritis?
Many patients are interested in the answer to the question of which specialist treats rheumatoid arthrosis of the knee joints, and which doctor should make an appointment with. Many people believe that this disease is under the purview of a rheumatologist. Actually this is not true. A rheumatologist can stop acute inflammation. But he will not be able to restore the functionality of the affected joints. An orthopedist or osteopath, or a chiropractor can help with this.
Therefore, before treating rheumatoid arthrosis, try to collect as much information as possible about the available methods and methods of treatment.
For example, with the help of manual therapy methods, you can completely defeat rheumatoid arthrosis of the hands and restore lost fine motor skills of the hands. For this purpose, reflexology, laser treatment, therapeutic gymnast courses and massage are used. Positive results from such treatment can be obtained only in the early stages of the disease. Therefore, if clinical symptoms of rheumatoid arthrosis appear, you should immediately consult a chiropractor or orthopedist.
Complications
The consequences of untimely treatment and advanced arthrosis of the joints are fraught with complications such as:
- disability;
- deformation beyond repair;
- the appearance of vertebral hernias;
- inactivity or immobility of the joint;
- decline in quality and standard of living.
The chronic course, in addition to these complications, is accompanied by intense and frequent pain, complete destruction of the structural components of the joint, discomfort, and the inability to perform physical work and play sports.
Treatment of rheumatoid arthrosis
As mentioned above, treatment of rheumatoid arthrosis in the later stages is only possible using surgical methods. This is endoprosthesis replacement of the affected joints, followed by rehabilitation and restoration of muscle performance.
In the early stages, manual therapy methods can be used to treat rheumatoid arthrosis:
- Osteopathy and massage allow you to restore microcirculation of blood and lymphatic fluid, restore elasticity to all soft periarticular tissues;
- acupuncture restores normal body tone, starts the process of regeneration of damaged tissue in the joint area;
- therapeutic exercises increase the amplitude of mobility and maintain it for many years, activate diffuse nutrition through active muscle work;
- kinesiotherapy allows you to effectively combat ankylosis and contractures;
- physiotherapy improves tissue condition;
- laser treatment allows you to get rid of osteophytes and bone growths;
- electromyostimulation is used for severe muscle dystrophy.
The course of treatment for rheumatoid arthrosis is developed individually. To do this, you need to make an appointment for a free appointment with a chiropractor at our clinic. Call the administrator and agree on a time convenient for your visit.
knee
knee
- as an addition to surgical treatment during any operations except joint replacement;
- an alternative to surgical treatment for those for whom surgery is contraindicated;
- used while waiting for surgery.
Painkillers
To reduce pain, most patients are prescribed 2 groups of medications:
- non-steroidal anti-inflammatory drugs (NSAIDs);
- chondroprotectors.
The first ones work instantly, but give a short-lived effect. While chondroprotectors do not act immediately, they reduce pain only after several months of regular use. The effect is less pronounced. But chondroprotectors are absolutely safe, they complement NSAIDs, and therefore are often prescribed by doctors even with advanced arthrosis.
The main NSAIDs that are used:
- aceclofenac – good because it improves metabolism in cartilage tissue;
- diclofenac, ibuprofen – have a pronounced anti-inflammatory and analgesic effect;
- meloxicam, celecoxib, nimesulide - have a lower risk of developing complications from the gastrointestinal tract, therefore they are often prescribed to patients over 65 years of age or with a history of erosive and ulcerative lesions of the gastrointestinal tract.
Doses of drugs should be as minimal as possible to relieve chronic pain. However, painkillers must be taken constantly, because advanced forms of arthrosis are accompanied by pain even at rest.
Intra-articular injections
A large number of different medications (glucocorticoids, proteinase inhibitors, chondroprotectors, anesthetics) can be administered inside the joint. But not all of them are equally effective, and some are even dangerous. We use two drugs for intra-articular administration, which:
Alternative operations
In recent years, the frequency of alternative surgeries for osteoarthritis has been decreasing. This is especially true for the hip joint. But for degenerative-dystrophic processes of the knee joint, alternative methods of surgical treatment are quite common. They can achieve significant improvement in the patient’s condition for several years. The main advantage of such methods is the following:
- the own joint is preserved;
- long-term rehabilitation is not required, because the methods used are mostly minimally invasive (carried out with arthroscopic access);
- less risk of complications.
Arthroscopy allows you to perform many manipulations on the joint. The doctor determines which of them are necessary individually. To do this, an MRI of the joint is performed before surgery. In addition, arthroscopy itself has enormous diagnostic value.
During the operation, the doctor may perform the following actions:
- rinse the joint, remove inflammatory fluid from it;
- remove fragments of damaged menisci, altered Goff bodies, restore ligaments, remove loose bodies;
- perform osteochondral mosaicplasty or tunnelization.
Some patients undergo multiple surgeries. All actions can be performed in one treatment step. Less commonly, two-stage surgery is performed (two operations on different days).
Osteochondral mosaic plastic surgery
Osteochondral mosaicplasty is an operation that involves taking a section of non-load-bearing cartilage and transplanting it onto the articular surface of a joint damaged by arthrosis. The technique gives good results, but can be used in no more than 5% of cases with osteoarthritis, since it requires certain conditions:
Stages of the disease
Arthrosis of the joints develops gradually and in the process goes through three successive stages that determine the severity of the disease:
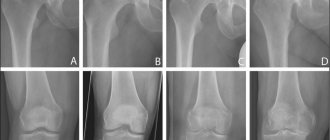
- Stage 1: the pathology is not detected on X-ray or ultrasound, but the destruction processes have already started; the composition of the joint fluid changes, as a result of which the tissues receive fewer nutrients and become more sensitive; increased stress on the affected area causes inflammation (arthritis) and pain;
- Stage 2 is characterized by active destruction of cartilage tissue, and bone spines and growths appear along the edges of the articular platform (the area of contact of surfaces); at this time, the pain becomes habitual, and the inflammatory processes become stronger and weaker; spasms of the muscles associated with the joint are periodically observed;
- Stage 3: areas of destruction affect almost the entire surface of the cartilage, the articular area is deformed, the affected limb deviates from its axis; range of motion decreases and ligaments weaken and become short.
Some experts also distinguish stage IV of the development of arthrosis. It is characterized by almost complete immobility of the joint.