Make an appointment by phone: +7 (343) 355-56-57
+7
- About the disease
- How to cure
- Prices
- Sign up
- Specialists
- About the disease
- Prices
- Sign up
This is inflammation of the tendon followed by a degenerative process, which is localized in the knee joint. The pathology is often found in athletes. In most cases, the patellar ligament is affected at the site of its attachment to the bone structures.
Why does the disease occur?
Tendonitis of the knee joint is a problem for physically active people, most often teenagers and professional athletes. Numerous jumps on hard surfaces during volleyball, basketball, tennis, football and athletics provoke the disease.
Contribute to the development of pathology:
- incorrect training regimen;
- uncomfortable shoes;
- knee injuries;
- long-term therapy with antibacterial drugs;
- foot deformities (flat feet, hallux valgus, etc.);
- posture disorders and spinal diseases;
- overweight;
- lack of muscle elasticity;
- wide hips in women.
Secondary tendonitis is a complication of rheumatic, infectious, parasitic diseases and metabolic pathologies.
Pathogenesis
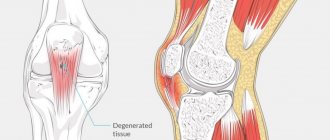
As a rule, inflammation occurs at the site of attachment of the patellar ligament to the bone. With excessive loads, microdamages with local hemorrhages occur in the tendon tissue, which cause aseptic inflammation. The outcome of the inflammatory process is necrosis of collagen fibers and replacement with scar tissue.
A tendon with many scars is fragile, inelastic, and therefore vulnerable and easily injured again. New microbruises, aseptic inflammatory process and scar, long-term sluggish course, leads to degeneration and thinning of the tendon-ligamentous structures of the joint.
Clinic
Clinical manifestations increase gradually and progress slowly. First, pain on the front surface of the knee occurs at peak loads. Further, dull, periodically paroxysmal pain bothers you during normal exercise, and quickly disappears after stopping training. Gradually, pain and discomfort progress, not disappearing after 4-8 hours of rest. As a result, a tear or rupture occurs in the pathologically altered tendon.
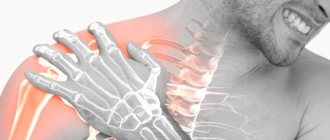
A characteristic clinical symptom of tendinitis is pain when palpating the tendon, when pressing on the tibial tuberosity, or patella. Sometimes local swelling and hyperemia of the adjacent skin, limited range of motion, and creaking and crunching when flexing and extending are characteristic.
Important! Untreated tendonitis reduces resistance to physical activity, interferes with training, and can put an end to a sports career.
Lunge with torso rotation and toe touching
Role of the exercise: Activates neuromuscular control and proper functioning of the entire kinetic chain from the moment the foot hits the ground.
How to do it: Stand straight with your feet hip-width apart. Take an extended step forward (about two feet), then lower your hips into a lunge phase until your front thigh is parallel to the ground (or as deep as is comfortable). The knee of the front leg should be behind the toes of the same front leg, squat. From here, slowly move forward to touch your front leg with your opposite hand, focusing on proper foot placement and alignment of your posture—don't let your knees bend inward and avoid rounding your back as you reach the goal. Return to a vertical lunge position, then stand with your legs straight and feet together to... Step forward again with the opposite foot and repeat the above.
Volume: three sets of 10-15 repetitions on each leg.
Diagnostics
The doctor makes a diagnosis based on a history of sports or other injuries and a characteristic clinical picture. Additional examination methods (ultrasound, CT and MRI of the knee joint) are usually not required.
An x-ray of the knee sometimes shows slight thickening of the soft tissue. With ossifying tendonitis, there are foci of calcification.
Reference! CT, MRI and ultrasound are indicative of advanced stages of the disease. Ultrasound of the knee joint reveals a violation of the tendon structure. MRI and CT scans reveal ligament damage.
Laboratory tests are relevant for secondary symptomatic tendonitis. Rheumatoid diseases are indicated by anticiruline antibodies and rheumatoid factor, accelerated ESR, and metabolic pathologies are indicated by increased levels of creatinine and uric acid.
Most often, tendinitis is differentiated from injuries to the bone structures of the knee joint and rheumatoid diseases. The decisive method in this situation is the x-ray diagnostic method.
Treatment
Treatment of knee tendonitis is usually conservative outpatient. Surgical interventions are indicated for ineffective conservative therapy and tendon ruptures.
Treatment methods include:
- Protective mode. Stop training, recommend rest, and in some situations immobilize with plaster or plastic splints.
- Drug therapy with NSAIDs. Nonsteroidal anti-inflammatory drugs (naproxen, ibuprofen) are prescribed to relieve swelling, inflammation and relieve pain. The duration of administration is limited due to side effects from the gastrointestinal tract.
- In case of severe swelling, intense pain, widespread fibrosis, radiotherapy, blockade with glucocorticosteroids and shock wave therapy are prescribed. Hormonal drugs are administered in short courses with an interval of at least 6 months. Such regimens are recommended to avoid serious side effects (including progression of tendon degeneration).
- Physiotherapy. After acute manifestations subside, therapeutic exercises, massage, electrophoresis with novocaine, iontophoresis, UHF and magnetic therapy are prescribed.
- "GIAL-IN" and "GIAL-IN PROLONG" are medical biological products for periarticular or subcutaneous administration. A metabolite of the drug, hyaluronic acid, is part of the connective tissue of all living organisms. Penetrating into the intercellular spaces, the biological product stimulates metabolic and regenerative processes in ligaments, cartilage, joint capsules and synovial membranes of muscles.
Reference! "GIAL-IN" has no side effects and no restrictions on the duration of use. Indicated for tendonitis, degenerative-dystrophic changes in tendons, ligaments, cartilage and soft tissues.
During rehabilitation, the joint is loaded gradually. When the disease is in remission, it is recommended to regularly unload the damaged ligament using special tapes (stape) or fix the joint with an orthosis.
Good results are ensured by targeted improvement of the technique and height of jumps, since tendinitis occurs more often in athletes who practice hard landings, high jumps or landings with a deep squat.
Symptoms of knee tendonitis
The main symptoms of knee tendinitis are:
- pain when moving the affected limb;
- painful sensations on palpation;
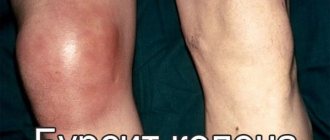
- increased temperature in the area of inflammation, possible redness;
- deterioration of joint mobility;
- prolonged pain, intensifying at night.
In addition to common symptoms, the stages of development of pain syndrome are also distinguished:
- The first stage is characterized by pain in the tendon area only at the peak of physical activity. In any other circumstances there is no pain.
- At the second stage, dull pain occurs even with standard physical activity.
- At the third stage, the pain does not subside even after a long rest.
- The fourth stage is the last in the development of the disease. The tendon of the knee joint loses its strength, and the tissues undergo minor tears. Rupture is possible during physical activity.
With secondary tendinitis, symptoms appear faster and pain develops more intensely. The spread of inflammation goes away in just a couple of days, and the swelling is more pronounced. Hyperemia occurs in the affected area, and in rare cases, hyperthermia of the skin.
At the first signs of tendonitis, it is strongly recommended to seek help from a specialist. Self-diagnosis can lead to serious consequences, since the symptoms of tendinitis are similar to tendinosis. However, their treatment is different.
Surgery
Surgical interventions are indicated for tendon tears, ruptures, or ineffective conservative treatment for 1.5-3 months. The operation is performed as planned in an orthopedic or trauma hospital. The skin over the pathological area is dissected, the ligamentous canal is opened, and necrotic tissue is removed.
In some situations, to stimulate reparative processes, the lower part of the patella is scraped out or multiple incisions are applied through traditional or minimally invasive endoscopic access.
For significant tears and ruptures, surgical reconstruction of the patellar ligament is indicated.
After the operation, antibacterial drugs, painkillers, physiotherapy and massage are prescribed. They are allowed to train after rehabilitation, recovery is possible within 2-3 months.
Fix tight hamstrings permanently
Tight hamstrings are the bane of every athlete's life, opening the door to a range of pain and problems ranging from muscle strains, knee pain and poor posture to decreased strength and performance.
This may be why hamstring stretching is such a ubiquitous feature in fitness programs, pre-race warm-ups, and physical therapy protocols.
Despite countless hours spent stretching and massaging these incorrigible musculoskeletal conditions, most people still struggle with tight hamstrings. But they think for the wrong reason.
A Quick Guide to Muscles
Muscles are not solid pieces of flesh that function as a single unit. Like all the different parts of our body, muscles are made up of smaller and smaller subunits that are linked together like links in a chain.
Within each subunit are proteins that have the unique ability to move closer (contract) or further away from each other (stretch). The relative proximity of the proteins to each other determines the overall length of the muscle.
It is generally accepted that if a muscle lacks range of motion, it is because the chain is too short—not enough links—or the links are somehow tied. In theory, stretching could correct the tension by stretching the links or, over time, adding more links to the chain.
An unexpected fork in the road
The reality is that except in very rare circumstances (usually associated with prolonged immobilization after injury), muscles do not fall out of the chain links. The length of the muscles in an absolute sense is always the same.
What CAN change is the amount of tension in the muscle, and this is a function of the overall position the muscle is in, not a change in raw material. So, although your hamstrings may be "tight", it's probably not because they're too short.
The Real Reason Your Hamstrings Get Tight
Your hamstrings and all the other muscles are like giant elastic bands. When you pull the ends of these "bands" in opposite directions, they become longer and tighter. In other words, the more they are stretched, the more tension is retained in the bands and the more stable they become when stretched further.
This is why decreased mobility and a feeling of “tightness” under the knees when bending forward does not necessarily mean that the muscle is short; it is often a sign that the opposite is true.
This explains why some people's tight hamstrings never improve, no matter how hard they stretch them. In fact, most people are in the too-long camp rather than the too-short camp.
The pelvis is to blame for everything.
The hidden life of your pelvis
In addition to being the anchor point of your hamstrings, your pelvis should also synchronize its position with your ribcage. The thoracic diaphragm (attached to the inside of your chest) and pelvic floor (the muscles that run through your pelvic floor) act as a sort of container for the internal pressure created by the air moving in and out of your lungs and internal organs. move while driving.
It's kind of a brute physics thing that your musculoskeletal system has to deal with, but the pelvis and pelvic floor muscles set the foundation for the rib cage and thoracic diaphragm to act on. Between the chest ceiling and the pelvic floor is all your soft stuff.
None of this is a problem. Not yet.
Modern people sit a lot and strain a lot, both of which affect the body. Long periods of sitting place the hip flexors in a shortened position. This ends up pulling the pelvis forward and down at the front while pulling it up at the back where the hamstrings attach. This causes one end of the muscle to separate from the other.
As for stress, let's just say that it has the expected effects on our physiology, including increased heart rate and blood pressure, extra sweating and dilated pupils, among a variety of other markers.
One of these markers is increased extensor tone (hyperactivity) in the muscles that extend the body, especially in the back. It is essentially a fight or flight pose that prepares the body for action.
This is the same situation we find ourselves in when we perform virtually all the major exercises—squats, deadlifts, pull-ups, and presses—for two reasons. Firstly, lifting very heavy shit is extremely difficult and dangerous for your body, and secondly, extension is a very stable position from which to do it.
As before, the pelvis moves forward, rotates anteriorly, and the hamstrings stretch and tighten like an overstretched rubber band. Either way, the net result is over-lengthening of the hamstrings with excess tension.
What to do instead
Other than briefly increasing range of motion, stretching doesn't work here. You should focus on restoring normal pelvic alignment, which will in turn restore normal length and tension in your hamstrings.
Here are four exercises you can do for 5-10 minutes a day that will make your yoga mat obsolete.
90/90 Skywalker
If the problem is long, hyperextended hamstrings secondary to an anteriorly rotated pelvis, then restoring normal alignment is a game of balancing the tension. Press firmly on the bone and it will change position. This is the concept of using braces to strengthen teeth.
The 90/90 Skywalker (credit to the Postural Restoration Institute for the idea) uses the tension created by the hamstrings and their attachment points on the pelvic bones to pull the pelvis back and down:
- Place your feet on a wall, chair or sofa.
- Press through your heels, imagining that you are pulling or dragging a wall (or something else) towards the ground. This should involve the back of your legs, similar to a hamstring curl without movement.
- Bend your buttocks so that the back pockets of your pants reach your knees.
- Step away from the wall and reach for the sky.
- Reach your opposite hand towards the foot of the leg that is in the air.
- Maintain this position for 3-5 sets of 5 breaths, moving a little further with each exhalation.
Lazy Bear
The hamstrings aren't the only muscles that position your pelvis and allow you to touch your toes. This is where your abs, especially your internal obliques, come into play.
These powerful abdominal muscles, located on the sides of your torso, connect your rib cage and pelvis. This makes them convenient for reshaping the spine by removing the arch from the middle and lower parts, thereby turning the pelvis back.
- Start on all fours - hands and knees on the ground, feet pressed against the wall.
- Shift more of your weight forward into your hands as you roll your pelvis back and round your upper back, spreading your shoulder blades and drawing your ribcage toward your body.
- Raise your knees 1-2 inches off the ground.
- Exhale and try to sink deeper into this position.
- Inhale and try not to lose the pose.
- Repeat 3-5 sets of 5 breaths.
3. Pull-out strap for high knees
If the lazy bear is hamstrings-abdominal integration 101, then this is exercise 102, using an upright position but with bent knees for optimal engagement and extra reach to align the chest and pelvis:
- Kneel with both knees on the mat or ground. You can place a weight platform on your heels or place your feet under a glute pad.
- Lower your knees and pull your hips into a backward tilt.
- Wrapping the resistance band around your upper back, exhale and extend your arms forward, pulling your ribs down and back.
- Repeat 2-5 sets of 5 breaths.
Hind leg elevated, RDL
One of the problems associated with an anteriorly oriented pelvis is the inability to expand the dorsum of the thigh when bending forward. As a result, the hip cannot be pushed all the way back into the socket to allow normal hip rotation.
Instead of trying to stretch the problem, here's how to fix it with a modified traditional single-leg deadlift:
- Place the weight platform under your back foot (so your hip is toward the back of your thigh) while holding a kettlebell in your opposite hand.
- Rotate your hips toward your back foot as you reach with the weight in the same direction.
- Press into the ground with your front foot to maximize your posterior hip shift.
Let me repeat the problem so it sinks in
Tight hamstrings are often a problem, but stretching is rarely an effective treatment.
This is why people can stretch every day for years without ever making significant or lasting changes in range of motion or the subjective feeling of tightness in the back of their legs.
More often than not, the real problem is excessive stretching of the tissue leading to overstretching.