16 June 2020
43479
1
3.9 out of 5
Hemangiomas are vascular tumors that can occur in the skin and any internal organs that contain a network of blood vessels. Thus, such formations cannot form only in the articular surfaces and optically transparent environments of the eyes. The spine is one of the places where it can form. In such cases, a hemangioma of the spine, or more correctly, a vertebra, is diagnosed.
A tumor of this kind in 100% of cases is a benign neoplasm and never becomes malignant, i.e., does not turn into malignant. Vertebral hemangioma is localized in its thickness, which is due to the peculiarities of the blood supply to the structural elements of the spine, and is, so to speak, an advantageous location for a tumor of this type. Growing inside the spongy tissue of the vertebra, the vascular formation is reliably protected from external influences by the bone, which reduces the risk of injury to a minimum. At the same time, hemangiomas formed in the parenchyma of internal organs are easily damaged and can become a source of severe bleeding.
In recent years, the frequency of diagnosing vertebral hemangiomas has increased significantly, but not due to an increase in the number of cases of their formation, but due to the introduction of modern diagnostic methods: CT and MRI.
Methods for removing hemangioma
To get rid of hemangioma, the following methods are used:
- organ removal surgery;
- injection of alcohol into the tumor (alcoholization);
- embolotherapy;
- radiation therapy (radiotherapy);
- surgery.
Resection (surgery to remove an organ)
The method has been developed and used since past centuries, in the 30s. This method is characterized by a large number of complications:
- problems with spinal cord nutrition;
- bleeding from tumor vessels;
- fractures.
Due to the high probability of developing the above problems, the method is used extremely rarely and serious complications - the compressive effect of the tumor on the vertebra or its roots.
Alcoholization
Alcoholization involves the procedure of injecting alcohol into the site of a tumor in order to destroy or reduce it in size.
There is a negative side - depletion of the vertebral bones, their destabilization. A few months after the operation, a vertebral fracture is possible.
Embolotherapy
The essence of the method is to cause embolism (blockage of blood vessels). It is necessary to disrupt the nutrition of the hemangioma; for this, a special solution is injected under the skin. It is possible to inject the solution directly into the tumor (selective embolization of neoplasm vessels).
The disadvantage of this method is a possible relapse. Small hemangioma vessels may remain in the tissues, which will subsequently grow. There may be a violation of the statics of the lumbosacral spine, and disturbances in the nutrition of the spinal cord.
Radiotherapy
A common method of treating this disease. When carrying out therapy, when compared with the first method (surgery), the risks are minimal, but they do exist. During radiation therapy, a person is exposed to radionuclides (a group of atoms that have the property of radioactivity) that affect the entire body.
To completely remove the tumor, a large dose of radiation may be required, as a result of which other internal human organs will suffer, especially the reproductive system in women and the fetus of pregnant women. Also, after removal of the tumor, the thickness of the vertebra will decrease - there is a risk of a compression fracture (a fracture of one individual or several vertebrae).
Operation
Surgery – surgery is performed to strengthen the damaged spinal column. A special cement composition with barium sulfate and titanium is injected into the affected part of the vertebra. As a result, barium acts on the tumor, causing the tumor to shrink, and the vertebral body is strengthened with bone cement. This reduces the risk of compression fracture to a minimum.
Treatment of vertebral hemangioma
Due to the fact that any vertebral hemangioma is securely hidden inside the vertebral body, it is absolutely pointless to use any conservative methods to treat it. Massage, reflexology, hirudotherapy, drug treatment and other methods are not able to have any effect on the vascular formation, not only on its size, but also on its tendency to grow. Therefore, the only way to get rid of hemangioma and permanently remove the sword of Damocles hanging over your head in the form of possible complications is only through surgery.
Today, the following are used for surgical treatment of vertebral hemangioma:
- percutaneous puncture vertebroplasty;
- alcoholism;
- embolization
Previously, to remove vertebral hemangiomas, radiation therapy was used or all altered parts of bone tissue were removed along with the vascular tangle. But both methods had to be abandoned due to lack of effectiveness and a high risk of neurological disorders or other disorders.
Yes, and alcoholization, as well as embolization of hemangioma, is being gradually abandoned today, since percutaneous puncture vertebroplasty gives the best result and has a number of additional advantages.
Alcoholization
The method was developed at the end of the twentieth century. It is based on the ability of alcohol to provoke vascular thrombosis and destruction of endothelial cells.
Sclerotherapy using ethyl alcohol (alcoholization) or other compounds, although it leads to the destruction of the tumor, does not allow achieving high strength of an already fairly destroyed vertebra, and alcohol additionally has a negative effect on the strength of bone tissue. Therefore, even after such operations, the risk of a vertebral compression fracture was not eliminated with all the ensuing consequences.
In some cases, with the help of alcoholism, it was not possible to achieve the death of the tumor at all, which over time led to its relapse. Studies also show the possibility of developing paravertebral abscesses (in the soft tissues surrounding the spine) and myelopathy with Brown-Séquard syndrome after using the method. In such cases, central paralysis and serious disturbances of sensitivity in one half of the body were observed against the background of a decrease in pain sensitivity and temperature in the other half.
Embolization
The method was developed and introduced into medical practice in the late 60s. XX century. Embolization required the participation of a vascular surgeon and the performance of several punctures. It involved the introduction of special substances into the vascular bed that caused the formation of blood clots and cessation of blood circulation in this area of the circulatory network.
There were 2 ways to introduce emboli: into the area of the hemangioma and into nearby vessels. In both cases, the surgical intervention was technically complex and did not allow a radical solution to the problem, since although the blood flow in the main vessels stopped, new ones constantly appeared, which led to a relapse with even more serious risks of a vertebral compression fracture.
Vertebroplasty
This operation is one of the modern minimally invasive interventions that are safe and highly effective. The essence of the method is to eliminate the cavity inside the vertebral body by filling it with special bone cement. It is designed in such a way that once inside, the mass quickly expands and fills the entire space, destroying the tangle of blood vessels located in it.
Bone cement is not a one-component product. It includes:
- a quickly hardening biopolymer that directly fills the vertebral body;
- X-ray contrast agent that allows you to accurately control the quality of vertebral filling in real time;
- antibacterial compounds.
Vertebroplasty does not require any incisions, so it leaves no noticeable scars on the skin. The procedure is performed under the control of an image intensifier, but initially the spinal surgeon must find the affected vertebra and very accurately apply markings to the skin. Local anesthesia is then administered and a needle is inserted into the vertebra. The operating neurosurgeon monitors the accuracy of each movement through a monitor.
As soon as the needle passes the intact vertebral wall and plunges into the tumor, a cementing agent begins to be injected through it. Its properties are such that it provokes heating of surrounding tissues up to 60°C. As a result of heating, the tumor cells are completely destroyed, and due to the ability of bone cement to expand, it will completely fill all the voids inside the vertebral body and quickly harden. This ensures the restoration of the natural hardness of the vertebra and its solidity.
The completeness of filling the vertebra with bone cement is controlled using an image intensifier, so the neurosurgeon always knows exactly how much more mass needs to be applied to completely fill all the voids. On average, about 4 ml of cementing mass is required to treat a hemangioma of the cervical vertebra, and 6-7 ml of the product is needed to treat a tumor of the lumbar vertebrae. The postoperative puncture does not require sutures and is covered with a sterile bandage.
Bone cement is prepared immediately before injection into the affected vertebra by mixing a liquid monomer with a powdered polymer.
Since vertebroplasty is performed under local anesthesia, it can be performed even on elderly people with concomitant heart and respiratory diseases for whom general anesthesia is contraindicated. But it is contraindicated for:
- diabetes mellitus in the stage of decompensation;
- blood clotting disorders;
- acute period of infectious diseases;
- the presence of manifestations of skin infectious and inflammatory diseases in the projection of the affected vertebra;
- individual intolerance to bone cement components.
Surgery to remove hemangioma does not require a long hospital stay, a difficult recovery period and has an extremely low risk of complications. After it is completed, the patient can literally leave the clinic the next day and return to everyday duties. But immediately after completing the procedure, he must remain motionless on the operating table for 2 hours. After their expiration, the patient is allowed to get up and move independently.
Surgical treatment of complications of hemangioma
If the hemangioma has grown so large that it has led to a vertebral fracture, this often requires immediate surgery to restore its integrity and eliminate compression of the spinal canal. In some cases, vertebral compression fractures are treated conservatively, but in the presence of a hemangioma this can be dangerous. After all, the tumor will interfere with bone fusion, and since it is no longer protected by bone walls, the risk of injury and bleeding increases sharply.
If a vertebral hemangioma has led to compression of the spinal cord and its roots, patients are prescribed open surgery. Preference is given to decompression techniques that allow the removal of elements compressing the spinal cord.
In such cases, the surgeon makes a soft tissue incision at the level of the spinal cord lesion, carefully moves the muscles apart and assesses the situation visually. In most cases, it is necessary to remove part of the vertebra, its spinous processes, arches, and in especially complex cases, the body along with the hemangioma. This way the surgeon gains access to the damaged area of the spinal cord and removes the formations compressing it.
Depending on the radicality of the operation, the removed bone fragments and intervertebral discs can be replaced with special implants or grafts taken from the patient’s own bone. If there is a risk of spinal instability, the structures of the operated spinal motion segment are fixed with metal structures and screws to healthy vertebrae. The final stage of the operation is layer-by-layer application of sutures and a sterile dressing.
This operation is very traumatic, but with compression of the spinal cord there is no choice. Otherwise, the patient faces severe disability. After it, a long recovery is required using various types of rehabilitation. Therefore, it is much better not to let aggressive vertebral hemangioma progress to such an extent; if it is detected, be examined regularly and if indications for surgery arise, prepare for it without delay.
Thus, vertebral hemangioma is a benign tumor that has nothing to do with cancer. Moreover, as long as it is stable, that is, it does not grow, it does not affect the quality of life and does not manifest itself in any way, and therefore does not require any treatment, but only dynamic observation. As long as the mass occupies less than half of the vertebral body and does not cause a serious risk of compression fracture, it is considered relatively harmless. But in other cases, surgery is the only way to avoid the development of extremely dangerous complications.
Symptoms of the disease
Hemanglioma has different symptoms depending on its size, histological structure and location within the spinal column. If the size is small (within 1 cm), there are no symptoms and the tumor can be detected by chance during X-ray or MRI.
Upon reaching a larger size, symptoms begin to appear if the location of the hemangiolipoma irritates the pain receptors of various structures of the spine (vertebrae, intervertebral discs, muscles). Pain is the very first and most common symptom for all departments, but can be of a different nature, from dull and aching to sharp and unbearable.
Tumor growth contributes not only to an increase in pain, but also to the appearance of neurological disorders. Occupying more and more space, the neoplasm puts pressure on the spinal cord, intervertebral discs and nerve fibers. As a result, the natural position of these structures and the quality of the functions they perform are disrupted.
For example, a displaced spinal disc together with a tumor can irritate the afferent and efferent roots of the spinal cord and disrupt the sensory and motor innervation of the limbs. Partial impairment of movement and sensitivity is called paresis.
In their complete absence, paralysis occurs. Growing horizontally, the tumor can displace the spinal column relative to the vertical axis, which will lead to scoliosis. Disc displacement leads to the formation of intervertebral hernias.
When bone tissue is lysed by osteoblasts, the strength of the vertebrae decreases and, as the load on the spinal column increases, spontaneous compression fractures occur. Fatigue and fatigue may also occur, which reduce the quality of life and cause discomfort.
Characteristic symptoms in the spine with hemangiolipoma:
| Spine department | Effect of tumor | Symptoms |
| Cervical | Compression of the cervical artery, impaired circulation in the brain. | Headache, pressure changes, dizziness, sleep, hearing and vision disturbances. |
| Chest | Compression of blood vessels and nerve fibers that supply and innervate the upper limbs. | Disorders of the heart rhythm, digestive system, decreased sensitivity and numbness in the hands and fingers. Paresis and paralysis of the upper limbs. |
| Lumbar | Compression of blood vessels, pressure on the spinal cord. | Tingling and numbness in the feet, paresis and paralysis of the lower extremities. Dysfunction of the urinary system. |
We advise you to study - Inflammation of the coccygeal tract
If the damage has affected areas of neighboring departments, a complex picture of symptoms can be created. For example, when the thoracic and lumbar segments (Th12 – L2) are affected, disturbances are observed in the functioning of the heart, gastrointestinal tract and reproductive system.
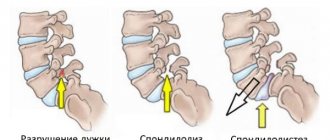
Main hazards
A vertebral hemangioma may or may not grow in size. A stable hemangioma, especially a small one, does not pose a serious threat. Since a formation of this kind is not prone to malignancy, its main danger lies in its destructive effect on the vertebra in which it is located. The result may be:
- vertebral compression fracture;
- stenosis of the spinal canal at the level of the affected vertebra with the occurrence of compression myelopathy and severe neurological abnormalities characteristic of this condition;
- compression of the spinal canal with damage to the dura mater by bone fragments up to penetrating wounds of the spinal cord.
Vertebral hemangioma is not capable of leading to severe bleeding, firstly due to the absence of the risk of mechanical damage, and secondly due to the fact that the vertebrae do not have such an active blood supply as internal organs. Therefore, if the hemangioma has not yet destroyed the vertebra so much that a careless movement or blow led to a compression fracture, then bleeding is impossible. But if a fracture has already occurred and the operation has not been performed, the formation can be damaged by sharp bone fragments, resulting in bleeding and sometimes the formation of hematomas.
Criteria for assessing the danger of hemangioma
The risk of complications is directly dependent on:
- size of hemangioma;
- location;
- growth rate;
- patient's age;
- the presence of concomitant diseases and individual characteristics.
It is impossible to name the specific size of the hemangioma at which surgical intervention is already necessary. For example, the discovery of a hemangioma measuring about 1 cm in a large adult man in the body of the 4th or 5th lumbar vertebra cannot be considered a dangerous condition. Therefore, in such situations, it is recommended to keep the tumor under control and undergo routine examinations annually. This will allow you to notice in a timely manner if it begins to grow and there is a risk of complications. At the same time, if a vascular tumor of a similar size is detected in the cervical vertebra of a miniature girl, surgery must be performed as soon as possible to avoid dangerous complications.
The lumbar vertebrae are the largest structural elements of the entire spine, and the cervical vertebrae are the smallest.
Such differences in the management of patients with hemangiomas of the same size but different locations are explained by the fact that at the level of the 4th vertebra of the lumbar spine the spinal cord no longer passes (it ends at the level of the 1st or 2nd lumbar vertebra). Therefore, even if, against the background of the existence of a vascular tumor, a compression fracture of the body of the 4th lumbar vertebra occurs, this will not lead to such terrible consequences as if it happened in the cervical spine.
In the first case, the patient is at maximum risk of developing cauda equina syndrome, caused by the infringement of a number of nerve fibers that make up its composition. This may result in:
- pain in the buttocks, lower extremities;
- numbness of the legs, buttocks, perineum;
- erectile dysfunction;
- urination disorders.
Of course, such complications are also absolutely undesirable, but they do not pose a threat to life. But if the hemangioma destroys the cervical vertebra, resulting in a compression fracture, this will lead to profound disability, since everything below the level of damage to the spinal cord will be paralyzed.
Thus, the size of the hemangioma is not the only indicator of its danger. Therefore, in each case, the level of threat is assessed strictly individually.
Important criteria for danger are the growth rate and the position of the tumor inside the vertebra. If the formation does not grow and is of non-critical size, there are no indications for surgery. Also, a tumor is considered relatively safe if it is small and located approximately in the center of the vertebra and is protected on all sides by healthy bone tissue. In such situations, the risk that the vertebra will break is minimal. Therefore, surgery is also not indicated. But if the hemangioma is located close to the border of the vertebral body, this significantly increases the likelihood of complications.
When assessing the danger of a vascular tumor, the condition of the bone tissue is also taken into account. When it is detected in a young man with healthy bones, the prognosis is more favorable than when a vertebral hemangioma is diagnosed in an elderly woman. In the latter case, osteoporosis will additionally be present with a high degree of probability. Therefore, even a small hemangioma will be much more dangerous than a larger formation for a healthy person.
Thus, the decision on the need for a planned operation is made only on the basis of a whole complex of data on a strictly individual basis. If a vertebral hemangioma that does not threaten the development of complications is detected, the patient is recommended to be examined again in a year. If it shows no growth, it is suggested to undergo diagnostics again in a year. If the size of the tumor is stable, the person is released for 3 years. If this examination does not show any changes in the condition of the hemangioma, the next one can be carried out after 5 years, and then not worry about it at all.
To simplify the assessment of the danger of vertebral hemangioma, cases where it occupies more than 55–60% of the vertebral body and is prone to growth are considered an indication for considering the need for surgical intervention.
Treatment methods
Not all patients require treatment, as about 10% have an aggressive form of the disease. Therapy is developed individually for each patient. Before answering the question: How to treat spinal hemangioma? – information collection is required.
The doctor takes into account and evaluates several factors:
- The size of the tumor lesion.
- Localization of inflammation.
- The degree of vertebral injury.
- Are nearby tissues affected?
- Presence of complications.
- Patient's condition.
If you are diagnosed with a hemangioma in the vertebral body, treatment begins with an examination, which is aimed at identifying compression fractures of the vertebrae and the rate of tumor development.
Therapy methods:
Ray. A tried and tested method. The effectiveness has been confirmed by numerous studies. The essence: under the influence of rays, tumor cells are destroyed. Its growth stops, which relieves pain in the patient.
It is impossible to apply this method only if the vertebra is severely injured by the tumor. The bone structure is thin and fragile, which is fraught with subsequent fracture.
Embolization. Today this method is not as popular as it used to be. The bottom line: a prepared solution is injected into the vertebral body using a catheter, which should prevent bleeding, and therefore prevent the development of a tumor. The solution is polyvinyl alcohol.
The disadvantage of this method of therapy is quite significant - relapses. There is a high probability of complications that occur due to the solution getting into nearby tissues.
Surgical. They are used extremely rarely and only if the presence of a tumor causes severe pain or neurological disorders.
Only the part of the vertebra that has an irritating or compressive effect is subject to removal. After surgery, radiation therapy is carried out for a fairly long period.
With the surgical method, there is a high probability of bleeding and recurrence of spinal hemangioma. Treatment of children by surgical removal of the tumor is justified by harm caused by X-rays to the growing body.
- Sclerotherapy. Alcohol is injected into the damaged vertebra, which promotes narrowing and gluing of blood vessels. The bad news is that the damaged vertebra is susceptible to fracture.
- Vertebroplasty. The most gentle and popular method of therapy. The bottom line: a cementing solution is injected into the vertebral body using puncture. Filling the cavity helps stop bleeding and tumor growth. Hardened medical cement increases the strength of the vertebra. Low trauma facilitates rapid rehabilitation of the patient.
Manifestations of spinal hemangioma
Symptoms of the tumor depend on its size and location in relation to the vertebral body. For a long time, the tumor proceeds hidden, without causing any concern. An asymptomatic neoplasm is detected accidentally during examinations in connection with injury or other pathology of the spinal column.
The earliest sign of a growing hemangioma is pain, which is initially mild and occurs periodically. As the tumor grows, the intensity of the pain increases and it becomes unbearable. Dangerous tumor sizes (over 1 cm) contribute to the progression of not only pain, but also neurological disorders associated with disruption of the vertebral structure and compression of the spinal cord.
For small tumors, the pain is moderate, most often bothers patients at night or after physical activity, and is localized to the area of the affected vertebra. When spinal cord structures are involved, numbness, paresis and paralysis, and dysfunction of the pelvic organs are possible.
Hemangioma of the thoracic spine manifests itself:
- Pain in the area of the affected vertebra;
- Feeling of numbness in the limbs;
- Paresis and paralysis (rarely);
- Disturbances in heart rhythm, digestive system function, and disorders of the pelvic organs.
If the cervical spine is affected, blood flow in the brain may be impaired, resulting in headaches, decreased mental performance, insomnia, dizziness, hearing and vision impairment.
The lumbar region ranks second in frequency of lesions. With hemangioma of this localization (l1, l2, l3, l4) the following are possible:
- Pain in the lower back, groin, hips;
- Numbness in the limbs;
- Paresis and paralysis of the legs;
- Dysfunction of the pelvic organs (especially with damage to l3-4).
In adults, in addition to the described neurological symptoms, signs of aggressive hemangioma may include infertility and impotence.
Hemangioma with an aggressive course can provoke very serious complications - compression fractures of the vertebral bodies, compression of the spinal cord and its roots, when paresis, paralysis and dysfunction of internal organs can become persistent and irreversible. To prevent this from happening, if the symptoms described above appear, you should consult a specialist.
Diagnosis of hemangiomas involves:
- X-ray examination of the spine in different projections is the simplest, cheapest and most accessible method.
- CT.
- MRI allows you to determine not only the extent of damage to the vertebra, but also the surrounding soft tissues.
spinal hemangioma on a diagnostic image
Diagnosis of vertebral hemangiomas
Before the introduction of magnetic resonance and computed tomography methods into medical practice, hemangiomas in the spine were detected during X-ray examination as a light spot against the background of the vertebral body, i.e. they gave signs of bone loss. There were no other signs, especially specific ones. Therefore, it is extremely rare for patients to be diagnosed with vertebral hemangioma during their lifetime.
The exception was cases when a vascular tumor provoked fractures of the vertebral bodies. In such situations, its presence was detected during the operation. During the surgical intervention, material was selected for histological examination, on the basis of which a diagnosis of “vertebral hemangioma” was made after the fact.
Today, it is possible to detect a vertebral hemangioma, assess its size and location features with high accuracy using MRI and CT. Since such formations do not manifest themselves in any way until complications arise, vertebral hemangiomas are still most often an incidental finding during an MRI, CT or X-ray (also requiring subsequent confirmation using magnetic resonance or computed tomography). But when they are detected, regardless of size, they require monitoring.
If the hemangioma shows signs of growth or the first study reveals a high risk of complications, this is regarded as an indication for surgery.
Symptoms of the disease
If the tumor is located in the thoracic region, a person may have numb hands
Many neoplasms, including hemangioma in the th11th vertebral body, may not manifest themselves for a long time. Among the first signs that are often attributed to fatigue are:
- the appearance of discomfort in the spine after physical activity;
- weakness and numbness of the arms and legs due to the pathology in the thoracic region;
- later, digestive disorders develop;
- gallstones appear;
- arrhythmia may occur;
- Women often develop infertility, but this mainly concerns neoplasms of the lumbar region.
Symptoms of hemangioma of the cervical vertebrae are usually associated with constant headaches, insomnia, dizziness, decreased hearing and vision.
The symptoms of the tumor lead to severe neurological problems if it is located in the thoracic region. It all starts with weakness and can develop into acute pain. This symptom is caused by compression of the nerve roots and impaired sensitivity.
Types of hemangioma development
The aggressive type develops quickly and causes pain in the thoracic region
Symptoms of a neoplasm largely depend on the characteristics of the disease:
- non-aggressive hemangioma - does not cause any symptoms for a long time, is often discovered only after the death of the patient, but can be detected accidentally with MRI and CT;
- aggressive tumor – develops quickly, often causes pain and leads to disruption of body functions.
The first type of tumors is guaranteed not to degenerate into malignant ones, as it develops too slowly. The second one is more prone to this process. However, there is no need to worry: hemangiomas degenerate into cancer less often than in 5% of cases.
Puncture vertebroplasty
A real breakthrough in the treatment of vertebral hemangiomas was the use of puncture vertebroplasty, proposed by French doctors. The essence of the method is to introduce into the vertebra a special cementing substance mixed with barium sulfate (a radiopaque agent) and titanium.
In this case, several goals are achieved at once: the tumor shrinks and stops growing, the vertebral body is stabilized with bone cement and compacted, and the risk of fracture is minimal. Puncture vertebroplasty is considered the method of choice for vertebral hemangioma, especially in cases of aggressive tumor progression. It is possible as the main method of therapy or as part of a combination treatment.
We advise you to study - Back pain in the lumbar region
Hemangiolipoma in the vertebral body: what is it, treatment
With vertebral hemangiolipoma, this can be found out in detail from the doctor who made the diagnosis, but often patients try to independently find out the details of the disease, the causes and symptoms of vertebral lipoma, and also understand the principles of diagnosis and treatment. The term hemangiolipoma is used for benign formations in the vertebral area. A tumor appears when there is a malfunction in the vessels of bone tissue.
If any tumor is dominated by adipose tissue, then it is a lipoma; in the case where there is more vascular tissue, the disease is called hemangioma. When vascular and adipose tissue grow simultaneously, hemangiolipoma occurs.
Since without examination it is impossible to determine exactly what tissue the tumor consists of, it can tentatively be called either a hemangioma or a lipoma in the spine.
Hemangiolipomas, in addition to the vertebrae, can be localized in organs and tissues.
What is spinal hemangiolipoma?
Spinal hemangiolipoma is a benign tumor. It develops inside the spinal column. In their structure, they are fatty tissues, inside of which there are many blood vessels. Localized in the spine, in one of the sections.
This disease affects people after 30 years of age. Many doctors say that the cause is aging, so it is really difficult to insure against such a tumor.
The tumor is dangerous because in the first stages of growth it practically does not show symptoms. Often people begin to realize that something is wrong with them when pain occurs. For some, the appearance of such a neoplasm prevents them from moving normally. Since the growth proceeds quietly, it is noticed when it poses a real danger to the spine - a fracture of the vertebra and injury to the spinal cord occurs.
Such growth belongs to the category that does not pose a danger in terms of changing to malignant, therefore the risk of metastases is eliminated.
Diagnosis of the disease
Since the pathology has a benign course, a general blood test will not reveal its presence.
Therefore, in order to detect, it is necessary to resort to instrumental diagnostic methods, which include:
- X-ray;
- MRI;
- X-ray contrast study;
- CT scan.
This method involves placing the patient in an area of a magnetic field. The ability of molecules in the human body to change their charge helps the device’s sensors take pictures of the damaged organ from different angles and sections.
MRI is distinguished by the ability to accurately visualize the soft tissues that make up the hemangiolipoma and the ability to evaluate:
- The location of the tumor relative to the vertebra;
- Dimensions;
- Involvement of the tissues that surround it;
- The condition of the vessels suitable for the neoplasm;
- Changes in bone structure.
Based on these indicators, the specialist will choose the most preferable treatment method.
Diagnostics
If you experience periodic back pain, you need to find out the cause. In 9 cases out of 10, the cause of pain lies in the spine, so the diagnosis of the spinal column should be carried out as carefully as possible.
Diagnosis begins with imaging methods that can reveal degenerative-dystrophic changes in the spine.
For an initial examination, you should make an appointment with a therapist. Based on the nature of the pain and examination of the spinal column, the general practitioner will make a preliminary diagnosis, prescribe an x-ray and refer you to a specialist (vertebrologist or neurologist).
An X-ray allows you to understand the general condition of the spinal column, deformation, the presence of a fracture and the degree of damage to bone tissue. But it is impossible to assess the condition of the spinal cord, muscles, and nerve fibers.
Based on the results of the examination and x-ray, the vertebrologist will determine the general picture of the condition of the spine. A neurologist diagnoses the disease when it spreads to soft tissues (muscles, spinal cord, nerve fibers).
If radiography is not enough to determine the cause of pain, then computed tomography (CT) is performed, which evaluates the density of soft tissues layer by layer. But a simple CT scan may not detect all types of tumor. The most accurate types of CT are represented by spiral CT (SCT) and multislice CT (MSCT), which capture the slightest changes in the structure of tissues and blood vessels.
And they can detect the early stages of emerging pathological processes. To determine the pathology of a benign tumor, a CT scan with contrast is usually performed. Contrast is used to clearly distinguish hemangiolipoma from malignant tumors (osteosarcoma, osteoma and metastases).
Magnetic resonance imaging (MRI) shows more clearly the tissues located behind the bones: the brain and spinal cord, intervertebral discs, and pelvic organs. Using MRI, not only the location of the tumor in the vertebra is assessed, but also the degree of involvement of surrounding tissues in the tumor process, the condition of blood vessels and changes in bone structure.
If the diagnosis is uncertain, consultation with a neurosurgeon may be required. A comprehensive study will allow you to correctly establish the diagnosis. Based on this, treatment is prescribed or a decision is made to perform surgery.
Price
- X-rays in clinics can be done free of charge under the compulsory medical insurance policy.
- A CT scan of individual sections costs 1,200 – 12,000 rubles, of the entire spine from 7,000 rubles.
- MRI of the spine 2,500 – 20,000 rubles, the entire spine 6,000 – 44,000 rubles.
Diagnostic methods
When you know what it is, vertebral hemangiolipoma, it’s time to talk about diagnostic methods. Modern equipment helps to identify tumors in the early stages.
The most effective method is MRI of the spine with contrast enhancement. The doctor also studies the patient’s medical history, listens to his complaints and decides which department should be examined first. Since iodine-based contrast is introduced into the circulatory system, the neoplasm becomes clearly visible on the image. A magnetic resonance imaging scanner takes images of successive sections of your tissues and bones, which helps track the disease even at the earliest stages of its development.
What is it, a hemangioma in the vertebral body
Hemangioma is a benign vascular neoplasm consisting of endothelial cells that have a tendency to proliferate, that is, to multiply.
In very rare cases, diagnosticians identify hemangioma in two segmental components of the spinal column. A neurological anomaly (vertebral body hemangioma) can remain invisible for a long time, without causing discomfort to the owner. However, the very presence of a tumor requires therapeutic treatment of vertebral hemangioma, since foreign growth contributes to structural destruction, increased joint fragility, instability fraught with displacement, the risk of fracture and other disorders of the articular surface of the spinal column.
The most common location of damage to the vertebral body is the Th12 thoracic vertebra and/or L1-L14 lumbar vertebra. However, a vascular neoplasm can occur on any part of the spine. Depending on the degree of growth, aggressive and non-aggressive hemangiomas of the spinal bodies are determined.
Let's consider the main pain symptoms when a particular spinal area is affected.
Painful signs and symptoms of thoracic hemangioma, manifested in the most common areas of the spinal column - Th2, Th9, Th10, Th11 and Th12 vertebrae:
- difficulty bending and turning the body, resulting in discomfort and pain;
- heart rhythm disturbance;
- when you breathe, there is pain in the back;
- the general condition of the chest causes nervousness and psychological discomfort in a person.
Hemangioma of the cervical spine, as the most mobile articular segment of the spine, responds more sensitively to tumor growth. The less active seventh vertebra C7 of the cervical region, articulating with the first vertebra of the thoracic region, is the most vulnerable from the point of view of neurological pathology. Therefore, hemangioma of the cervical vertebra in this area is the most problematic area for therapeutic measures. Possible consequences of a tumor-like lesion of one of the seven cervical vertebrae:
- constant attacks of headache;
- inability to clearly coordinate neck movements;
- blood flow to the brain is disrupted;
- the functioning of the hearing and/or visual system deteriorates.
Hemangioma of the cervical spine not only limits the motor activity of the neck, but also leads to swelling, vascular constriction and decreased mental performance.
It is possible to treat hemangioma L1, L2, L3, L4 and L5 of the lumbar vertebrae only after a thorough differentiated instrumental examination, since pain symptoms in these areas of the spine are very similar to other signs and symptoms of neurological diseases, for example, osteochondrosis or lumbar hernia. sacral section. Affecting the second, third, fourth lumbar and/or L5 - S1 sacrolumbar regions, hemangioma localized in these places causes various pain symptoms, for example, numbness of the lower extremities, functional blocking of the hip joint, paresis, and so on. However, pain in the lumbar spine remains a constant and classic symptom, which affects the general physical condition of a person. Often the cause of intimate restriction in men is a tumor-like neoplasm in the lumbar segment of the spinal frame. Persistent formation and growth of a neurological abnormality can have unpleasant consequences for health, and sometimes irreversible.
We advise you to study - Curvature of the lumbar spine
Causes of hemangioma formation
Today, the true causes of the appearance of vascular tumors are not yet known. They are often congenital and caused by hereditary factors. In such situations, formation is formed at the stage of intrauterine development or immediately after birth. The presence of hemangiomas of any location in close relatives increases the risk of their formation up to 5 times.
In rare cases, newborn children are found to have 3 or more hemangiomas visible to the naked eye on the skin, which is good reason to believe that they are also present in internal organs, including the vertebrae. In such cases, hemangiomatosis is diagnosed.
It is believed that hemangiomas can also occur during life, i.e., be acquired, but the mechanism of their formation is not yet clear. It is known for sure that the tumor is formed from endothelial cells lining the inside of blood vessels, and the action of sunlight is considered as a factor that provokes their excessive growth. But this assumption does not yet have convincing evidence. According to some data, tissue hypoxia, high levels of estrogens (female sex hormones) and spinal injuries are regarded as risk factors for the formation of benign vascular tumors.
It is believed that vertebral hemangioma is a consequence of congenital inferiority of the walls of the blood vessels of a particular vertebra. Therefore, increased stress on it, injuries and other factors provoke minor hemorrhages. In places where blood vessels are injured, blood clots form, and cells that destroy bone tissue, called osteoclasts, are activated. In this area, new vessels are formed that have a defective wall. This is how the vascular tumor begins to increase in size.
In most cases, vertebral hemangioma is an incidental finding during an examination for another reason (most often when there is a suspicion of intervertebral hernia). But the level of development of modern medicine does not yet allow us to say for sure whether it was formed a year ago or still at the stage of intrauterine development. Be that as it may, the time of hemangioma formation is not so important for developing a strategy for further behavior.
Vertebral hemangiomas occur with equal frequency in men and women. They are found in every 10th person, most often in people 20–30 years old. Since there is no objective data yet on what factors cause the formation of a vascular tumor, it is believed that every person can experience this disease.
In 60–80% of cases, hemangiomas are found in the vertebrae of the thoracic spine, most often in the 7th . Less commonly, they are detected in the lumbar vertebrae, and in only 1% of people such benign vascular tumors grow in the vertebrae of the cervical spine. It is extremely rare to have more than one, however, there are cases where hemangiomas are present in 2-5 different vertebrae.
Causes and types of hemangiomas
Hemangioma is a vascular tumor, which is a tangle of intertwined and altered vessels of various types. Damage to the vertebral bodies is usually observed, but tumor growth is also possible in the cartilaginous layers.
typical location of hemangioma in the spine
Initially, defective vessels of the vertebra form a tumor inside it. Under the influence of injuries or heavy stress, hemorrhages and thrombosis occur; the spilled blood stimulates osteoclast cells to “cleanse” the damaged area, and then the vacated space is filled with new defective tumor vessels. This process occurs continuously, leading to the growth of the tumor. The size of vertebral hemangioma rarely exceeds 1 cm.
The causes of vertebral hemangiomas can be:
- Hereditary predisposition;
- Female;
- Vertebral injuries.
It has been established that if you have close relatives suffering from vascular tumors of the spine, the risk of hemangioma increases up to five times. This may be due to hereditary failure of the vascular walls, which contributes to neoplastic transformation.
The role of estrogens in tumor formation is evidenced by the more frequent occurrence of pathology in women, who become ill several times more often than men. In addition, during pregnancy, especially in the third trimester, there is an intense increase in the tumor not only due to altered hormonal levels, but also due to the increasing load on the spine.
Injuries and excessive stress can contribute to increased growth of the vascular component and the formation of a tumor. Moreover, if a hemangioma already exists, then repeated mechanical impacts enhance its growth.
examples of spinal hemangioma growth
Depending on the nature of the flow, there are:
- Aggressive hemangioma;
- Non-aggressive.
An aggressive course is indicated by a rapid increase in the size of the tumor, severe symptoms in the form of compression syndrome, and pathological fractures of the vertebrae. Every tenth detected tumor turns out to be aggressive.
Non-aggressive hemangiomas have a relatively benign course, grow slowly and asymptomatically, and in rare cases of small tumors they may even spontaneously resolve.
Depending on the extent of the lesion, the hemangioma can be limited only to the vertebral body, the posterior semi-ring, the entire vertebra, and epidural growth over the pia mater is also possible.
The histological structure allows us to distinguish different types of neoplasms:
Capillary - built from small vessels of the capillary type and is usually benign in flow;
Cavernous – represented by vascular cavities filled with blood, occurs with intense pain and a high risk of pathological fracture; Mixed.
Symptoms
Often, spinal hemangioma develops without any clinical manifestations - it may turn out to be an accidental finding during examination in connection with some other pathologies or traumatic injury to the spine.
But in some patients the clinical picture is still observed. It is based on the following features:
- pain;
- symptoms of irritation of the spinal cord and nerve roots.
Pain occurs in about 10-15% of patients diagnosed with spinal hemangioma. The characteristics of pain are as follows:
- by localization - in the vertebral region or in the paravertebral (paravertebral) zone;
- by distribution - they can irradiate (give off) to neighboring soft tissues;
- by character - mostly dull, aching;
- in terms of severity – tolerable;
- by occurrence - they begin to bother you at a certain size of the tumor (when it irritates the pain receptors of the periosteum and posterior longitudinal ligament), intensifies at night and after physical activity.
Important
With a spinal hemangioma, symptoms of irritation of the spinal cord and nerve roots arise due to the pressure of this tumor on them.
Spinal hemangioma itself is a benign tumor, but in 3-4% of cases its aggressive growth is noted. This means that, as it grows, it puts pressure on bone tissue; such pressure leads to a significant decrease in bone strength, which causes pathological fractures to form. In this case, the following may also develop:
- sensory disturbance;
- paresis of various types - decreased muscle strength;
- paralysis - lack of muscle activity;
- disorders of the pelvic organs.
There are four types of spinal hemangiomas:
- asymptomatic non-aggressive – clinical and radiological signs of tumor aggressiveness do not appear;
- symptomatic non-aggressive - there are clinical manifestations of aggressiveness, but without radiological signs;
- asymptomatic aggressive - radiological signs of aggressiveness appear, but there is no clinical picture;
- symptomatic aggressive - both clinical and radiological signs of aggression develop.