Spinal stenosis (narrowing) at the level of the cervical spine is a condition that can lead to compression of the spinal cord or nerve roots and disruption of their function, which is accompanied by corresponding symptoms (within the framework of cervical radiculopathy or cervical myelopathy).
Spinal stenosis can occur due to spondylosis (degenerative changes in the cervical spine), as well as due to trauma (fractures and instability), inflammatory processes, intervertebral hernias and tumors.
Anatomy
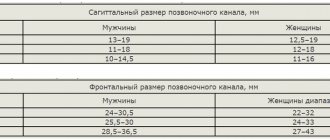
Normally, the spinal canal has enough space for all neural structures. The diameter of the spinal canal depends on the level and individual characteristics. For example, the height of the body of the third cervical vertebra (C3) is about 21.8 mm and the spinal cord occupies about 50% of the spinal canal. The height of the C6 vertebral body is 17.8 mm and the spinal cord occupies about 75% of the spinal canal.
Lee et al. described the mean anterior-posterior distance within the spinal canal (and acceptable deviations) in all samples and at all levels. It is 14.1 +/- 1.6 mm. The minimum diameter is 9.0 mm, maximum 20.9 mm, average 14.4 mm. In men, the diameter of the spinal canal at all levels is greater than in women.
Although congenital narrowing of the spinal canal is possible, most often the stenosis is acquired. It is formed as a result of progressive degeneration of the intervertebral disc, which may be accompanied by the formation of protrusion, ventral osteophytes, thickening of the ligamentum flavum and hypertrophy of the facet joints.
Meyer et al. described how movements change the diameter of the spinal canal and spinal cord. The diameter of the spinal canal decreases with flexion and extension. During extension, the ligamentum flavum forms folds, which leads to a narrowing of the spinal canal. In addition, changes in the length of the spinal cord also affect the diameter of the spinal canal. For example, shortening of the spinal cord during extension results in an increase in the diameter of the spinal canal. If spinal stenosis occurs, the spinal cord may be damaged during movement. It can be compressed between the posteroinferior part of one vertebral body and the arch or ligamentum flavum of the underlying segment. This mechanism causes not only damage to the spinal cord, but also to the vessels that supply it. Firstly, the anterior spinal artery may be compressed, and secondly, compression of the spinal cord leads to twisting of the transverse grooves in which other arteries lie. These vessels supply the gray matter and medial white matter, which are primarily affected.
Cost of surgery for stenosis
In Russia, the price of spinal surgery varies widely. The price of the operation depends on its complexity, the level of the medical institution and the qualifications of the specialists working there.
Decompressive laminectomy in Moscow clinics costs 25,000-50,000 rubles, discectomy – 18,000-60,000 rubles, transpedicular fixation of the vertebrae – 40,000-65,000 rubles, interbody fusion – 35,000-70,000 rubles. As for dynamic stabilization, in Russia it is performed only in some medical institutions, and it costs much more than stabilizing operations.
As we have already found out, with spinal stenosis, patients require decompression and fixation of the spine. To achieve this, you need to do several manipulations at once. Naturally, surgical intervention will not be cheap for the patient. At the same time, he will have to pay for the examination, consultations with the necessary specialists, anesthesia, the cost of consumables and implants.
Residents of the CIS are increasingly going abroad for surgery. The quality of medical care there is higher, and treatment does not cost much more. In the Czech Republic, you will undergo surgery and complete rehabilitation for just one euro. As for other countries that are so popular among our fellow citizens, prices there are slightly higher. In Germany, surgery without rehabilitation costs 14-18 thousand euros, in Israel – 16-20.
Epidemiology
Spinal stenosis is quite common. It has been estimated that in the adult population, cervical spinal stenosis occurs in 4.9% of people, of which 6.8% are people 50 years of age or older, and 9% are people 70 years of age or older. For most patients, symptoms worsen with age. The deterioration sometimes increases quickly and is irreversible. 75% of people suffer from neurological deficits. There is evidence that about 5% of people who do not have symptoms of spinal cord compression worsen each year. There are also patients with acute disease. As a rule, these are people with pronounced but asymptomatic stenosis, which begins to appear after a minor injury.
Spinal stenosis most often leads to spinal cord myelopathy in people aged 50+ years.
Prevention
To slow down the progression of the disease, you should choose the right special exercises.
Every day you should do exercises, dedicating at least 30 minutes to it. Aerobic training (in the form of swimming or walking) is recommended. Proper control of your body and good posture should become a habit.
Examples of treatment of stenosis at the A.N. Center for Pathology and Neurosurgery Baklanova
Clinic
Cervical stenosis does not always cause symptoms, but when they do occur, they are always associated with cervical radiculopathy or cervical myelopathy. The following symptoms may occur:
- pain in the neck and arms; - dysfunction of arms and legs; - weakness, stiffness or clumsiness in the hands; - weakness in the legs; - walking impairment; - frequent falls; - increased urge to urinate, which can lead to incontinence; - violation of proprioception.
The progression of the disease can occur in different ways:
- slow and constant deterioration; - deterioration to a certain point and stabilization; - rapid progression.
Features of surgical treatment of complicated stenosis
In cases of spinal stenosis combined with spinal instability, the use of decompression or interspinous fixation systems alone is unacceptable. Surgical interventions will lead to even greater loosening of the spinal motion segments and aggravate the patient’s condition. In this case, the installation of front or rear stabilizing systems is considered optimal.
Titanium stabilizer.
If there are IVD hernias, a person undergoes a microdiscectomy or a classic discectomy. The first operation is usually supplemented with the installation of interspinous spacers, the second - with stabilization of the spine with a titanium cage.
Diagnostics
X-ray is not informative enough to confirm spinal stenosis, but can be used to exclude other pathologies. Stenosis can occur at one level or at several levels simultaneously, so the use of magnetic resonance imaging is justified. MRI clearly visualizes stenosis and compressed spinal cord. Computed tomography (CT) is informative regarding bony narrowing of the spinal canal and can be used in combination with myelography.
If the spinal cord or spinal roots are not compressed, then stenosis in the cervical spine may exist asymptomatically (for the patient). However, if you conduct a complete neurological examination, you can identify some neurological symptoms:
— hyperreflexia: increased tendon reflexes (knee and Achilles); - changes in gait (awkwardness or imbalance); - loss of sensation in the arms and legs; - Babinsky's symptom; - Hofmann's symptom.
Causes of development of spinal canal stenosis
People who have crossed the age of 50 are more often susceptible to pathology. If stenosis is diagnosed earlier, the cause is a congenital malformation in one or more vertebrae. Stenosis in this case is defined as primary. Secondary stenosis is caused by:
- arthrosis of the facet joints;
- growth of osteophytes;
- changes in the ligamentum flavum in the form of compaction;
- protrusion;
- injuries;
- epiduritis;
- lipomas;
- spondylolisthesis;
- spondylosis;
- osteochondrosis.
Treatment
Surgical treatment
For patients who have increasing weakness, pain, or gait disturbance, surgery may be recommended. Options for stenosis at several levels may be as follows:
Anterior access:
— anterior cervical discectomy with spinal fusion; — anterior cervical corpectomy with spinal fusion; - their combinations.
The disc or bone that is compressing the spinal cord is removed from an anterior approach, and then the spine is stabilized. It involves the use of an implant, which is installed between two adjacent segments to support and compensate for the defect.
Rear access:
- laminectomy without stabilization (removal of a section of bone or ligament); — laminoplasty.
The posterior approach can be accomplished in two ways: direct removal of the offending structures and indirect dislocation of the spinal cord. The choice between the two operations depends on the location of the spinal cord compression, the number of levels of compression, posture, the presence of instability, neck pain, and risk factors for pseudarthrosis formation.
Laminoplasty is more effective than laminectomy without fusion because it reduces the risk of developing perineural adhesion and postoperative kyphosis. Surgeries from the anterior approach and laminectomy with spinal fusion are also less effective than laminoplasty. Laminoplasty protects segments during movement and prevents the development of complications such as implant displacement, the formation of a false joint and damage to adjacent segments.
After the operation, the patient remains in the hospital for several more days. In order for a person to quickly return to an active life, various rehabilitation programs are implemented. For example, a set of therapeutic measures may include exercises aimed at increasing the range of motion in the cervical spine.
Physical therapy
Conservative treatment aims to reduce pain intensity and increase function. It does not change the size of the spinal canal, but can provide long-term pain relief and improved function without surgery. The rehabilitation program may require 3 or more months of treatment under the supervision of a specialist.
The program may include:
- Stretching exercises: These exercises are aimed at restoring the elasticity of the muscles of the neck, torso, arms and legs. — Manual therapy: manipulation of the cervical and thoracic spine to improve and maintain mobility. — Heat therapy: microcirculation in muscles and soft tissues improves. - Cardio Exercise: It also improves blood circulation and increases the patient's cardiovascular endurance, ensuring good physical fitness. — Hydrokinesitherapy: it will allow your body to move without putting stress on the spine. – Training to increase daily physical activity and functional movements.
Exercises and techniques that can reduce symptoms of stenosis and prevent progression of the disease:
— Specific exercises to strengthen the muscles of the arms, torso and legs. - Stretch marks. — Exercises to correct posture. — Exercises to stabilize the scapula. — Recommendations for ergonomics to avoid harmful positions. — Planning your daily routine: you take breaks during daily activities such as walking or working in your garden. — Recommendations regarding “how to lift, push and pull correctly.”
Colleagues, we remind you that this weekend a seminar by Georgy Temichev “Neck pain and headaches” will be held in Moscow.
Decompression surgery of the cervical spine
Surgical interventions on the cervical spine can be performed through an anterior or posterior approach. In the first case, the surgeon “makes his way” from the spine through the tissue spaces of the neck, in the second, he cuts through the soft tissues from the back.
Anterior access.
Indications for operations with anterior access:
- kyphosis;
- MRI-verified anterior compression;
- the extent of stenosis is no more than 2 vertebrae;
- severe spinal instability.
During surgical interventions, doctors perform discectomy and spinal fusion. If there are no contraindications, they can install a dynamic DCI implant in place of the IVD. Surgeries with anterior access are traumatic and lead to the development of complications.
Surgical interventions with a posterior median approach are less invasive and safer. During these procedures, the specialist performs a laminectomy or laminoplasty. If necessary, he performs spinal fusion. The surgeon can use a variety of structures to fix the vertebrae.
Indications for operations with posterior access:
- the presence of extended posterior compression;
- cervical lordosis;
- identification of ossification of the posterior longitudinal ligament;
- congenital stenosis.
In case of osteoporosis, ligamentous insufficiency and a high probability of developing pseudarthrosis, doctors prefer operations with a posterior surgical approach.
Source
Meyer F, Börm W, Thomé C. Degenerative cervical spinal stenosis: current strategies in diagnosis and treatment. Deutsches Ärzteblatt International. 2008 May;105(20):366. Lee MJ, Cassinelli EH, Riew KD. Prevalence of cervical spine stenosis: anatomic study in cadavers. J.B.J.S. 2007 Feb 1;89(2):376-80. João Levy M., António Fernandes F., João Lobo A. “Neurologic aspects of systemic disease part I.” Handbook of clinical neurology: Chapter 35- Spinal Stenosis (2014) Volume 119; pg 541-549 North American Spine Society Public Education Series. Cervical stenosis and myelopathy. https://www.spine.org/Documents/cervical_stenosis_2006.pdf(Accessed November 22, 2011). Williams SK, et al. Concomitant cervical and lumbar stenosis: Strategies for treatment and outcomes. Semin Spine Surg 2007;19(3):165-176. Congenital stenosis of the cervical spine: Diagnosis and management. J Natl Med Assoc 1979;71(3):257-264. L. Yang et Al., Plate-only Open-door Laminoplast Versus Laminectomy and Fusion fortification Treatment of Cervical Stenotic Myelopathy, Healio Orthopedics, Vol. 36, January 20132 Yeh et Al., Expansive open-door laminoplasty secured with titanium miniplates is a good surgical method for multiple-level cervical stenosi, Journal of Orthopedic Surgery and Research, August 2014 Chikuda et Al., Optimal treatment for Spinal Cord Injury associated with Cervical canal Stenosis(OSCIS): a study protocol for a randomized controlled trial comparing early verus delayed surgery, BioMed Central, 2013. Y. Yukawa et Al., Laminoplasty and Skip Laminoplasty for Cervical Compressive Myelopathy, Spine, 2007 May, S . & Comer, C. Is surgery more effective than non-surgical treatment for spinal stenosis, and which non-surgical treatment is more effective? A systematic review. Physiotherapy, 2013, 99(1), 12-20 Hu SS, et al. Cervical spondylosis section of Disorders, diseases, and injuries of the spine. In H. B. Skinner, ed., Current Diagnosis and Treatment in Orthopedics, 4th ed., pp. 238–242. New York: McGraw-Hill., 2006 Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res 2006; 443:198.
Symptoms
The space inside the spinal canal may be narrowed and there may be no symptoms. However, if the narrowing puts pressure on the spinal cord, cauda equina, or nerve roots, then symptoms appear that slowly progress. The neck or lower back may or may not hurt. More often, patients experience numbness, weakness, cramps, or generalized pain in the arms or legs. If the narrowed area puts pressure on the nerve root, patients may experience pain radiating down the leg (lumbosacral sciatica). Squatting or flexing the spine can reduce pain symptoms (when flexing, there is an increase between the vertebrae in the spine. This is why spinal flexion exercises are recommended, along with weight training exercises.
Patients with more severe stenosis may have problems with their bowel, bladder, or lower limb function. For example, cauda equina syndrome is a fairly rare but very serious type of spinal stenosis. Cauda equina syndrome occurs due to compression on the structures of the cauda equina, and symptoms may include loss of bowel control, bladder control, erectile dysfunction, or pain, weakness, and sensory loss in the lower extremities. Cauda equina syndrome is a medical emergency.
How is cervical artery stenosis treated?
Stenosis of the cervical arteries is treated using conservative methods (physiotherapeutic procedures and medications) and surgical intervention.
Conservative treatment
The course of treatment is selected for each patient, taking into account the characteristics of his condition:
- painkillers (NSAIDs) with analgesic and anti-inflammatory effects;
- injections of hormonal agents into the spine to reduce swelling, tissue compression and pain;
- diuretics to reduce cerebrospinal fluid pressure and relieve swelling;
- electrophoresis with novocaine to relieve pain in the affected area;
- magnetic therapy to reduce swelling and relieve pain;
- when the muscle frame is tense, massage is used;
- physical therapy – special exercises for stenosis help strengthen the cardiovascular system, arm and neck muscles;
- manual therapy;
- acupuncture;
- spinal traction.
Surgical treatment
Surgical methods are used if a conservative approach does not provide a lasting effect or the development of the disease calls into question the patient’s life and ability to work. Today there are many methods of surgical treatment, but three operations provide maximum effectiveness:
- decompressive laminectomy - an operation to remove a structure that causes a narrowing of the canal (hernial protrusions, tumors, intervertebral discs and arches, osteophytes;
- installation of stabilizing systems;
- installation of an implant after removal of the affected fragment.
Forms and varieties of the disease
Stenosis is classified according to several indicators. First of all, in accordance with anatomical criteria. This is discussed in the following table.
Table. Anatomical classification of stenosis
| Types of disease | Description |
| Central stenosis | Characterized by a significant change in the size of the spinal canal. There may also be a decrease in the clearance between the posterior plane of the vertebra and the closest opposite point located on the arch. Additionally, the central type of stenosis is classified into relative (the size of the mentioned gap is less than 1.2 cm) and absolute (decreases to 1 cm and beyond) forms. |
| Lateral stenosis | The size of the canal and intervertebral foramen is reduced to 4 mm or even more. |
The second common classification is based on the causes of stenosis. More details in the table.
Table. Classification according to causes
| Causes of the disease | Explanations |
| Disturbances in the processes of formation and further development of the skeleton | They progress against the background of congenital pathologies of the spine. |
| Degenerative changes | The disease progresses against the background of various ailments accompanied by degenerative-dystrophic disorders. An example is the final stages of a disease such as osteochondrosis. |
| Acquired non-degenerative causes | In such conditions, stenosis develops as a complication of other diseases, as well as against the background of previous injuries. |
| Combined reasons | Combinations of any of the above provoking factors. |