- Home >
- Directory >
- Spinal abnormalities
It's a strange situation!
If you've been looking for information about spinal abnormalities, you've probably noticed this. Finding complete, structured material on this topic is a problem, isn’t it? Very uncomfortable. You are interested in this issue, which means you need this information. Moreover, spinal abnormalities are very serious diseases. 12% of children are born with congenital defects of the spinal column. This is a very high percentage!
Let's organize all the necessary data in one article so that you can get a clear picture of the problem without wasting time searching for information. We will tell you the most important things, conduct something like a free consultation, providing answers to all the questions that you might have.
So, we have a problem - anomalies in the development of the spinal column. We will deal with it.
If you have any questions, ask our specialist! Ask a Question
Types of congenital spinal anomalies
All spinal anomalies formed in utero are divided into two large groups - ontogenetic and phylogenetic origin.
There is also a third group of mixed defects of ontophylogenetic origin.
1. Types of congenital vertebral deformities associated with ontogeny disorders
These types of vertebral anomalies are the cause of severe forms of congenital scoliosis.
- Defects associated with underdevelopment, decrease or increase in the number of vertebrae:
- Microspondylia.
- Asymmetrical vertebra.
- Flattened vertebra.
- Additional wedge-shaped vertebrae and hemivertebrae.
- Posterior wedge-shaped vertebrae.
- Fusion (partial or complete) of two or more adjacent vertebrae in any part.
- Short neck syndrome is a fusion and abnormal development of the cervical and sometimes also thoracic vertebrae (due to a genetically determined pathology that is inherited. Another name for the pathology is Klippel-Feil syndrome).
- Butterfly-shaped vertebrae.
- Spina bifida.
- Developmental anomalies or absence of part of the arch, spinous processes, spondylolysis, spondylolisthesis. Nonfusion of the arches and vertebral bodies.
2. Types of congenital spinal anomalies associated with phylogenesis disorders
- Partial or complete lumbarization (the first sacral vertebra is separated from the sacrum), sacralization (the fifth lumbar vertebra is fused to the sacrum), occipitalization (fusion of the first cervical vertebra and the occipital bone).
- Transitional seventh cervical or first thoracic vertebrae, which are characterized, respectively, by an increase or decrease in the number of ribs - accessory cervical ribs syndrome).
- Any other types of increase or decrease in the number of vertebrae.
3. Congenital spinal defects of combined origin (ontophylogenetic)
Principles of treatment
Treatment of spinal abnormalities started too late is always tantamount to the need to use surgical techniques. This should be avoided while possible.
Above, we named eight reasons why you should not delay treatment, and now we will name eight of the most compelling reasons to give preference to conservative treatment (not only you, but also your attending physician will be guided by these facts).
- Reason 1: Painlessness of treatment procedures compared to surgical methods.
- Reason 2: There is no need to use anesthesia, including local anesthesia.
- Reason 3: Low percentage of disease recurrence.
- Reason 4: No complications (secondary infections, adhesions, loss of function).
- Reason 5: The ability to adjust the treatment regimen at any time if the current one is not suitable.
- Reason 6: Treatment on an outpatient basis, without mandatory hospitalization and loss of ability to work.
- Reason 7: There is no need to take a course of antibacterial agents (for operations this is a mandatory measure).
- Reason 8: Ability to avoid the appearance of post-operative scars.
The choice between harmless and dangerous methods is obvious. If you still need surgical treatment, it will be prescribed immediately. Our goal is to improve your quality of life and achieve remission, regardless of what method of therapy needs to be used. We use conservative methods, the effectiveness of which is often higher than the effectiveness of surgical interventions, but if surgery is necessary for recovery, you will know this immediately.
Causes of congenital spinal abnormalities
The etiology of congenital pathologies of the spine is not fully understood, and in many cases the exact cause of the pathology at birth cannot be established.
But it has been established that most often deformities and diseases of the spine occur when:
- Genetic hereditary prerequisites, various gene mutations.
- Disorders of intrauterine development of the fetus for various – exogenous or endogenous – reasons.
- Dietary disorders of the expectant mother, lack of vitamins and microelements, as well as metabolic disorders of the pregnant woman’s body.
- Hormonal disorders in the body of the expectant mother.
- Severe toxicosis, nephropathy, gestosis in pregnant women.
Anatomical features
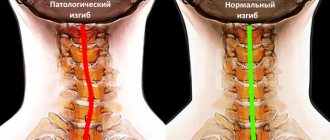
The spinal column includes the cervical, thoracic, lumbar and sacral sections, as well as the coccyx. The most vertebrae are in the thoracic region - twelve, in the cervical region - seven, in the lumbar and sacral - five vertebrae, in the coccyx - from one to three vertebrae.
Between the vertebrae there are strong, flexible intervertebral discs that perform a shock-absorbing function. The vertebrae have processes that, when connected with the processes of neighboring vertebrae, form joints. In the center of the vertebrae there are openings through which a cylindrical cord passes - the spinal cord.
Normally, the spinal column consists of five sections
Diagnosis of congenital anomalies of the spine - can they be identified by symptoms?
Performs diagnostics and makes a diagnosis by a pediatric surgeon or orthopedist.
Diagnostic methods used today:
- X-ray – allows you to determine additional vertebrae or hemivertebrae, irregularities in the shape of the vertebrae, displacement relative to each other, etc.
- Computed tomography (CT) - allows you to more clearly identify bone disorders of the spinal column.
- Magnetic resonance imaging (MRI) – successfully detects disorders of the spinal cord and its structures, as well as the ligamentous apparatus.
In addition, to identify pathologies in the development of the fetal neural tube, prenatal diagnosis is necessary:
- Laboratory tests of a pregnant woman's blood , as well as amniotic fluid, to determine acetylcholinesterase and α-fetoprotein levels.
- Ultrasound screening of a pregnant woman.
We recommend you:
- Manual therapy. This method is most effective when used correctly. Take a look at the graph - it shows the percentage of patients with various spinal anomalies who noted a significant improvement in their well-being after 5-6 manual therapy procedures.
- Therapeutic exercise. Exercises are selected individually: taking into account the fact that the treatment of anomalies is always long-term, a scheme will be developed for you, which you can adhere to even after the end of treatment in the clinic.
- Massotherapy. To achieve a lasting effect, at least 10 procedures are needed. Remember that unprofessional massage (especially with vertebral instability) can only aggravate the disease. Therapeutic massage should be performed by a qualified specialist.
- Reflexology as a means of relief.
- Physiotherapeutic procedures: muscle stimulation, vacuum therapy, electrophonophoresis.
- Fixation of the spinal column using Shants collars and corsets is a necessary component in the treatment of most spinal anomalies.
We do not carry out any procedures without an initial consultation with a specialist who will evaluate the indications and contraindications and select the desired type and frequency of sessions.
The article was reviewed by Doctor of Medical Sciences, Professor Grigory Isaakovich Shvartsman, Northwestern Medical University. I.I. Mechnikov.
Sign up at the MART medical center in St. Petersburg (see map) by phone, or leave a request on the website.
Accessory cervical rib syndrome
Accessory cervical rib syndrome can clinically manifest itself under the influence of unfavorable factors (coldness, trauma, infection). In many cases, additional cervical ribs do not indicate anything about themselves and turn out to be an accidental discovery. Clinical manifestations of accessory cervical ribs are characterized by the presence of neuralgic pain in the shoulder, which sometimes spreads to the entire limb.
Usually there are vasomotor and trophic disorders (pale, cyanotic, cold skin, sweating, increased pilomotor reflex). Sometimes muscle weakness and atrophy occur. The presence of autonomic disorders, as well as in some cases the sympathetic nature of the pain, indicate traumatization of the cervical sympathetic fibers by the accessory ribs.
Split vertebra (spina bifida)
The most common developmental defect that has the greatest practical significance is spina bifida. In the vast majority of observations, clefting consists of non-healing of the vertebral arches. It is extremely rare to observe splitting of the vertebral body itself. Most often, nonfusion of the arches is observed either in the LV lumbar or in the SI sacral vertebra. In other parts of the spine, cleft arches are observed less frequently.
A distinction is made between closed and open vertebral bifida . Closed spinal bifida (spina bifida oculta) is more common. In most cases, closed spina bifida oculta is not accompanied by any neurological disorders. The only exception is bedwetting.
With closed spinal bifida (spina bifida oculta), there may also be mild pain in the lumbosacral region. The resulting scar changes in the area of the roots cause neurogenic disorders: paresis of the legs with loss of tendon reflexes, radicular sensitivity disorders, trophic and vasomotor symptoms (ulcers, swelling, local hypertrichosis, skin changes).
Open spina bifida is much less common (one child per 1000–1500 births) and is a more severe degree of spinal developmental defect. Typically, open vertebral fissures are combined with dysplasia of the spinal cord, membranes and roots. Through the existing splitting of the vertebrae, the substance of the spinal cord and membranes protrude.
Classification
The disease is divided into several groups:
- change in the number of vertebrae: occipitalization (fusion of the first cervical vertebra with the occipital bone), sacralization (fusion of the fifth lumbar vertebra with the sacrum), lumbarization (separation of the first sacral vertebra from the sacrum), fusion of several vertebrae;
- modification of the structure of the vertebrae: wedge-shaped vertebrae (underdevelopment of the vertebrae in the anterior section), spondylolysis (underdevelopment of the vertebrae in the posterior section);
- underdevelopment of individual elements of the vertebrae: anomalies of the vertebral bodies and arches - non-fusion.
Klippel-Feil syndrome
In another way, this abnormal phenomenon is called “short neck syndrome.” Its essence is the fusion (concrescence) of the cervical vertebrae. In some cases, not only the cervical vertebrae are united, but also the upper thoracic ones. The pathology is expressed in the form of a noticeable shortening of the neck, lowering of the hair growth line, and limitation of head movements. A typical sign is the so-called. Proud head posture (head tilted slightly back).
A typical sign of Klippel-Feil syndrome is a short neck.
In some patients, powerful folds of skin are observed from the shoulders to the ears. Klippel-Feil syndrome is often combined with other developmental anomalies of the spinal column (“cervical ribs”), pathologies of the cardiovascular, respiratory and nervous systems, spinal bifida, and cleft palate. There may be no neurological manifestations. When the roots are compressed, sensitivity is impaired, which causes paresis and reduced hand strength.
For pain, analgesics and physiotherapeutic methods are prescribed. This pathology is treated conservatively with the help of exercise therapy and massage, the purpose of which is to improve posture and prevent the development of new deformities. The operation is prescribed for compression of the spinal roots.
Additional cervical ribs
This is a congenital anomaly of the cervicothoracic region. Additional ribs can be two-sided or one-sided. Paired ribs come in different sizes and have different clinical manifestations. The disease attracts attention more often in adulthood. During puberty, vascular or neural symptoms may first appear. In general, the disease has no specific symptoms and is discovered accidentally during an x-ray.
No ads 2
Hypothermia, traumatic factors, and infectious diseases can cause pain, muscle weakness, impaired vascular tone, increased sweating and skin manifestations (pallor, cyanosis of the skin). Some patients are characterized by low shoulders, which visually resemble an extension of the neck. This gives the so-called seal species.
For the purpose of immobilization, a Shants collar is used to secure soft bandages. Physiotherapy, vasodilators (Dibazol), massage, exercise therapy are prescribed. Conservative treatment has no effect when the neurovascular plexus is compressed by the rib. In this case, an operation is performed. The excess rib is removed through the posterior or anterior approach.
Kimmerle anomaly
Kimmerly's anomaly (anomaly of the 1st vertebra) is the presence in the structure of 1st cervical vertebra of an additional bone arch, which limits the movement of the vertebral artery and causes its compression. Patients with this disorder complain of dizziness, unsteady gait, tinnitus, poor coordination, darkening of the eyes, muscle weakness, and syncope (presyncope). Afferent and motor disorders, transient ischemic attacks often occur, and ischemic stroke is possible.
The diagnosis is made after radiography of the craniovertebral junction, magnetic resonance angiography, and ultrasound examination of the vessels of the head and neck.
X-ray is the best way to diagnose Kimmerle anomaly
With such an anomaly in the development of the spine, conservative treatment is allowed. Vascular agents are prescribed to improve cerebral circulation (vincamine, etc.). Under the control of a coagulogram, drugs that improve blood rheological parameters (pentoxifylline) are taken.
Complex treatment also includes nootropic drugs, neuroprotectors, antioxidants, metabolic drugs (piracetam). Removal of the additional bone arch of the vertebra is carried out in particularly serious cases when severe circulatory failure occurs in the vertebrobasilar area.
Spina bifida
This is one of the most common types of spinal disorders. Most often, non-fusion of the arches of the fifth lumbar or first sacral vertebrae occurs. Non-fusion of the arches of the remaining vertebrae and splitting of the body are rarely diagnosed. Spina bifida can be closed or open. Closed clefting is more common. The pathology occurs without visible changes or manifests itself in the form of mild pain in the lumbar and sacral regions.
No ads 3
When scars form in the roots, sensitivity is impaired, and paresis may appear along the innervation of the compressed nerve. Vascular tone and trophism of the skin are disrupted, and ulcers and swelling may occur. The prognosis for a closed form of cleft is usually favorable. With timely treatment, the disease can be defeated at an early stage immediately after the birth of the child.
The main methods of treatment are gymnastics, physiotherapy and massage. The purpose of these measures is to restore the microvasculature of blood vessels and ensure normal growth of the child.
Open spina bifida is rare. The disease is diagnosed in one out of one and a half thousand newborn children. This is a very serious disease, which is accompanied by many other disorders (underdevelopment or pathological formation of the roots and membranes of the spinal cord, spinal cord dysplasia and others). In particularly dangerous conditions, not only the vertebrae are split, but also the spinal cord.
The membranes and substance of the spinal cord protrude through the split vertebra. On the child’s back, at the level of the cleft, there is a hernial protrusion, not covered by skin and muscles. The hernial sac may include only the membranes of the spinal cord (meningocele) or the membranes together with the substance of the spinal cord (meningomyelocele). Large hernias are accompanied by impaired innervation and trophism, and motor dysfunction.
Herniation on the back of a child with spina bifida
Spina bifida and other abnormal spinal conditions are diagnosed through CT scans. Magnetic resonance imaging allows you to assess the condition of soft tissue structures (intervertebral discs, ligaments, spinal cord, etc.). Treatment of the pathology is carried out after the birth of the child. The purpose of surgery is to prevent further damage to nerve tissue and prevent infection.
During the operation performed by neurosurgeons, the spinal column defect must be closed as much as possible: the spinal cord along with the roots is placed back into the spinal canal and covered with the meninges. In some cases, a shunt is installed to drain excess cerebrospinal fluid.
Sacralization and lumbalization
Fusion of the sacrum with the fifth lumbar vertebra and separation of the first sacral vertebra from the sacrum can occur without any symptoms. When the roots are compressed, sensitivity is impaired, paresis and trophic disturbances occur in the innervated area. Both conditions can lead to curvature of the spine, the development of spondyloarthrosis and osteochondrosis, deterioration of blood supply to the spinal column, and limited mobility.
Conservative therapy consists of taking medications, exercise therapy, physiotherapeutic procedures, massage, and the use of orthoses. Hydrogen sulfide baths, the use of ultrasound, novocaine electrophoresis, and paraffin baths have a good effect. Drug treatment consists of taking anti-inflammatory and analgesic drugs during exacerbations.
Wedge-shaped vertebrae
Wedge-shaped vertebrae (or hemivertebrae) are common anomalies of the spinal column. Unlike normal ones, hemivertebrae consist of a semi-arch with a spinous process and a hemibody. This developmental pathology can occur in any part of the spine. Scoliosis develops in children due to wedge-shaped vertebrae. Patients often complain of back pain, poor exercise tolerance, and shortness of breath.
If the wedge-shaped vertebrae are located in the cervical region, headaches occur. Externally, patients have poor posture ranging from minor to severe. With severe curvatures, the chest is deformed, with divergence of the intercostal spaces on one side. Conservative therapy is carried out for mild, non-progressive scoliosis and kyphosis. Patients are prescribed corset mowing, therapeutic exercises, massage, and physiotherapy.
In severe cases, when the functioning of internal organs is disrupted, radical treatment is indicated. The nature of the intervention depends on the severity of the pathology. The following types of operations are performed: posterior spinal fusion (simple or with metal structures), excision of a wedge-shaped vertebra, anteroposterior spinal fusion. In childhood, anteroposterior epiphysiospondylodesis is mainly performed, thanks to which it is possible to stop the growth of the vertebra on the convex side of the curvature.