The load on the human osteoarticular system is colossal throughout life and very often leads to the occurrence of various joint pathologies, which is reflected in detail in the document of the International Classification of Diseases, 10th revision. Traumatologists consider bursopathies of various etiologies to be one of the most common problems of this type, for example, the ICD 10 code for hygroma carries information about its frequent development among all age groups.
This pathology is formed due to long-term load on a particular joint. As a result, a cavity is formed on its surface in the form of a bulge on the skin, filled with liquid.
It is called a benign neoplasm of soft tissue, that is, a cyst of the synovial bursa. The cavity formed due to any inflammatory process in the joint is usually filled with serous fluid mixed with mucus and fibrin.
The M71 section contains all the information about the pathological processes of the mucous membrane of the synovial bursa of the joints (bursopathy).
An exception is bursitis of the big toe (M20.1) and identical pathologies associated with the impact of high pressure on the joint (M70). Hygroma is defined by code M71.3 , which characterizes the causes, pathogenesis, clinical manifestations, treatment methods and prognosis.
The main reasons for the formation of hygroma
- Hereditary predisposition.
- A connective tissue disease that has not been properly treated for a long time.
- Wearing uncomfortable tight shoes for a long time (if we are talking about hygroma on the leg).
- Excess excess weight (due to which the load on the legs increases significantly).
- Injury with subsequent loading of the damaged area (for example, as happens with athletes who often continue training even during the rehabilitation period).
- Unsuccessful attempts to self-medicate arthritis and/or arthrosis.
- The same type of load on the joint, occurring on a regular basis.
The latter applies to those whose work comes down to repeated repetition of monotonous actions day after day. These could be pianists, seamstresses, programmers and people of other essentially similar professions.
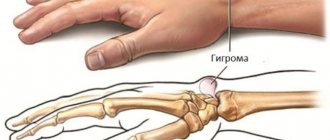
As for the location of the hygroma, it can be any part of the body where there is connective tissue. However, most often the neoplasm occurs in the distal parts of the extremities:
- On the palmar surface of the wrist joint.
- On his own back side.
- On fingers.
- On the ankle or foot.
Features of the disease in children
Hygroma under the knee in a child manifests itself and develops in the same way as in an adult. The difference between the disease detected in young patients is in the reasons for its occurrence. Children whose parents suffer from the disease in question, as well as overly active children, are at high risk of developing diseases.
Up to 40% of detected cysts resolve without the use of surgical methods, with limited sports activities (wait-and-see tactics) and the use of physical therapy.
If the joint hygroma continues to grow, excision of the affected tissue is used (for children under 10 years of age, general anesthesia is administered; for children over this age, local anesthesia is administered).
A Becker cyst can appear during the period of fetal development, in the first 12 months of a baby’s life.
There is practically no relationship between the manifestation of the disease and the presence of diseases in the anamnesis in children.
Characteristic symptoms
The main symptom indicating the formation of a hygroma is a small tumor that is clearly visible under the skin. As a rule, the pathology is localized in isolation, but in rare cases, several tumors may appear in close proximity to each other.
When touching the tumor, the patient feels acute pain. The rest of the time (when the tumor is in a calm state), symptoms may manifest themselves in different ways. Depending on the size of the tumor and its location, this may be:
- Continuous dull pain.
- Unpleasant sensations when a load is applied to the limb.
- Referring pain impulses.
Other symptoms of hygroma include:
- Coarsening and exfoliation of the skin.
- Redness of the affected area.
- Changes in the size of the tumor (increases when moving, decreases when at rest).
Often the pathology does not manifest itself at all until the formation of the hygroma is complete. This is especially true in cases where the tumor is located under the ligaments. Ultimately, pain does appear - either in the process of holding an object with the hand, or in the case when it (the arm) bends.
Complications and consequences
Hygroma is generally not dangerous, as it is a benign neoplasm. Such tumors never become malignant. Moreover, small hygromas that do not increase in size and do not cause discomfort may not even be treated. A daily massage is enough for the hygroma to decrease in size or disappear completely. True, you should consult a doctor about this, since it is not always possible to independently assess the severity of the pathology.
Complications arise when the tumor ruptures and the wound becomes infected. The infection penetrates the joint, causing it to become inflamed. A severe complication of hygroma is a knee abscess, the treatment of which requires urgent surgery.
Related Articles
Hygroma of the ankle joint: photos of symptoms, causes of development and methods of treatment
Wrist hygroma: symptoms, treatment and prevention methods
Folk remedies for the treatment of hygroma: the best recipes
What does hygroma look like in a child and how to treat the tumor
Brain hygroma: causes, symptoms and treatment
Synovitis of the knee joint: causes of development, ICD-10 code, symptoms and treatment
Why is hygroma dangerous?
Patients often postpone visiting a doctor until the hygroma reaches a critical size. And this despite the fact that its presence provokes a number of serious consequences. In the absence of proper timely treatment, a person will face not only pain, but also:
- Purulent tendovaginitis is a disease that disrupts the functioning of the damaged area.
- Paresthesia is a disorder manifested by tingling, burning and numbness.
- Hyperesthesia, in which the affected area becomes much more sensitive to touch.
- Venous stagnation, which in turn can provoke varicose veins, thrombosis and even tissue necrosis.
Often, when trying to self-medicate, people simply puncture the hygroma and let the fluid drain out. Doing this is strictly prohibited, since at this moment you can introduce an infection into the wound. Also, this action will not give the desired results - after some time the hygroma will be restored, and new formations will appear near it.
Prevention of disease development
It is quite simple to prevent the occurrence of the disease; for this you need to carefully monitor the condition of the joints (avoid injuring them), promptly consult a doctor in case of bruises, fractures, and do not self-medicate.
Women are not recommended to wear high heels; athletes - use various bandages, tight elastic bandages that fix the area that is frequently affected; employees of enterprises with hazardous working conditions must undergo medical examination.
Additional preventive measures are:
- weight control;
- eating foods that contain calcium, vitamin B, copper and phosphorus;
- regular testing if there is a history of chronic diseases;
- joint training (moderate sports, gentle physical activity);
- choosing the right shoes, purchasing clothes that do not restrict movement (especially for children);
- optimization of labor associated with long periods of being “on your feet” (if possible);
- alternation of work and rest.
The effectiveness of therapy depends on the time of its initiation. Identification of even minimal discomfort requires contacting a traumatologist for advice. This approach will ensure a complete cure for the disease.
Diagnosis of the disease
If you suspect that you have a hygroma, you need to make an appointment with a doctor. During the consultation, he will perform a visual inspection of the affected area and perform palpation. If this alone is not enough to make a diagnosis, he will refer you to:
- Ultrasound, which will allow you to evaluate the structure of the hygroma - its homogeneity, volume of fluid, etc.
- X-ray, due to which various osteo-articular pathologies are excluded.
- MRI - to exclude the possibility of nodular tumors.
If there is a suspicion that the neoplasm may be malignant, a puncture is taken. And then a histological and cytological examination of the withdrawn fluid is carried out.
What is hygroma and its ICD-10 code
From the International Classification of Diseases, 10th Revision, the lump is defined as “Other bursal cyst”, classified in class XIII, block M70-M79, and coded M71.3.
A hygroma is a cyst, or fluid-filled cavity.
The neoplasm is considered a benign tumor, but this opinion is erroneous: there are no atypical changes in cells in the affected area. The disease should be considered a complication of a number of pathological processes occurring in the human musculoskeletal system.
Treatment methods for hygroma
When the doctor receives confirmation that the patient has a hygroma, and not some other neoplasm, he begins to select a treatment option. Depending on the complexity of the case and the location of the tumor, they may vary. But the following three are considered the most effective and, as a result, the most common:
- Conservative treatment. It involves pumping out fluid from the hygroma and filling the resulting cavity with a specialized sclerasant that glues its walls. To consolidate the result, a fixing bandage is applied to the affected area, which is removed after 3-10 days.
- Minimally invasive method. The hygroma is treated with a laser, which literally “evaporates” its contents, simultaneously “sealing” the edges of the wound. Damaged tissue is cut off. The advantages of this method are a small incision area and a reduction in the recovery period to a couple of days.
- Surgical intervention. It is used when other methods are no longer useful. The hygroma is completely excised using a scalpel, and sutures and a fixing bandage are applied to the treated area. The operation is performed under local anesthesia or general anesthesia.
Recovery period
Rehabilitation after removal of a hygroma takes up to ten days. This formation is not classified as particularly severe, so hospitalization is not required, and the patient can go home immediately after the operation. In the future, he will only have to visit the doctor a couple more times to evaluate how successful the removal of the hygroma was and to remove the stitches (if any were applied). There are no special restrictions on the wound healing period. The only thing is that if the patient does not want to face a relapse or the appearance of new formations, he will need to exclude from his life what leads to their appearance. For example, change jobs, reduce training load, etc.
The medical department has everything you need for safe and low-traumatic removal of hygromas of different locations. Also, with us you can undergo all the necessary tests and studies prior to the main treatment. The clinic's doctors are experts in their field. Make an appointment and you will soon forget about hygroma forever.
Prices
| Code | Name of service | Price |
| 1108 | Removal of benign soft tissue formations up to 3 cm in diameter. | 3000 rub |
| 1109 | Removal of benign soft tissue formations up to 6 cm in diameter. | 4000 rub |
| 1110 | Removal of benign soft tissue formations up to 10 cm in diameter. | 5000 rub |
| 1111 | Removal of benign soft tissue formations from 10 cm to 15 cm in diameter. | 8000 rub. |
| 1112 | Opening abscesses, phlegmon 1st category of complexity | 2500 rub. |