Surprisingly, many patients do not take discomfort in the ankle seriously - they say, it will hurt and it will stop. Meanwhile, pain in the joint, limitation of physical activity and swelling can indicate various, and sometimes very serious, problems.
In this article we will look at when ankle pain can occur in healthy people, which doctor treats ankle pain, and what to do if the ankle hurts. However, first things first.
The ankle joint is a mobile connection between the bones of the lower leg and foot. Anatomically, it consists of the tibia, fibula and talus, enclosed in an articular capsule and surrounded by ligaments. This complex block joint gives us the ability to walk - it is responsible for the movement of the foot in all planes. Rotating your foot and rising on your toes is simply impossible with a sore ankle.
Pain in the ankle joint: causes
Causes of ankle pain
The ankle is characterized by pronounced mobility and strength, but at the same time it is a very vulnerable joint, especially on the outside. Among the factors predisposing to the development of ankle diseases is a high body mass index. For the same reason, joints suffer in pregnant women.
All causes of ankle pain can be divided into 3 large groups:
- Traumatic,
- Infectious (inflammatory),
- Dystrophic-degenerative.
Let's look at each group with an example.
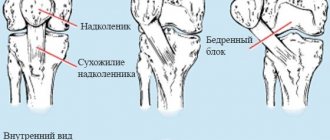
Knee pain: reasons, what to do, which doctor to see
Knee pain: causes, first aid, which doctor to contact
Knee joints
- a very vulnerable part of the body. Pain in this area can be caused by various reasons: injuries, age-related changes, inflammation, autoimmune diseases. Pain in healthy knees usually occurs due to excessive or improper stress caused by training, physical labor, or pathologies in the structure of the spine and feet. For treatment to be effective, it is important to identify the main and additional causes of knee pain, and this is only possible with the help of experienced doctors and a high-quality examination.
How to determine the reason why your knees hurt?
Knee pain can result from:
- diseases of the musculoskeletal system;
- previous lower extremity injuries;
- infectious diseases (if you have been sick in the last 1–3 weeks);
- excessive physical activity;
- hereditary tendency to autoimmune diseases (for example, rheumatoid arthritis).
When contacting a doctor, it is important to mention these factors during the survey. Be sure to check the time of onset of pain. Tell us if the pain appeared for the first time or if your knees hurt periodically. These data will allow you to correctly assume the possible causes of knee pain and prescribe the necessary diagnostic procedures.
Before a medical consultation, you can use a self-examination to determine:
- knee joints or soft tissues hurt;
- whether mobility is impaired;
- what is the color of the skin in the painful area;
- is there any swelling, hematoma, spider veins;
- whether the temperature of the knees has changed relative to other areas;
- Do pain sensations change with palpation and movement?
What symptoms indicate inflammation in knee pain?
Inflammation is accompanied by pain and fever - either only local (in the area of damage) or general.
For inflammation of the knee area:
- gets hot;
- swelling;
- changes color - the skin turns red or blue.
Inflammatory processes in the knee area can develop with the following disorders:
- acute bursitis, synovitis;
- infectious and autoimmune arthritis;
- injuries, including fractures, sprains, cartilage damage.
Inflammation in the knees can be infectious or autoimmune in nature. As a rule, treatment is conservative, but for bursitis and synovitis, minimally invasive surgery is sometimes required to remove excess fluid and pus from the joint cavity. Lack of treatment causes destruction of the knee joints and can lead to complications: a sharp deterioration in mobility, sepsis.
Knee pain in the absence of inflammation and acute injury
The cause of knee pain is not always associated with inflammatory processes. For example, cartilage, natural shock absorbers, can become dehydrated and decrease in size. Because of this, the bones begin to collide with each other, shift and gradually wear out. Often, with age, ligaments lose elasticity, which also leads to deterioration of joint functions.
Why knee pain may occur in the absence of inflammation:
- age-related changes;
- incorrect distribution of load on the legs (due to flat feet, spinal deformities);
- pregnancy;
- excess weight;
- excessive physical activity;
- unbalanced diet, metabolic disorders.
Knee pain can be caused by tumors and cysts, including Baker's cyst, a non-cancerous tumor in the posterior part of the joint.
Which doctor should I consult for knee pain?
As a rule, an orthopedic traumatologist deals with the treatment of knee pain. Doctors specializing in traumatology mainly deal with acute injuries: bruises, fractures, sprains, dislocations. Orthopedic specialists treat chronic and acute deformative, autoimmune and infectious joint pathologies, and help solve problems associated with age-related changes. Less commonly, neurologists, rheumatologists, infectious disease specialists, and surgeons treat knee pain.
To identify the causes of pain you need:
- medical examination;
- blood tests (CBC, biochemical, less often antibody tests);
- hardware studies (X-ray, ultrasound of the joint, MRI).
You should immediately go to the emergency room or call an ambulance if you have the following symptoms:
- extremely rapidly growing swelling or pulsating mass in the knee area;
- increase in body temperature to 39.2 degrees and above;
- confusion, loss of consciousness;
- significant, increasing weakness;
- intoxication;
- sudden drop in pressure.
Without timely medical care, dangerous complications can develop: fat embolism in injuries, sepsis and tissue necrosis in synovitis and bursitis.
What to do if the condition is not urgent:
- take a non-steroidal anti-inflammatory drug;
- remove the load from the sore knee;
- apply anesthetic ointment;
- apply a supporting bandage to the joint;
- do not heat the sore spot, apply cold;
- Make an appointment with a doctor as soon as possible.
The nature of pain in various pathologies, accompanying symptoms
Ankle injuries
The most common type of traumatic ankle injury is a sprain or subluxation of the foot. When walking, running, or jumping, you may step on your foot awkwardly and twist it inward, overstretching the ankle ligaments. The more fibers are damaged, the more severe the nature of the damage and the more pronounced the pain symptoms. In addition to pain, the leg will react with pronounced swelling, and often a bruise appears.
Fractures are less common in this joint. However, jumping or falling from a great height can cause a fracture of the heel bone or ankle. The symptoms are similar to those of a dislocation or sprain, but much more intense. You cannot step on your foot, and when you feel the injured joint, a sharp, unbearable pain occurs. The heel thickens and seems to turn towards the outer surface.
Arthritis of the ankle
The general name for all inflammatory joint lesions is arthritis. Depending on the type of microorganism that causes it, arthritis can be viral or bacterial. When measles, chickenpox or gonorrhea spread throughout the body, it can also affect the joints. A characteristic rash appears around the affected joint, and the skin over it changes color. The patient often complains of aching pain in the ankle, but motor function is preserved. Similar symptoms are characteristic of tuberculous arthritis.
However, if there is intense bursting, throbbing pain in the joint, this may lead the doctor to think about purulent arthritis. With such a reactive course of the disease, general health worsens, fever, chills and a feeling of weakness occur.
Osteoarthrosis (arthrosis) of the ankle joint
Professional athletes who subject their ankles to sprains and hyperextensions over and over again develop degenerative osteoarthritis over time. Due to multiple traumatization of the surfaces of the ankles, fibula and tibia, their surface loses its natural smoothness. Physiological sliding in the joint is disrupted, movements become more and more painful, ankles swell, which even affects the choice of clothing and shoes.
However, not only athletes are susceptible to arthrosis; nowadays, more and more young people complain of pain in the joint after rest, which goes away with movement, as if they need to “disperse”. In the early stages of the disease, joint destruction can be stopped and slowed down.
Other causes of pain
Among other etiological factors of pain in the ankle, experts note flat feet, tendinitis, and a disease with the unusual name “heel spur.” Varicose veins, neoplasms in this area, or osteoporosis can cause similar symptoms. In addition, wearing tight shoes for a long time also causes discomfort in the lower leg.
Ankle pain: diagnosis
Diagnosis of ankle pain
After interviewing the patient, examining the joint, determining the degree of its mobility and swelling, and after gentle palpation of the ankle, the specialist prescribes an x-ray examination. This simple method reliably shows:
- violation of bone integrity, fracture line,
- narrowing or fusion of the joint space,
- osteoporosis (thinning bones),
- osteonecrosis (bone destruction),
- bone osteophytes (protrusions).
If a more detailed diagnosis is necessary, computed tomography (CT) is prescribed. Magnetic resonance imaging (MRI) is used to examine the ligaments, cartilage and other non-osseous elements of the joint. For vascular pathologies, such as varicose veins or thrombophlebitis, it would not be superfluous to perform an ultrasound with Dopplerography. As a rule, a general and biochemical blood test is prescribed, paying special attention to the leukocyte formula and the value of C-reactive protein.
If arthritis or arthrosis is suspected, a joint puncture can be performed, followed by a cytological examination of the resulting fluid.
Which doctor treats ankle pain?
If symptoms similar to those described earlier occur, it is recommended to consult a traumatologist, orthopedist, surgeon or rheumatologist. Doctors of these specialties will conduct an examination, perform the necessary diagnostics and, if indicated, refer you to an endocrinologist, gynecologist or rehabilitation specialist for additional studies.
Medication methods.
The main purpose of nonsteroidal anti-inflammatory drugs (NSAIDs) is to relieve pain and reduce the inflammatory response. They do not affect the speed of the pathological process and do not control it, but they are good at removing accompanying symptoms such as acute pain and local fever. NSAIDs are usually taken as tablets or applied as creams or ointments to the affected area. For severe conditions, the best method of administration is injection directly into the affected joint.
See also: Why is it so important to relieve inflammation?
Treatment of joint pain
Consult a doctor if the joint is cracking, swollen and very painful, or if mild pain occurs more than once. The doctor will examine and palpate, assess joint mobility and refer you for additional examinations: ultrasound, radiography, magnetic resonance imaging, arthroscopy. He may also prescribe tests and consultations with doctors of related specialization.
At an early stage of disease, anti-inflammatory and corticosteroid drugs, antibiotics and supportive care are prescribed. Supportive care includes physical therapy and exercise therapy. If the pain is severe, therapeutic blockades are prescribed - injections of anesthetics and medications into the joint cavity. If the patient cannot sleep due to sore joints, the doctor may prescribe sleeping pills.
In advanced cases, partial or complete joint replacement surgery is performed.
Causes
Joint pain occurs for two reasons - injury or disease. Joints are injured not only by falls and direct blows, but also by intense physical activity, sudden lifting of heavy objects, and prolonged immobility. Some injuries go away on their own if the joint is kept at rest and stress is avoided. But in most cases, injuries become chronic, causing inflammatory processes that lead to the development of diseases.
Diseases that cause joint pain:
- Arthritis
- inflammation of the joints; - Arthrosis
- deformation and limitation of joint mobility; - Bursitis
- inflammation of the joint capsules; - Gout
is the deposition of uric acid salts in the joints; - Neoplasms
- benign and malignant tumors in the joint area; - Autoimmune diseases
are bacterial and viral infections that suppress the functioning of the immune system. Due to disruptions in the immune system, the condition of connective tissues deteriorates.
In most cases, the pain is weak and aching. Acute pain is a symptom of an advanced stage of the disease, in which you should immediately consult a doctor.
Also, be sure to consult a doctor if an old injury hurts: a long-standing bruise, a healed fracture, a healed sprain.
Joint pain rarely occurs on its own. Often, joint diseases have other accompanying symptoms: stiffness of movement, especially after sleeping or sitting in one position, creaking and crunching of joints, swelling and redness.
Arthrosis is not a diagnosis
Therefore, most often, when complaining of joint pain, the patient is given a “universal” diagnosis - arthrosis or cartilage wear. In fact, the clinical manifestations that the patient complains about are not always associated with arthrosis. They can be a manifestation of pathologies of ligaments, tendons, periarticular tissues, injuries or, for example, a meniscal tear in the case of knee joints. Moreover, almost all people over 35-36 years old experience degenerative changes in the joints associated with wear and damage to cartilage. Arthrosis is not a diagnosis. It may accompany arthritis or be a manifestation of systemic diseases. And most importantly, the clinical manifestations that the patient complains about are not always associated with arthrosis.
"Old age" is being treated
However, a person may remain exposed to ineffective therapy for a very long time. He has “arthrosis”, everyone has it and it’s “too early” to go to a rheumatologist. This may be explained by the fact that, as a rule, regional clinics do not have their own rheumatologist specialists, and in regional clinics their appointment is limited by the availability of appropriate quotas or the availability of the corresponding doctors. The patient is simply not referred to a rheumatologist. It is quite difficult to determine the need to see a rheumatologist. Although such cases also occur in practice, when patients themselves “find” their way to a rheumatologist.
The process is delayed, the “therapeutic window” is closing. And at some point, a person, especially in old age, is informed that now it is supposedly “too late” to see a rheumatologist and in general “old age cannot be cured.” It is not true. Even if the therapeutic window has been missed, regardless of age, modern medicine has answers to many challenges. The modern level of medicine makes it possible to improve the quality of life at any age.
When to go to a rheumatologist
In fact, the profile of a rheumatologist is very wide and includes several dozen diseases and pathologies. For example, a predisposition to sore throats and viral diseases may have a rheumatological cause. Of course, there are certain age indicators, but if you are young and rule out the possibility of injury, then the reason to contact a rheumatologist is pain, discomfort, or some changes in the structure or shape of the joints. Especially if all this is accompanied by fever, unexplained weight loss, and changes in blood tests. In this case, the process cannot be delayed. Contact your rheumatologist directly to get into the “therapeutic window.”