Causes of radiculitis Types of radiculitis Symptoms of radiculitis Diagnosis of radiculitis How to treat radiculitis Drug treatment of radiculitis Prevention of radiculitis
Radiculitis is pinching or inflammation of the nerve roots of the spinal cord, which is accompanied by severe pain and rudely interferes with the daily life of patients. This disease always occurs against the background of degenerative changes in the spine, so its symptoms only intensify with age. According to statistics, every 8th person in the world who has reached middle age (over 40 years old) is susceptible to radiculitis, while symptoms of the disease are increasingly observed in urban residents over 30.
Although radiculitis usually does not cause complications, the disease itself can be quite painful and affect the ability to work and the quality of life of patients. Radiculitis pain is caused not only by everyday household activities, but even by prolonged sitting. However, advanced radiculitis still increases the risk of diseases and pathological conditions such as:
- ischemia;
- hemorrhage (infarction) of the spinal cord;
- inflammation of the spinal cord membranes;
- partial paralysis of the limbs;
- atrophic paralysis.
Therefore, it is advisable to begin treatment of the disease at the first symptoms. Which ones? Let's look at it below.
Radiculitis is a lesion of the nerve roots of the spinal cord, which is accompanied by severe pain
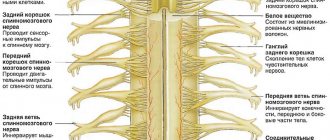
Causes of radiculitis
The main cause of radiculitis is that the elastic intervertebral disc, which performs a shock-absorbing function and maintains a sufficient distance between the vertebrae, begins to receive less nutrients, dries out and cracks. Dehydration and wear of the disc leads to its height decreasing, the vertebrae begin to rub against each other, and osteophytes (bone outgrowths) appear on the edges of the vertebral bones. Because of this, the ridge ceases to be flexible and becomes ossified, and vulnerable nerve roots experience compression and injury.
Radiculitis is usually caused by:
- back injuries, incl. untreated and old;
- postural disorders (lordosis, kyphosis and scoliosis);
- age-related and hormonal changes that reduce the strength of cartilage and bone tissue;
- osteochondrosis and osteoprosis;
- spondylosis deformans;
- protrusion and herniation of intervertebral discs;
- uneven load on the spine;
- hypothermia;
- vibration loads;
- stress and chronic fatigue;
- infectious diseases;
- tumors.
An uncomfortable bed for sleeping or a workplace equipped with poor ergonomics can also provoke symptoms of radiculitis - its development or exacerbation.
The risk group for the disease includes:
- people over 40 years old;
- representatives of professions associated with heavy physical labor (including professional athletes), as well as long stays in one field (especially office workers, truck drivers);
- people suffering from physical inactivity;
- patients with autoimmune diseases;
- men and women with excess weight, bad habits, metabolic diseases.
Types of radiculitis
Radiculitis is usually distinguished by the localization of the inflammatory process. So, they distinguish:
- lumbosacral radiculitis (the most common);
- cervical radiculitis (sometimes cervicobrachial radiculitis is also distinguished, in which pain also occurs in the shoulders and arms, aggravated by movements in the limbs of the upper belt, when turning the head and coughing;
- thoracic radiculitis (less common).
As for the forms of the disease, there are acute and chronic forms. The vast majority of cases of acute radiculitis end with its transition “to chronicle” with periodic exacerbations (if the patient does not comply with the preventive recommendations of the attending physician).
Lumbosacral radiculitis
Lumbosacral radiculitis manifests itself with acute pain in the lumbar region. The pain syndrome intensifies with:
- long walking or sitting;
- bends;
- body turns.
With this disease, patients often complain that they have bent over and are “jammed”; they can only get up with difficulty and through pain. The pain is similar to an electrical discharge that shoots sharply through the sacrum. With radiculitis of the lumbosacral region, 3 characteristic types of pain are observed:
- lumbago is an acute pain that occurs suddenly with sudden, jerky physical activity (for example, when sneezing) and lasts from several minutes to several days. It can also be provoked by a wardrobe that is not suitable for the weather - with overheating, hypothermia of the sacrum, or sitting in a draft, the pain can intensify. Also, a similar type of pain is observed with spastic tension of the lower back muscles (which indicates an imbalance of the load along the spine), displacement of the vertebrae or intervertebral hernia;
- sciatica - shooting, burning or stabbing pain radiates to the sciatic nerve, can respond in the back of the thigh and even the calf muscles, up to the foot. The limbs become noticeably weaker, and muscular dystrophy may occur. A characteristic sign of sciatica is that it can be simultaneously accompanied by tingling and numbness in the area of the affected nerve.
- lumboischialgia is a burning or aching pain, which is characterized by gradual intensification, as well as its localization in the gluteal muscles and the back of the thigh. It does not reach the feet, but can occur in both legs at the same time.
The intensity of any pain varies - from tolerable and rare to unbearable and constant, which prevents the patient from sleeping and moving.
The first symptoms of the disease often appear with sudden weight gain, pregnancy, or unsuccessful lifting of a load.
In a calm state, stage 2 lumbosacral radiculitis can make itself felt by a feeling of numbness, insensitivity of the skin to temperature or physical influence, and tingling in the soft tissues. At the same time, the back muscles weaken, and it becomes increasingly difficult to hold it straight.
The severity of symptoms and treatment of lumbar radiculitis depends on the area of the lesions - inflammation can affect one root or numerous nerve plexuses that are located in the sacral region.
Thoracic radiculitis
Thoracic radiculitis is extremely rare, since due to the ribs and chest, the vertebrae in this part of the spine are not mobile. And therefore, they are less likely to get injured.
Pain from thoracic radiculitis can radiate to the shoulders, arms and even resemble heart spasms. It is accompanied by a feeling of stiffness, especially when trying to take a deep breath. In this case, patients characterize the sensations emanating from the affected nerve as an acute, sharp pain - as if a needle or knitting needle is being driven into the chest and then suddenly pulled out. Often the feeling of pinching in the intercostal spaces is attributed to intercostal neuralgia, missing the onset of radiculitis.
A feature of thoracic radiculitis is the so-called. girdle pains that make patients think about damage to internal organs (heart, liver, pancreas and others). Indeed, deterioration of innervation can affect their work, but the root cause lies in pinched nerve roots.
Thoracic radiculitis often makes itself felt at night, especially when trying to roll over to the other side. They usually affect middle-aged and older people with poor posture.
Cervical Radiculitis is one of the most common types of radiculitis.
Cervical sciatica
Among all cases of radiculitis, cervical radiculitis ranks second in occurrence, second only to lumbar radiculitis. In 95% of cases, the pathology occurs against the background of osteochondrosis of the cervical spine. The peak incidence occurs at the age of 50 years, while every 20th patient eventually loses his ability to work. With cervical radiculitis, a whole complex of symptoms occurs:
- pain in the neck (especially when turning, tilting the head, moving the shoulders) and throughout the upper limbs, including the inner surface of the arm);
- stiffness in the neck, which is especially acute after sleep, a working day, or stress on the neck;
- headaches associated with spasms and deterioration of blood supply to the head;
- hearing and vision impairment, dizziness, coordination problems associated with compression of the vertebral arteries supplying the brain;
- unsteadiness, unsteadiness and uncertainty of gait;
- atrophy of the shoulder muscles
Pain in the back of the head with cervical radiculitis can be observed in people with spinal curvature, physical inactivity and computer work after 25 years. The inflammatory process with cervical radiculitis may be accompanied by deterioration in cognitive functions (it becomes more difficult for patients to understand or remember something). Patients usually find it difficult to find a comfortable sleeping position, so they often suffer from insomnia.
Side effects, contraindications
Gevkamen ointment can provoke the development of allergies, which manifests itself in the form of tingling of the skin, a burning sensation or coldness at the site of application.
The use of this product is contraindicated in the presence of the following disorders:
- individual intolerance to individual components of the drug;
- when the epidermis is damaged in the inflamed area;
- when symptoms of dermatological pathologies appear;
- children under 12 years old.
During pregnancy or lactation, Gevkamen can be used only with the permission of the appropriate specialist and only if the expected beneficial effect from its use exceeds the potential risk to the child or fetus.
Symptoms of radiculitis
For radiculopathy, there are 2 stages, which have different manifestations.
- The neurological stage begins with hyperesthesia (increased sensitivity) in the area of inflamed nerve roots, which is caused by overirritation of the nerve sheaths. If the process is started, there will be sharp pains that will shoot through the spine from time to time. One of the symptoms of sciatica is compensatory muscle tension, which is also called “clamping” or protective tension. To increase the gap between the vertebrae and reduce compression on the roots, patients often take tense, unnatural positions. When palpating the spine, the inflamed areas respond with pain.
- The neurotic stage, on the contrary, makes itself felt by a decrease in sensitivity, up to its complete loss. Pain, muscle tension and other symptoms of radiculitis only increase, causing constant or almost constant discomfort.
Common symptoms of radiculitis are:
- sharp, acute pain when there is a load on the spine or muscle tension (felt in the affected part of the spinal column, but can radiate to organs and limbs);
- paresthesia (persistent or recurrent sensory disturbances caused by pinched nerve roots);
- decreased endurance and muscle atrophy in the affected areas.
In the absence of constant pain, the doctor can identify the symptoms of lumbosacral radiculitis as follows:
- The patient lies on his back and tries to raise his straight leg (Lasegue's symptom).
- The patient stands up straight and moves his straight leg to the side.
- The patient lies on his back, and the doctor presses on the abdomen below the navel.
If there is radiculopathy in such positions, the patient experiences a characteristic symptom of radiculitis - shooting pain.
Symptoms of radiculitis are divided into two stages: neurological and neurotic
Indications
Gevkamen should be used in the presence of the following pathologies:
- different forms of myalgia;
- degenerative lesions of the musculoskeletal system of the body (for example, with arthralgia, deforming osteoarthritis of the spine and peripheral joints);
- tension headache;
- post-traumatic inflammatory reactions affecting joints, tendons, muscles or ligaments (bruise, sprain, overuse, sports injuries);
- various types of neuralgia.
Diagnosis of radiculitis
To diagnose radiculitis and exclude other possible causes of pain, you should consult a neurologist. After an initial examination, an oral interview with the patient and anamnesis, he may prescribe the following laboratory and instrumental tests:
- general and/or biochemical analysis of blood and urine, as well as ultrasound of the pelvis and abdominal region - to exclude diseases of the gallbladder, kidneys, urinary tract, especially pyelonephritis. They have similar symptoms to lumbar radiculitis, but treatment differs.
- electrocardiogram - to differentiate the diagnosis from cardiovascular diseases, in particular, heart attack;
- testing reflexes, sensitivity, mobility and pain, as well as the presence of autonomic disorders using special manual and instrumental tests;
- radiography - helps to determine the curvature of the spine, reduction of the distance between the vertebrae and their wear, and the formation of osteophytes;
- electromyography - to understand whether the passage of a nerve impulse is blocked or slowed down in certain areas, whether the nutrition of the nervous tissue is deteriorated, whether anomalies are observed in the direct and reflex excitability of neurons (this method is effective even in the absence of any symptoms of radiculitis and helps to identify it is still at the first stage);
- MRI - used in cases where radiculitis is the most likely diagnosis, and allows you to determine the degree of nerve compression and the specifics of the lesions;
- CT scan - to accurately determine the causes of radiculopathy and select treatment (allows you to exclude a spinal cord tumor, spondylitis, compression fracture).
How to treat sciatica
Treatment of radiculitis begins with the elimination of pain. At the same time, taking only conventional analgesics is contraindicated for patients - it does not relieve inflammation, but blurs the picture of the disease and complicates its diagnosis. The selection of anti-inflammatory drugs should only be carried out by the attending physician!
Physiotherapy is also selected to restore the trophism of nervous tissue and the conduction of nerve impulses. Patients are also recommended to take vitamin therapy (especially B vitamins), mineral supplements and chondroprotectors. In the first few days, bed rest on a hard bed is advisable, which will help relieve acute symptoms. After eliminating inflammation, you can begin doing therapeutic exercises to relieve compression of the nerve roots.
In the future, patients are recommended to wear orthoses (fixing, limiting, corrective, warming corsets). They help eliminate tension, relax muscles and accelerate the transition of the disease into remission. Corsets should also be worn when exercising, but their constant use can weaken the back muscles. Don't neglect physical therapy. Patients are also recommended to sleep on an orthopedic mattress.
In rare cases, surgical treatment of radiculitis is performed (if medications do not help eliminate persistent pain).
Physiotherapy in the treatment of radiculitis
Physiotherapy plays an important role in the treatment of sciatica at any stage. Some techniques are used exclusively during periods of exacerbation, while others are intended to maintain remission and are carried out in periodic courses.
The most effective types of physical therapy for sciatica include;
- electrophoresis (including pharmacophoresis);
- kinesiotherapy;
- manual therapy and massage;
- acupuncture;
- vacuum therapy (cupping massage);
- ultrasound therapy;
- laser therapy;
- diadynamic therapy;
- ultraviolet irradiation.
All these techniques help alleviate or completely relieve muscle spasms, hypertonicity, inflammation, pain, and restore atrophied muscles. They also improve nerve conduction and blood microcirculation, normalize the biomechanics of the spine, and make it possible to reduce the required volumes of medications.
Therapeutic exercises for radiculitis
Physical therapy is the most effective way to prevent radiculitis and its exacerbations. However, the attending physician or a qualified exercise therapy instructor should determine the level of load and the pace of its increase.
Moderate physical activity helps strengthen the skeletal muscles of the back, so they support the spine in the correct position. This not only reduces the stress caused by upright posture and slows down the wear of the intervertebral discs, but also prevents the displacement of the vertebrae and the formation of a hernia. Also, therapeutic exercises make muscles and ligaments more resilient - which means the risk of spinal injury when performing household duties is reduced.
For radiculitis of any part, traction gymnastics is recommended, which stretches the spine and increases the distance between the vertebral bones. It helps relieve spasms and reduce pinching.
It is especially recommended to perform exercises on special simulators.
For osteochondrosis of the cervical spine:
- Stand up straight with your arms positioned freely along your body. Make a fist and tense your hands, then stretch your neck, lowering your neck and shoulder blades. After 30 seconds, relax and return to your normal position.
- Stand up straight and lean forward so that your body is parallel to the floor. Spread your arms to the sides without raising your shoulders, and try to stretch the back of your head forward. The shoulder blades should be lowered. After this, bring your shoulder blades together and move your straight arms slightly back, working your back muscles.
- Tilt your head back and hold it for 3 seconds, trying to stretch your neck. Repeat - 10 times.
- Clasp your fingers behind the back of your head and stretch, straining your neck and squeezing your shoulder blades. Hold for 3 seconds, repeat 10 times.
- Place your hands on your belt and turn your head first one way, then the other, so that your chin is in line with your shoulder. Hold for 3 seconds, repeat 10 times. You can also give your muscles additional stress by placing your fingers on your temple and applying resistance.
- With your fingers clasped behind the back of your head, tilt your head forward, touching your chin to your chest. After this, raise your head, tensing the muscles at the back of your neck.
For thoracic radiculitis:
- Lie on your stomach and lift your chest off the floor, spreading your straight arms to the sides. Try to move your shoulder blades toward your spine, feeling the tension in your back, not your arms.
- Lie on your back and place a hard roller (or a rolling pin wrapped in a towel) under your back in the area of the thoracic vertebrae. With your hands behind your head, move the roller along your spine, either arching your back or lifting your upper body.
- Sit on the edge of a chair with your shoulder blades or upper back resting on the top of the back of the chair. Bend back, inhaling deeply, and then bend forward while exhaling.
- Wrap the bottom ribs in a towel or other durable cloth. As you exhale, pull the ends of the tissue together, squeezing the air out of your chest, and then inhale as deeply as possible.
- Sit or stand straight, keeping your legs slightly apart. Raise your arms straight above your head and wrap the fingers of your left hand around your right wrist. Tilt your body to the left and stretch your right arm behind you, feeling the tension in your side muscles. Repeat on the other side.
Therapeutic exercises for radiculitis of the lumbosacral region:
- Lie on your back and place your hands under your head. Bend your knees and place your feet on the floor. After this, begin to bend your legs together, first in one direction, then in the other, trying to place the side of your thigh on the floor. At the same time, do not lift your shoulder blades off the floor.
- Stand straight in front of the mirror, relax your limbs. Tighten your buttocks so that the iliac bones of the pelvis move forward, and try to rebuild the spine gradually. In profile, the lower back should be a straight line.
- Standing straight, fix your shoulders and upper body straight and begin to make figure eights with your pelvis, as if performing movements from the eastern pelvis.
- Get on all fours, placing your hips and arms at a 90° angle to the floor. Bend your back, trying to lower your lower back and move the back of your head back. The tension should be felt right down to the neck muscles. After 20 seconds, lift your lower back and arch your back.
Therapeutic exercises are the most effective way to prevent radiculitis and its exacerbations
How to treat radiculitis at home
Many patients use traditional medicine (for example, rubbing with camphor oil) to treat radiculitis at home. However, you cannot rely only on “grandmother’s” methods, and some of them can even worsen the condition! Thus, it is not recommended to apply bags of hot salt, sand, heated stones and warming herbal rubs to the sore spot. When a nerve is pinched, this will only increase swelling in the affected area, and consequently, pinching. If the cause of the pain is not radiculitis, self-warming may be contraindicated! At home, doctors recommend insulating the affected area with clothing and woolen bandages.
In addition to drug treatment and gymnastics, manual rubbing of diseased areas with specialized ointments for radiculitis is allowed at home. To relieve symptoms, pain-relieving herbs are used in the treatment of lumbar radiculitis (calamus, common basil, spotted hemlock, verbena, pine nut, stony stone, sage).
Swimming, contrast showers, air procedures, and sunbathing have a beneficial effect on the course of radiculitis.
Dosage and method of application of the ointment
The medicine is applied to cleansed and dry skin, only if there is no damage to its integrity. The medication is distributed over the surface of the epidermis of the damaged area or at the site of inflammation in an even layer. After applying the ointment, this area should be gently massaged with your hand until the drug is completely absorbed, as evidenced by coldness and a slight burning sensation of the skin. Then it is recommended to wash your hands (of course, if this part of the body does not need treatment).
Gevkamen in adults or children (from 12 years old) is prescribed based on the size of the affected area (organ) from 2 to 4 g of ointment. This is a strip of medication 3-4 cm long, or a volume of medication corresponding to the size of a cherry or walnut. This amount of gel is enough to treat the sacral area or knee joint with an area of 400 to 800 cm2. Application should be repeated 3-4 times a day. The maximum permissible dose of the drug per day is 8 g. Treatment lasts 3-5 days, if desired, the course of therapy can be repeated after 3 days.
Drug treatment of radiculitis
First of all, non-steroidal anti-inflammatory drugs (NSAIDs) and chondroprotectors are used for the medicinal treatment of radiculitis. If NSAIDs are ineffective, they are replaced with glucocorticosteroids (GCs), analogues of hormones produced by the adrenal cortex.
Conventional analgesics can also be used to relieve pain; in severe cases, the attending physician may prescribe lidocaine or another blockade (a local anesthetic is injected into the affected area, where it provides a prolonged effect for 21 days or more).
Nonsteroidal anti-inflammatory drugs
Medicines that have analgesic (analgesic), antipyretic and anti-inflammatory effects.
Glucocorticoids
HA is usually prescribed in the form of injections for radical relief of swelling, inflammation and pain.
Antispasmodics and muscle relaxants
Medicines that reduce the tone of skeletal muscles with a decrease in motor activity up to complete immobility.
Although systemic blood microcirculation correctors can be prescribed for radiculitis, local preparations in the form of ointments and gels are usually used.
Chondroprotectors
Chondroprotectors (glucosamine and chondroitin sulfate preparations) promote the regeneration of cartilage and bone tissue. They slow down degenerative processes in the spine, preventing osteochondrosis, the main cause of radiculitis, from progressing. Regular use of chondroprotectors in courses of 2-6 months can improve the flexibility of the spine, reduce swelling, inflammation and pain. Unlike symptomatic drugs, chondroprotectors, such as Artracam, affect the structural cause of the disease. Due to the almost complete absence of contraindications, these drugs can be used even before the development of the disease, thereby taking care of all joints of the body from a young age.
Pharmacological properties
The therapeutic effect of Gevkamen is due to the action of the plant and chemical components that make up its composition. The ointment affects nerve receptors, increases the lumen of capillaries and arterioles, exhibiting analgesic and distracting properties.
The drug compacts the membranes of skin cells and reduces their exudation. Immediately after applying this product to the affected area, irritation occurs at the site of its application, which is expressed in the appearance of redness, swelling and burning of the epidermis. After 30 minutes, the effect of Gevkamen becomes analgesic and anti-inflammatory in nature. The therapeutic effect of the ointment extends to the deep layers of tissue and muscles.
Prevention of radiculitis
The main role in the prevention of cervical, thoracic and lumbosacral radiculitis is played by therapeutic exercises and the use of chondroprotectors. In addition, doctors recommend:
- avoid hypothermia and drafts, always dress appropriately for the weather;
- watch your posture;
- properly organize the workplace and place to sleep (a hard mattress with a low pillow is desirable);
- Avoid heavy lifting and other excessive physical activity;
- do not forget about warming up at the workplace, especially if it involves staying in one position for a long time;
- stick to 4-5 meals a day;
- drink enough fluid (at least 2-2.5 liters per day);
- promptly treat infectious and colds, injuries, pay attention to chronic metabolic disorders;
- observe safety precautions when forced to lift weights (do not try to lift the load with a jerk, bending over it, but grab it and then stand up with it - this way the load will transfer from the lumbar region to the leg muscles).
To prevent radiculitis, it is useful to include foods rich in fiber, vitamins B and C, and antioxidants in your diet. These include fruits (including dried fruits), vegetables, berries, fatty fish from the northern seas, eggs, dairy products, legumes, and whole grain cereals. You should avoid foods that are harmful to joints, such as: processed foods, carbonated drinks, alcohol, salty, smoked, spicy, sweet foods, fatty meats. Excess coffee can also provoke inflammatory processes.